INTRODUCTION
Gastric cancer with peritoneal carcinomatosis (PC) presents a major clinical challenge due to its poor prognosis and high lethality. Diagnosis at an advanced stage often limits treatment options and leads to dismal survival rates. The reported incidence of synchronous metastases ranges from 10% to 40%, paralleling the incidence of metachronous metastases, which ranges from 23% to 38%[1,2]. Risk factors for synchronous PC include younger age, non-cardia gastric tumors, female sex, signet ring cell carcinoma, diffuse histology, T4 stage, Hispanic ethnicity, and multiple metastatic sites[3]. After curative gastrectomy, an R1 resection or positive cytology is associated with a higher risk of peritoneal recurrence[4]. Median survival among patients who receive only best supportive care is typically 2-4 months[5,6]. Advances in surgical techniques and systemic therapies guided by patient biomarkers have significantly extended survival, with median overall survival now reaching 13.1-18.2 months[7,8]. These developments underscore the urgent need for more effective treatment strategies to optimize outcomes for this vulnerable patient population.
Currently, the main treatment modality for PC is systemic therapy[9,10]. However, various surgical interventions are emerging as alternatives or adjuncts to standard systemic therapy. For patients with extensive PC, either intraperitoneal chemotherapy (IP) or pressurized intraperitoneal aerosolized chemotherapy can be used to mitigate symptoms and prolong survival in palliative settings[11,12]. Both techniques are minimally invasive and associated with low morbidity. In IP, systemic chemotherapy is administered alongside intraperitoneal paclitaxel, which is favored for its concentration-dependent cytotoxicity and pharmacokinetic advantages[13]. Approximately 2.7% of patients who receive IP eventually undergo conversion surgery with curative intent[14]. Three-year overall survival rates as high as 21.9% have been reported with IP[15]. Pressurized intraperitoneal aerosolized chemotherapy offers both therapeutic benefits and an opportunity to reassess the peritoneal cavity via laparoscopy to gauge treatment response. Platinum-based agents or doxorubicin are delivered into the abdominal cavity through a nebulizer under pressure. Median survival times of 13-19.6 months have been described with pressurized intraperitoneal aerosolized chemotherapy, and up to 26% of patients may proceed to curative surgery[16,17].
In contrast, cytoreductive surgery (CRS) with hyperthermic IP (HIPEC) is feasible as a curative option for patients with limited PC. According to the GYMSSA trial, gastrectomy combined with CRS and HIPEC significantly improves median survival compared with systemic chemotherapy alone[18]. This procedure involves standard radical gastrectomy with lymphadenectomy, removal of peritoneal nodules, and administration of chemotherapy at elevated temperatures directly into the peritoneal cavity. The optimal temperature enhances chemotherapy efficacy and facilitates deeper tissue penetration. Achieving a low peritoneal cancer index (PCI) and complete cytoreduction is crucial for improved survival. A multi-institutional cohort study from the Peritoneal Surface Oncology Group International reported a median overall survival of up to 11 years[19]. Additionally, a 3-year disease-free survival rate of 21.7% has been documented in selected patients with PCI < 7[20]. However, this procedure carries significant morbidity due to its extensive surgical scope. Operative time and blood loss can be double those observed in standard gastrectomy with D2 Lymphadenectomy[21]. Although overall complications may not increase, higher postoperative renal dysfunction has been reported[22].
Kehlet[23] first introduced the multimodal approach for reducing postoperative pathophysiology and improving perioperative care. This concept led to the formation of the Enhanced Recovery After Surgery Society, which emphasizes minimizing surgical stress and accelerating recovery through a multidisciplinary framework. Enhanced recovery after surgery (ERAS) principles has since been applied across surgical disciplines with promising outcomes[24,25]. In 2014, the Society released consensus guidelines for gastrectomy, followed by guidelines for CRS with or without HIPEC in 2020. These protocols aim to optimize postoperative recovery and reduce complications. Adherence to ERAS principles can facilitate earlier restoration of gastrointestinal function and shorten hospital stays[26]. Such benefits are particularly important in cancer surgery, where prolonged recovery may delay systemic therapy.
