Published online Oct 10, 2015. doi: 10.5306/wjco.v6.i5.179
Peer-review started: February 8, 2015
First decision: May 14, 2015
Revised: June 8, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: October 10, 2015
Processing time: 248 Days and 0.5 Hours
A 16-year-old man had aswelling over the anterior aspect of the proximal third of the tibia for 1 year, which was peanut size initially and progressively increased to its present size of 10 cm × 8 cm. He underwent fine needle aspiration cytology (FNAC) twice during this period and reported aspindle cell sarcoma. Malignant peripheral nerve sheath tumor (MPNST) is a malignancy of the connective tissue surrounding the nerves. Previously, MPNST was also known as neurofibrosarcoma, malignant schwannoma, andneurogenic sarcoma. We are reporting this case for its rarity and peculiar mode of presentation. FNAC/core biopsy can be used as an effective tool to achievethe correct pathological diagnosis.
Core tip: In cases of malignant peripheral nerve sheath tumor of the tibia, fine needle aspiration cytology/core biopsy can be used as an effective tool to achieve the correct pathological diagnosis. In such cases, en bloc resection is the treatment of choice. Adjuvant radiotherapy/chemotherapy plays a vital role in achieving a good outcome.
- Citation: Rao A, Ingle SB, Rajurkar P, Goyal V, Dokrimare N. Malignant peripheral nerve sheath tumor of proximal third tibia. World J Clin Oncol 2015; 6(5): 179-183
- URL: https://www.wjgnet.com/2218-4333/full/v6/i5/179.htm
- DOI: https://dx.doi.org/10.5306/wjco.v6.i5.179
Malignant peripheral nerve sheath tumors (MPNSTs) are sarcomas originating from cells associated with the nerve sheath. The lifetime risk of MPNST is 0.001% in the general population. As MPNSTs arise from different types of cells associated with nerve sheaths, for example, Schwann cells and fibroblasts, the clinical presentation and histopathological features varies from case to case. So, it is a real challenge to diagnose and classify this rare entity. Generally, a sarcoma originating from a peripheral nerve or a neurofibroma is assumed clinically as MPNST[1,2].
A 16-year-old man was admitted to YCR Hospital Latur, with apeanut-size swelling when it was first noticed,which progressively increased to its present size of 10 cm × 8 cm. Pain was intermittent in the right proximal tibia, with tingling sensationin theright leg for the previous year.
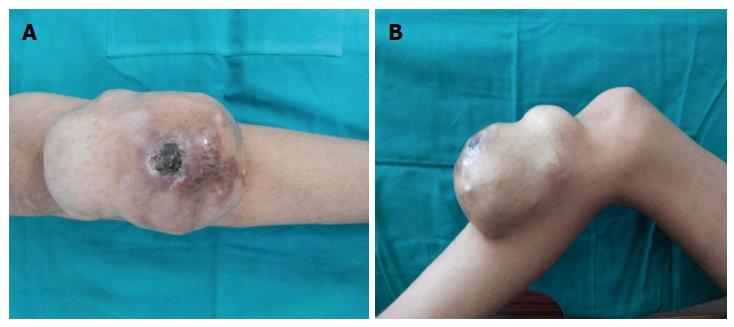
Physical examination revealed a swelling over the anterior aspect of the proximal end of the tibia (10 cm× 8 cm; Figure 1), shiny skin, a scab in the center of swelling, dilated veins over the swelling, and local temperature increase with tenderness. The swelling was mobile and not attached to underlying structures. The range of movements of the right knee joint was full and free, with intact neurovascular status. There was no history of exposure to radiation and no evidence of signs and symptoms of neurofibromatosis (NF) (Figure 2).
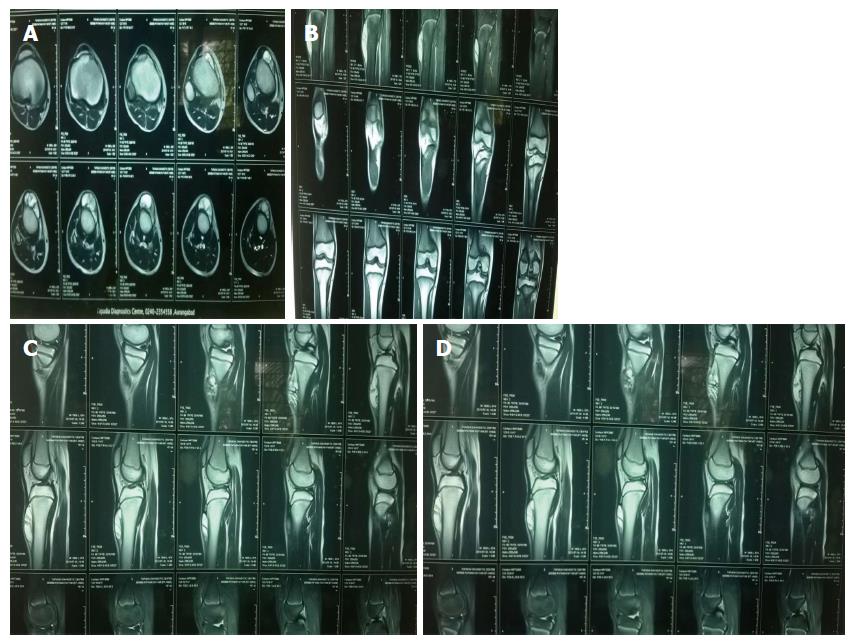
Anteroposterior and lateral radiography of the right knee and tibia showed an expansile soft-tissue mass destroying the adjacent cortex on lateral view, but it did not extendinto the medullary cavity. Congruency of the knee joint was well maintained (Figure 3).