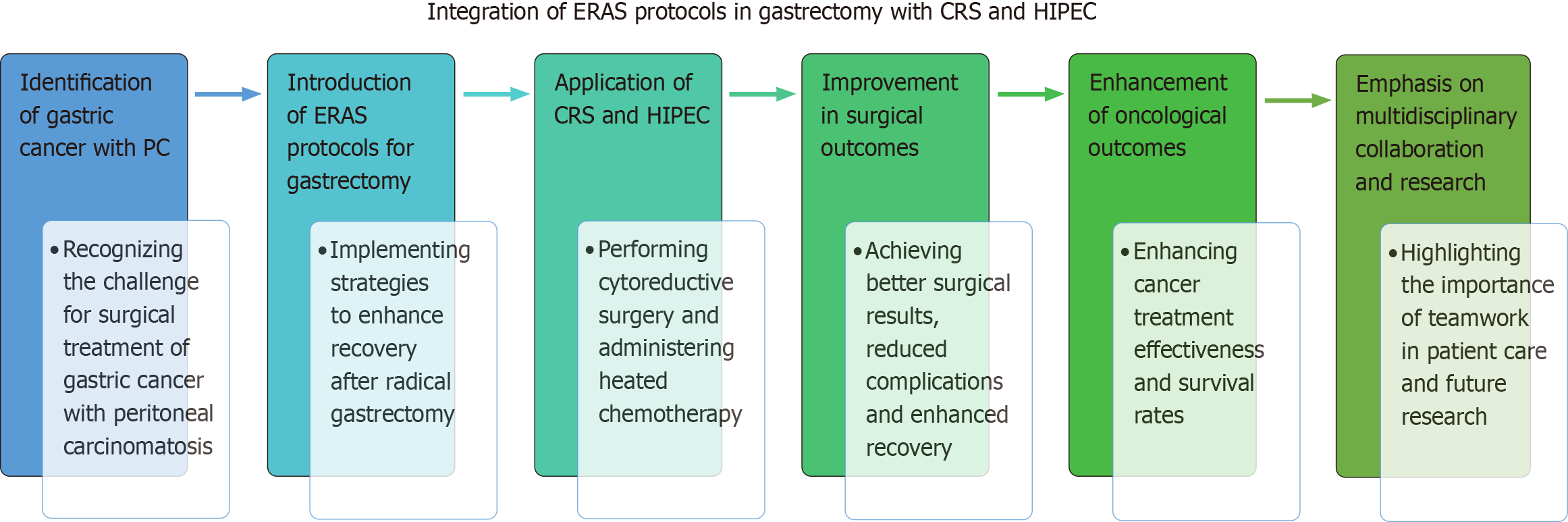
This minireview focuses on integrating ERAS protocols into gastrectomy with CRS and HIPEC, highlighting potential benefits for both surgical and oncological outcomes. We searched PubMed and Google Scholar for all studies evaluating ERAS implementation in gastrectomy and/or CRS with HIPEC and included relevant data on gastric cancer and peritoneal metastasis. This minireview therefore moves beyond a simple compilation of existing data. Instead, it provides a concise synthesis of current evidence and highlights the practical challenges of applying ERAS to complex procedures such as gastrectomy combined with CRS and HIPEC.
PATHOPHYSIOLOGY AND DIAGNOSIS OF PC
The peritoneum is a serous membrane formed by mesothelial cells that line the abdominal cavity and envelop visceral organs, playing a key role in various physiological processes. The membrane consists of 2 Layers: (1) The parietal peritoneum, which attaches to the abdominal and pelvic walls; and (2) The visceral peritoneum, which encloses the internal organs. A critical component of peritoneal function is the blood-peritoneal (peritoneal-plasma) barrier, which regulates substance exchange between the peritoneal cavity and the bloodstream. This barrier also plays an important role in medical applications, including peritoneal dialysis and IP.
Several mechanisms have been proposed to explain the pathogenesis of PC. In gastric cancer, a common route is direct dissemination from the primary tumor after tumor cell exfoliation. This typically occurs in tumors with serosal involvement, spontaneous perforation, or tumor spillage during surgical resection. Loss of E-cadherin is strongly linked to tumor cell detachment through the epithelial-mesenchymal transition pathway[27,28]. Once detached, tumor cells often seed the peritoneal cavity passively, driven by gravity and negative diaphragmatic pressure. They tend to migrate into the pelvis, follow the right paracolic gutter, and reach the subdiaphragmatic spaces and small bowel mesentery via transmesothelial or translymphatic routes[29].
Diagnosing gastric cancer with PC typically involves multiple imaging modalities, including computed tomography, magnetic resonance imaging, and positron emission tomography. Computed tomography imaging is the cornerstone for initial assessment, owing to its availability, cost-effectiveness, and short examination time. However, small peritoneal nodules can be overlooked, and distinguishing PC from other conditions remains challenging. Magnetic resonance imaging offers slightly higher sensitivity, especially for subdiaphragmatic lesions, but involves greater expense and longer study times. Positron emission tomography/computed tomography is frequently recommended to detect relapse after treatment due to its high specificity[30]. The commonly used radiotracer, 18F-fluorodeoxyglucose, may be less effective for diffuse-type gastric cancer, resulting in non-avid lesions. As imaging techniques evolve, newer radiotracers such as 18F-fluothymidine and 68Ga-Ga-FAPI-04 show potential for improving PC detection[31,32]. Still, staging laparoscopy remains the most effective tool for diagnosing PC[33]. It enables direct visualization of the abdominal cavity and precise scoring of peritoneal nodules using the PCI. Moreover, cytology can reveal occult PC when no gross peritoneal involvement is evident[34,35].
CURRENT ROLES OF GASTRECTOMY WITH CRS AND HIPEC
After comprehensive staging, gastrectomy with CRS and HIPEC can be performed with prophylactic, adjuvant, or palliative intent, depending on the extent of PC. A previous randomized, case-control study showed improved survival by adding HIPEC with cisplatin to standard D2 gastrectomy for tumors classified as ≥ T3 without PC. The 3-year disease-free survival rate was significantly higher in the HIPEC group (93% vs 65%, P = 0.0054), with no significant differences in biochemical parameters between groups[36].
For patients with limited PC, systemic therapy is offered as primary treatment instead of upfront surgery. Biomarkers such as human epidermal growth factor receptor 2, mismatch repair, programmed death-ligand 1, and claudin 18.2 help guide therapy selection. Patients who achieve a favorable clinical response may become candidates for conversion surgery, defined as an operation aiming for R0 resection after systemic therapy in otherwise unresectable disease. Yoshida et al[37] proposed 4 categories of stage IV gastric cancer based on the presence of macroscopic peritoneal dissemination and other organ metastases. Categories 1 and 2 Lack macroscopic peritoneal dissemination, whereas categories 3 and 4 present with gross peritoneal spread. Gastrectomy with CRS and HIPEC may be curative for category 1 patients who have CY1 disease following neoadjuvant treatment. It may also benefit category 3 patients who achieve complete or partial clinical response, have negative cytology, and are technically resectable. Median survival times for P1 and P0CY1 patients who underwent R0 resection were 41.8 (33.8-49.7) months and 42.4 (34.7-not reached) months, respectively[38].
The operative procedure typically begins with a standard gastrectomy and D2 Lymphadenectomy. The extent of gastric resection depends on the primary tumor’s location and ensuring sufficient proximal margins for each macroscopic type. All visible peritoneal nodules must then be removed. This peritonectomy step is technically demanding, requiring a highly skilled surgeon to handle peritoneal tissue carefully, minimize blood loss, and reduce operative time. The decision to perform peritonectomy depends on the extent of peritoneal involvement. According to Sugarbaker’s original technique, only diseased peritoneal areas are excised, while unaffected regions are preserved. However, a pathological analysis of total parietal peritonectomy revealed microscopic residual disease in about 23% of normal-appearing peritoneum in ovarian cancer[39]. Studies in colorectal cancer have shown superior survival with total parietal peritonectomy despite no visible peritoneal involvement, although this approach increases blood loss, prolongs operative time, and carries an overall morbidity of up to 32.3%[40,41]. Evidence comparing total and selective peritonectomy in gastric cancer remains limited.
Extensive intraoperative peritoneal lavage with normal saline is optional and not routinely performed. Two meta-analyses reported conflicting results regarding postoperative complications and recurrence survival with extensive intraoperative peritoneal lavage[42,43]. The final step involves administering chemotherapy in a heated environment at 42-43 °C for 60-120 minutes. Hyperthermia exerts antitumor effects by inducing protein denaturation and impairing DNA repair, potentially increasing chemotherapy penetration without causing significant systemic toxicity. No consensus exists on a standard IP regimen, although agents such as mitomycin-C, cisplatin, paclitaxel, docetaxel, and oxaliplatin have been used[44]. Mitomycin-C combined with cisplatin demonstrated superior 3-year overall survival (13.6% vs 0%) and 3-year metastatic-free survival (13.3% vs 0%) compared with CRS alone[45]. Patients with moderately differentiated tumors, CY1 without gross peritoneal nodules, and low PCI scores are more likely to achieve overall survival ≥ 36 months[46]. Those with higher pathological T and N stages often survive less than 36 months[46]. Other favorable prognostic factors include PCI < 7, complete cytoreduction, and absence of signet ring cells[20,47,48]. In advanced cases with severe recurrent ascites, palliative HIPEC may alleviate symptoms, although it rarely extends survival[49,50].