Magnetic resonance imaging showed alobulated mass lesion (7.5 cm × 3.9 cm × 1.6 cm) along the anterior surface of the tibial shaft, which caused periosteal elevation. There was no extension of the lesion within the medullary space of the tibia and no significant bone marrow edema in the adjacent tibia (Figure 4).
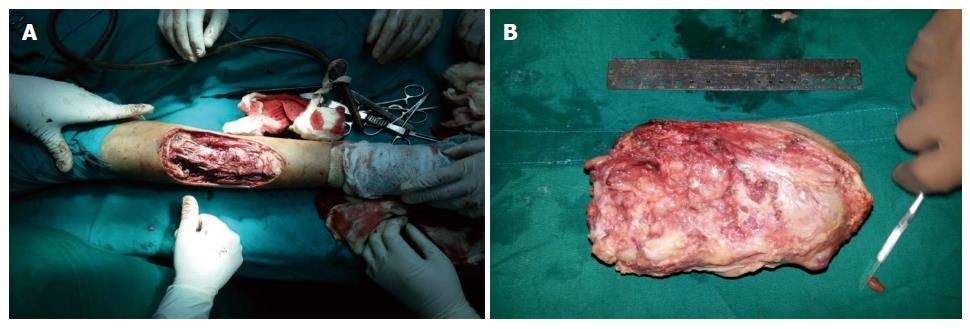
Considering the nature of the growth and high clinical propensity for malignancy, it was treated by en bloc resection and immobilization for 2 wk.
In this procedure, through an antero-medial approach, around 20 cm an elliptical incision of around 20 cm was made and radical en bloc resection of the tumor was performed.
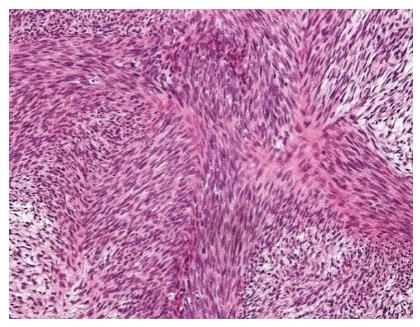
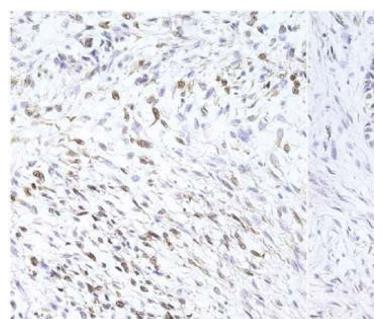
Care was taken to preserve the neurovascular bundle during resection of the tumor from the surrounding soft tissue. The wound was washed thoroughly with H2O2 and the excised mass was sent for histopathological examination. On gross examination, the cut surface was gray-white (Figure 5) and on histopathological examination, the mass was diagnosed as malignant spindle cell sarcoma, i.e., low-grade MPNST (Figure 6). The tumor cells were immunopositive for S-100, thus confirming the final diagnosis of MPNST (Figure 7).
The limb was immobilized in a long/medium knee brace for 2 wk and followed by active knee mobilization. The patient was discharged and advised to attend monthly review. He was also advised to consult an oncologist for chemotherapy/radiotherapy.
MPNSTs constitute 5%-10% of all soft-tissue malignancies. They are associated with NF-1, or may occur independently in a spontaneous manner.
The cause is not known, but they are strongly associated with history of exposure to radiation[3,4]. Fifty percent of the cases occur in patients with NF-1[5-7], and they usually occur in apre-existing neurofibroma.
The genesis ofMPNSTs is associated with genetic mutations in p53 and p16 genes[8-10]. NF-1 gene activity acts as a predisposing factor.
MPNSTs are commonly seen in adults, aged 20-50 years. In the first two decades of life, the incidence is 10%-20%[6], with exceptional casesseen in infants[11].
The plan of treatment for MPNSTs is surgical excision with wide margins. Adjuvant chemotherapy or radiotherapy does not achieve a better outcome[12,13].
It has been clearly stated that these tumors have a tendency to spread for considerable distances along nerves. In such a scenario, frozen sections are advised to ensure clear margins[14].
In a 10-year institutional review, chemotherapy did not seem to reduce mortality, so its effectiveness is questionable. With recent approaches inthe molecular biology of MPNSTs, new therapies and prognostic factors are being examined[15].