The ongoing, multicenter GASTRICHIP trial is a phase III study that began recruiting participants in 2014. It compares 5-year survival between standard gastrectomy alone and gastrectomy combined with oxaliplatin-based HIPEC for locally advanced gastric cancer, including CY1 cases[51]. The estimated completion date for this study is May 2026. Another phase III randomized controlled trial, PERISCOPE II, began recruiting in 2017 to compare CRS with HIPEC vs palliative chemotherapy in patients with a PCI < 7 or CY1. The experimental arm involves 30 minutes of hyperthermic oxaliplatin and 90 minutes of normothermic docetaxel. Its primary objective is to compare overall survival, with final results anticipated in 2026[52,53]. These 2 trials may substantially influence future clinical practice in this field.
ERAS IN GASTRECTOMY WITH CRS AND HIPEC: CORE COMPONENTS
As gastrectomy combined with CRS and HIPEC is often performed in stage IV patients, preoperative declines in performance status and nutritional status are common. Many of these patients also require further systemic therapy after surgery. Because multiple major surgical steps are combined with cytotoxic drug administration, the risk of complications is high. An analysis of the ACS-NSQIP registry comparing CRS and HIPEC with vs without gastrectomy (with 44.2% of gastric cancer cases in the gastrectomy arm) found higher intraoperative transfusion requirements and longer operative times in the gastrectomy group. Postoperative sepsis, deep surgical site infection, prolonged ventilation (> 48 hours), pneumonia, and cardiac arrest were more frequent, resulting in overall morbidity rates of 60.5% vs 27.9%. Hospital stays were 8 days longer in the gastrectomy group, although mortality did not differ significantly[54]. Incorporating HIPEC into gastrectomy with CRS also increases postoperative complications and length of stay[55].
Although the peritoneal-plasma barrier reduces systemic toxicity, IP can still cause adverse effects. Cisplatin frequently causes nephrotoxicity, mitomycin-C is associated with postoperative neutropenia, and oxaliplatin is linked with postoperative bleeding. Other possible adverse events include electrolyte abnormalities, hematological toxicity, and pulmonary complications[56]. Consequently, perioperative care is crucial for minimizing morbidity. Successful application of ERAS protocols to gastrectomy with CRS and HIPEC requires an understanding of both procedures’ guidelines. The fundamental concept emphasizes a multimodal perioperative approach that encompasses preoperative optimization, intraoperative management, and postoperative recovery. While certain ERAS components are common across procedures, protocol adaptations may be necessary to address procedure-specific demands.
Preoperative phase
During the preoperative phase, both ERAS protocols emphasize patient education, nutritional optimization, and multimodal analgesia to support postoperative recovery[57,58]. Patient counseling can reduce fear and anxiety, improve pain control, and increase satisfaction. Abstinence from alcohol and smoking for at least 1 month is recommended to minimize complications. Alcohol prolongs bleeding time and may increase cardiac events or arrhythmias, but these issues are reversible after cessation. Smoking impairs oxygen binding and weakens immunity, potentially increasing infection and anastomotic leakage risk[59]. Nicotine replacement therapy is a safe option for preoperative smoking cessation[60]. Nutritional assessment is advised, particularly in malnourished patients who benefit from nutritional and protein supplementation (1.2 g/kg/day) for at least 5 days, and up to 14 days if severely malnourished. Immunonutrition (e.g., arginine, glutamine, omega-3 fatty acids, nucleotides) has not shown routine benefit in gastrectomy. Oral intake is preferred, followed by enteral feeding via tube if needed, and parenteral nutrition as a last resort to avoid mucosal atrophy[61].
Prolonged fasting increases stress, discomfort, and insulin resistance. Hence, studies recommend a shorter fasting period before surgery, allowing solid food until 6 hours and clear fluids until 2 hours before induction. A meta-analysis demonstrated that a carbohydrate drink before surgery shortens hospital stay and reduces insulin resistance without raising complication rates in major abdominal surgery[62].
Additionally, according to ERAS guidelines for abdominal and pelvic surgery in low-middle-income countries, 50 g of carbohydrate with an osmolality < 300 mOsm/kg should be given 2 hours before surgery[63]. The ESPEN guideline also supports administering 800 mL of carbohydrate drink at night and 400 mL 2 hours before surgery, although caution is advised in poorly controlled diabetes and in gastric outlet obstruction[64].
Moreover, mechanical bowel preparation is unnecessary unless rectal resection is planned. Oral antibiotic decontamination may reduce surgical site infection and anastomotic leakage risk in CRS, although evidence is indirect. Postoperative nausea and vomiting is common. Its likelihood can be predicted by the Apfel score, which considers sex, smoking status, history of motion sickness or postoperative nausea and vomiting, and postoperative opioid use[65].
Furthermore, the gastrectomy guideline suggests risk-based antiemetic prophylaxis, whereas the CRS guideline advises at least 2 antiemetic drugs plus total intravenous anesthesia. Preanesthetic medication should include multimodal analgesia and short-acting anxiolytics, with oral celecoxib, pregabalin, and tramadol recommended to reduce opioid use[57]. Given the 30%-50% risk of venous thromboembolism, mechanical prophylaxis and pharmacologic therapy starting 12 hours before CRS and continuing 4 weeks postoperatively are mandatory[58].
The CRS guideline also highlights comprehensive preanesthetic evaluation due to the procedure’s complexity. Core assessments include cardiac evaluation using the Revised Cardiac Risk Index and the American College of Surgeons National Surgical Quality Improvement Program surgical risk calculator. Screening for obstructive sleep apnea in ascites patients with the STOP-BANG questionnaire, laboratory testing, and frailty screening are also recommended[57]. Preoperative anemia is associated with increased postoperative cardiac events, underscoring the need to evaluate hemoglobin at least 30 days before surgery. Potential causes of anemia include blood loss from gastric cancer or comorbid conditions such as renal disease. Correctable causes should be treated, and hemoglobin levels optimized[57]. Additionally, prehabilitation programs that incorporate physical exercise can improve fitness and reduce anxiety, aiding perioperative outcomes[66].
Intraoperative phase
Intraoperative elements from both ERAS guidelines are generally comparable, particularly in preventing surgical site infections. The operative field is often clean-contaminated or contaminated due to potential bowel resection, and reported surgical site infection rates range from 20% to 25%[67,68]. Adhering to Centers for Disease Control and Prevention recommendations, patients should bathe with soap the night before surgery, receive alcohol-based skin preparation, and be given antimicrobial prophylaxis 1 hour before incision[69]. If the antibiotic has a short half-life, an additional dose is given every 3 or 4 hours. Cephalosporins are preferred, with metronidazole added for bowel resection. Continuous thoracic epidural analgesia (T5-T11) using local anesthetics and short-acting opioids is routinely recommended for at least 72 hours postoperatively. Gastrectomy guidelines also accept patient-controlled analgesia or intravenous lidocaine as alternatives, while the CRS guideline promotes multimodal analgesia[58]. Short-acting induction agents, opioids, and muscle relaxants are preferred, and rapid sequence intubation may be necessary if aspiration risk is elevated. Both volatile-based anesthesia and total intravenous anesthesia are acceptable, with depth titrated using bispectral index.
Careful fluid management is crucial due to physiological changes during CRS and vasodilation from hyperthermia in the HIPEC phase. Goal-directed therapy with central venous pressure and cardiac index monitoring helps maintain adequate urine output (> 1 mL/kg/hour) and near-zero fluid balance[58]. Balanced crystalloids are typically used, and blood transfusions are selectively administered to keep hemoglobin near 8 g/dL. Tranexamic acid, cryoprecipitate, and fresh frozen plasma may be added as needed to manage bleeding. An arterial line is beneficial for real-time blood pressure control and frequent blood gas analysis. Normothermia should be preserved using forced-air warming or warming mattresses to avoid serious complications associated with hypothermia (< 36 °C) such as cardiac events, coagulopathy, wound infection, shivering, and prolonged hospitalization[70]. During HIPEC, body temperature should be maintained between 36 °C and 41 °C to prevent excessive hypermetabolism. Glycemic control within 140-180 mg/dL is also recommended to reduce perioperative morbidity.
Minimally invasive gastrectomy techniques have gained traction, showing lower complication rates and improved recovery for laparoscopic distal gastrectomy, especially in T1 gastric cancer. Data remain limited for locally advanced lesions, and laparoscopic total gastrectomy poses technical challenges related to complex anastomoses. Robotic gastrectomy is not yet discussed in ERAS guidelines, and further research is needed. Routine nasogastric or nasojejunal tubes are discouraged unless delayed gastric emptying is expected, as they may slow bowel function and increase patient discomfort[71]. Drains are also not mandatory for all gastrectomies, given minimal differences in wound infection, intraabdominal abscess, or intestinal recovery outcomes. Still, prophylactic thoracic drains may be placed after diaphragmatic peritonectomy to prevent pleural effusions or pneumothorax. After completing the operation, early extubation should be attempted if no contraindications exist.