A 16-year-old manpresented with apeanut-size swelling, when first noticed, which progressively increased to its present size of 10 cm × 8 cm, and intermittent pain in theright proximal tibia and atingling sensation in theright leg for the past year.
The case was diagnosed as soft tissue sarcoma.
Soft tissue sarcomas, that is, fibrosarcoma, malignant fibrous histiocytoma, and malignant peripheral nerve sheath tumor (MPNST).
On fine needle aspiration cytology (FNAC), the case was diagnosed as spindle cell sarcoma, which was confirmed by histopathology and immunostaining.
X-ray: Anteroposterior and lateral radiography of the right knee and tibia showed an expansile, soft tissue mass destroying adjacent cortex on lateral view, but it didnot extendinto the medullary cavity; congruency of the knee joint waswell maintained. Magnetic resonance imaging showed a lobulated mass lesion (7.5 cm × 3.9 cm × 1.6 cm) along the anterior surface of the tibial shaft, causing periosteal elevation. There was no extension of the lesion within the medullary space of the tibia and no significant bone marrow edema in the adjacent tibia.
MPNST was confirmed by immunohistochemistry.
En bloc resection followed by chemotherapy/radiotherapy.
FNAC/core biopsy can be used as an effective diagnostic tool to achieve early diagnosis.
It is a well written paper describing an interesting case report of MPNST of proximal third tibia treated by en bloc resection.
P- Reviewer: Chin Tan G, Moschovi M S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Adamson DC, Cummings TJ, Friedman AH. Malignant peripheral nerve sheath tumor of the spine after radiation therapy for Hodgkin’s lymphoma. Clin Neuropathol. 2004;23:245-255. [PubMed] |
| 2. | Amin A, Saifuddin A, Flanagan A, Patterson D, Lehovsky J. Radiotherapy-induced malignant peripheral nerve sheath tumor of the cauda equina. Spine (Phila Pa 1976). 2004;29:E506-E509. [PubMed] |
| 3. | Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986;57:2006-2021. [PubMed] |
| 4. | Loree TR, North JH, Werness BA, Nangia R, Mullins AP, Hicks WL. Malignant peripheral nerve sheath tumors of the head and neck: analysis of prognostic factors. Otolaryngol Head Neck Surg. 2000;122:667-672. [PubMed] |
| 5. | D'Agostino AN, Soule EH, Miller RH. Sarcomas of the peripheral nerves and somatic soft tissues associated with multiple neurofibromatosis (von recklinghausen’s disease). Cancer. 1963;16:1015-1027. [PubMed] |
| 6. | King AA, Debaun MR, Riccardi VM, Gutmann DH. Malignant peripheral nerve sheath tumors in neurofibromatosis 1. Am J Med Genet. 2000;93:388-392. [PubMed] |
| 7. | Weiss SW, Folpe AL. Enzinger and Weiss's Soft Tissue Tumors. Edited, St. Louis, Mosby, Inc., 2001. . |
| 8. | Cichowski K, Shih TS, Schmitt E, Santiago S, Reilly K, McLaughlin ME, Bronson RT, Jacks T. Mouse models of tumor development in neurofibromatosis type 1. Science. 1999;286:2172-2176. [PubMed] |
| 9. | Sabah M, Cummins R, Leader M, Kay E. Loss of p16 (INK4A) expression is associated with allelic imbalance/loss of heterozygosity of chromosome 9p21 in microdissected malignant peripheral nerve sheath tumors. Appl Immunohistochem Mol Morphol. 2006;14:97-102. [PubMed] |
| 10. | Vogel KS, Klesse LJ, Velasco-Miguel S, Meyers K, Rushing EJ, Parada LF. Mouse tumor model for neurofibromatosis type 1. Science. 1999;286:2176-2179. [PubMed] |
| 11. | Ellison DA, Corredor-Buchmann J, Parham DM, Jackson RJ. Malignant triton tumor presenting as a rectal mass in an 11-month-old. Pediatr Dev Pathol. 2005;8:235-239. [PubMed] |
| 12. | Cashen DV, Parisien RC, Raskin K, Hornicek FJ, Gebhardt MC, Mankin HJ. Survival data for patients with malignant schwannoma. Clin Orthop Relat Res. 2004;426:69-73. [PubMed] |
| 13. | Leroy K, Dumas V, Martin-Garcia N, Falzone MC, Voisin MC, Wechsler J, Revuz J, Créange A, Levy E, Lantieri L. Malignant peripheral nerve sheath tumors associated with neurofibromatosis type 1: a clinicopathologic and molecular study of 17 patients. Arch Dermatol. 2001;137:908-913. [PubMed] |
| 14. | Levi AD, Ross AL, Cuartas E, Qadir R, Temple HT. The surgical management of symptomatic peripheral nerve sheath tumors. Neurosurgery. 2010;66:833-840. [PubMed] |
| 15. | Neville H, Corpron C, Blakely ML, Andrassy R. Pediatric neurofibrosarcoma. J Pediatr Surg. 2003;38:343-346; discussion 343-346. [PubMed] |