Postoperative phase
Urinary catheters should ideally be removed by postoperative day (POD) 3, irrespective of epidural catheter removal. Adequate pain control remains vital after the epidural is discontinued, and multimodal analgesia with acetaminophen, nonsteroidal anti-inflammatory drugs, and opioids is recommended. Early mobilization can begin on POD 1, supported by a structured rehabilitation program to enhance bowel recovery. Extensive abdominal exploration in CRS and HIPEC can increase the risk of postoperative ileus. Preventive measures include epidural analgesia or transverse abdominis plane blocks, careful fluid balance, chewing gum, coffee, oral laxatives, and prokinetic agents. Both guidelines endorse initiating a clear liquid diet on POD 1 to minimize complications, with oral nutritional supplements added to achieve a daily protein intake of 2-3 g/kg/day by POD 5. Enteral or parenteral nutrition may be initiated preemptively in select cases.
In addition, systematic audit by a multidisciplinary team is crucial for maintaining ERAS compliance and improving outcomes. All ERAS items should be listed and assessed for every patient; completion rates and encountered obstacles must be recorded. According to the ERAS society, an interactive online audit platform is available to monitor adherence, promote integration of ERAS pathways, maintain quality control in clinical practice, and facilitate future research.
Special considerations for HIPEC
The CRS guideline highlights the importance of appropriate chemotherapy timing and dose. Systemic chemotherapy should generally be discontinued at least 3 weeks before surgery. Cisplatin-induced nephrotoxicity can be significant, especially at doses exceeding 240 mg. Intravascular volume optimization and avoidance of nephrotoxic agents are critical for renal protection. Intravenous sodium thiosulfate may also mitigate cisplatin-related nephrotoxicity[72]. High-dose mitomycin-C (over 40 mg) can cause severe myelosuppression, which can be managed with granulocyte colony-stimulating factor if needed, although routine prophylaxis is not recommended.
ADVANTAGES OF ERAS PROTOCOL
Adaptation of ERAS for vulnerable patients
A significant proportion of gastric-cancer patients with PC are elderly or exhibit low functional status, complicating both surgical recovery and long-term outcomes. For these individuals, ERAS pathways should be carefully adapted. Prehabilitation programs that combine light physical activity, breathing exercises, and basic psychological support can strengthen physical reserve before major surgery. Malnutrition and sarcopenia are common in this population; therefore, early recognition, high-protein diets or supplements, and prompt referral to a dietitian can improve resilience. Patients who show limited improvement after neoadjuvant therapy-or who have borderline performance status yet proceed to CRS-HIPEC-face a tangible risk of delaying subsequent systemic treatment. In such cases, ERAS elements can shorten recovery, minimize postoperative complications, and enable earlier resumption of adjuvant therapy. Although ERAS benefits frail patients, each protocol component should be individualized to match the patient’s capacity and clinical condition.
Surgical aspect
ERAS protocols confer distinct physiological advantages by optimizing postoperative recovery and minimizing complications. Early oral nutrition expedites gastrointestinal function, reduces postoperative ileus, and promotes quicker bowel movements. Limiting opioid use and encouraging early mobilization preserve muscle strength, enhance respiratory function, and lessen the risk of pneumonia. In CRS, which involves extensive tissue manipulation, ERAS strategies regulate fluid administration and pain management, preventing fluid overload, cardiovascular instability, and electrolyte imbalances. Early ambulation improves circulation and decreases venous thromboembolism risk. Collectively, these measures reduce surgical stress, bolster organ function, and curtail postoperative morbidity, ultimately supporting swifter and more robust recovery for patients.
Evidence in gastrectomy
Robust ERAS data for combined gastrectomy with CRS and HIPEC remain limited, but separate studies on gastrectomy or CRS have shown consistent improvements in early postoperative outcomes. One Western cohort reported decreased mortality and shorter hospital stays in the ERAS group, with comparable complication and readmission rates[73]. Another retrospective cohort found earlier oral intake and faster time to defecation without increasing complications[74]. A Chinese propensity score-matched analysis further revealed quicker restoration of intestinal function and ambulation, fewer postoperative complications, reduced length of stay, and lower treatment costs[24].
Two European cost-analysis studies also demonstrated significant reductions in total perioperative expenditures after ERAS implementation. Common sources of savings included laboratory tests, imaging, intensive-care utilization, anesthesia and operating-room services, physiotherapy, and blood transfusions, whereas higher costs were noted for disposable materials and dietitian services[73,75]. The GISSG1901 multicenter randomized controlled trial on ERAS for laparoscopic distal gastrectomy reported similar benefits, including a shorter interval before initiating adjuvant chemotherapy[76]. A meta-analysis of 17 randomized controlled trials confirmed faster gastrointestinal recovery, fewer overall complications, shorter hospitalization, and reduced costs in the ERAS arm; the meta-analysist also found significantly better postoperative C-reactive protein, albumin, and interleukin-6 Levels[77].
Evidence in CRS and HIPEC
Most ERAS studies on CRS and HIPEC focus on ovarian cancer, although some involve mixed origins. One retrospective series demonstrated reduced intraoperative and postoperative fluid requirements and shorter hospital stays in both open and laparoscopic HIPEC procedures[25]. Epidural analgesia decreased intravenous opioid use, enabling earlier ambulation and diet resumption[78]. Hyperglycemic episodes were fewer, and epidural catheters were often removed before POD 5, allowing transition to oral analgesics[79]. A meta-analysis comparing CRS with and without HIPEC also showed reduced hospital stays and major postoperative complications[80].
By contrast, cost-saving effects remain inconclusive; no definitive evidence confirms an overall reduction in expenses. A propensity-score-matched analysis even showed significantly higher total charges after ERAS implementation and called for further modification of specific components to tailor the protocol to individual patients[81]. Despite the complexity and invasiveness of CRS and HIPEC, existing ERAS implementations have yielded satisfactory outcomes, reinforcing the protocol’s potential benefits in this challenging clinical setting.
Oncological aspect
ERAS holds potential for improving long-term outcomes by reducing surgical stress, complications, and recovery time. Early mobilization, optimal pain management, and targeted nutritional support decrease infection risk and hospital stays, enabling timely adjuvant treatment. Standardized, evidence-based perioperative care supports better physical and functional recovery while reducing malnutrition, thromboembolic events, and postoperative ileus-factors that can undermine survival. ERAS also modulates the immune response by limiting postoperative immune suppression linked to major surgery. Although the direct impact on survival requires further study, one retrospective review reported significantly improved 5-year overall and cancer-specific survival in laparoscopic gastrectomy, particularly for stage III disease[24]. Another ongoing randomized controlled trial, recruiting since 2020, aims to compare ERAS with conventional care in laparoscopic distal gastrectomy, focusing on 3-year overall survival and disease-free survival[82].
The recognized surgical and oncological benefits of ERAS-enhanced recovery, immune modulation, and better tolerance of adjuvant treatments-underscore the necessity of continued protocol integration and optimization. Challenges remain in refining ERAS for maximum patient benefit, especially in the context of gastrectomy combined with CRS and HIPEC. Future investigations are essential to validate and expand its advantages for these complex procedures.
CHALLENGES
ERAS protocols have reshaped perioperative care, yet their full potential remains underutilized because adoption is difficult in vulnerable patients. After CRS with HIPEC, prolonged operating time, extensive peritoneal dissection, and hyperthermic chemotherapy create substantial third-space fluid loss and vasodilation. Precise fluid management is therefore critical: Both under-resuscitation and over-resuscitation carry significant risks, ranging from acute kidney injury to pulmonary or tissue edema that can jeopardize anastomotic healing. In addition, chemotherapeutic agents compound postoperative immunosuppression; coupled with surgical stress, this heightens infection risk and can delay wound healing, undermining early-recovery elements of ERAS.
Gastrointestinal function is frequently impaired after extensive peritonectomy. Paralytic ileus is common, and early oral feeding may be thwarted by nausea, vomiting, or abdominal distension, sometimes necessitating temporary nasogastric decompression. Patients also experience considerable pain from large abdominal incisions and diaphragmatic stripping, while drains, catheters, and epidural lines can restrict movement and delay ambulation. These factors hinder pulmonary recovery and raise venous-thromboembolism risk. Consequently, ERAS pathways must be customized to each patient’s functional status, operative extent, and postoperative course-incorporating tailored fluid regimens, graded nutritional strategies, and stepwise mobilization plans.
Another major obstacle is the lack of a standardized approach across hospitals, resulting in varying levels of adherence and divergent clinical outcomes. Resistance to shifting from traditional practices also complicates ERAS implementation. Comprehensive training is crucial to ensure that all surgical team members understand the protocol’s principles, reducing inconsistent adherence and optimizing benefits. Institutional culture plays a vital role as well: Long-established routines may resist the sweeping changes required for ERAS success. Overcoming these barriers demands a collaborative effort to establish uniform protocols, enhance staff education, and foster an environment that welcomes innovation. When these elements align, ERAS can significantly advance surgical care by improving recovery times and reducing complication rates. National surveys from India and Italy reflect this challenge, revealing widespread support for ERAS but limited adoption and high variation among centers[83,84]. A qualitative study, including surgeons, anesthesiologists, nurses, and dietitians, identified 8 core issues, such as limited resources, high patient turnover, inadequate policy support, and skepticism regarding patient safety[85].
Variability in healthcare infrastructure-from tertiary hospitals to primary units-further influences implementation and outcomes. Well-resourced centers can support comprehensive perioperative care, whereas low-income hospitals may lack costly elements such as nutritional-support teams or postoperative rehabilitation. Nonetheless, many ERAS components-preoperative counselling, smoking and alcohol cessation, glycemic control, judicious fluid balance, and early mobilization-can usually be adopted even in resource-constrained settings and still yield significant postoperative benefits. Differences in surgical experience with CRS-HIPEC also matter: Teams with limited exposure may focus on technical demands at the expense of strict protocol adherence, unintentionally reducing ERAS benefits. Such factors must be weighed when interpreting ERAS reproducibility across regions.
Despite agreement on ERAS benefits, poor doctor-patient collaboration persists, as some patients remain skeptical about early mobilization and short hospital stays. Financial constraints may also reduce compliance, particularly if regional anesthesia or additional supportive techniques increase medical costs. In some cases, health workers worry about deviating from established routines, citing patient safety concerns. Hospital staff shortages, leadership gaps, and inadequate policy frameworks further hinder adoption. These challenges amplify the workload for personnel, especially in hospitals with high bed turnover and limited multidisciplinary coordination. Poor team communication can compromise protocol implementation if surgeons, anesthesiologists, and nurses fail to align on individualized care plans. Another investigation, focusing on nurses’ perspectives, identified parallel issues, adding that strong leadership, widespread ERAS awareness, and supportive financial policies are vital for success[86,87]. Addressing these hurdles will require a multi-pronged strategy that includes focused education, transparent communication, and structural support to realize the protocol’s full potential (Figure 1).
Figure 1 The integration of enhanced recovery after surgery protocols in gastrectomy with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: Challenges and future perspectives.
CRS: Cytoreductive surgery; ERAS: Enhanced recovery after surgery; HIPEC: Hyperthermic intraperitoneal chemotherapy; PC: Peritoneal carcinomatosis.
PERSONALIZED PATHWAYS FOR ERAS IN GASTRECTOMY, CRS, AND HIPEC
Tailoring ERAS protocols to individual patient factors is essential, particularly for those undergoing gastrectomy with CRS and HIPEC. Not all patients benefit equally from ERAS, so assessing comorbidities, nutritional status, and psychosocial factors helps determine each patient’s resilience to early mobilization and postoperative diet[86]. Disease stage and surgical complexity also matter: Patients with early-stage gastric cancer tend to benefit more than those needing extensive resections for advanced disease. Optimizing nutritional status and managing conditions such as diabetes or cardiovascular disease can significantly improve recovery. Elderly patients may face additional hurdles, including higher complication rates and prolonged recovery tied to physiological changes. Moreover, psychological well-being and robust social support are crucial for adherence to the ERAS pathway, as anxiety or depression can delay recovery. By selecting patients best suited for intensive ERAS protocols and addressing individual barriers to adherence, clinicians can enhance surgical outcomes and maintain continuity of care-particularly in the high-stakes setting of gastrectomy with CRS and HIPEC.
CONCLUSION
ERAS protocols mark a paradigm shift in managing complex surgical procedures, including gastrectomy with CRS and HIPEC for gastric cancer with PC. By integrating multidisciplinary strategies across preoperative, intraoperative, and postoperative phases, ERAS can significantly improve recovery times and reduce complications. These benefits may also facilitate improved oncological outcomes through reduced hospital stays and enhanced patient readiness for subsequent treatments. Despite notable local successes, standardized global implementation remains crucial. Gastric cancer’s heterogeneity, combined with the technical intricacies of CRS and HIPEC, varies among regions, reinforcing the need for a unified, evidence-based framework. Strengthening international collaboration will foster knowledge exchange, consolidate data, and guide the evolution of ERAS protocols to address the unique challenges posed by gastric cancer with PC. Through ongoing refinement and broader adoption, ERAS may become the new standard of care. It can optimize patient well-being, shorten recovery, and potentially improve long-term survival by enabling earlier initiation of postoperative therapy.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country of origin: Thailand
Peer-review report’s classification
Scientific Quality: Grade B, Grade B
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade B
P-Reviewer: Chen YH S-Editor: Luo ML L-Editor: A P-Editor: Wang CH