INTRODUCTION
Breast cancer ranks as one of the most common malignant tumors among women globally. Epidemiological data indicate that its incidence rate (11.7%) now exceeds that of lung cancer, positioning it as the most prevalent cancer[1]. Breast cancer is characterized by significant molecular heterogeneity and is primarily classified into hormone receptor-positive, HER2-positive, and triple-negative subtypes. Its development is intricately linked to genetic, hormonal, and environmental factors[2,3]. Recent advancements in treatment have shifted towards a precise and personalized approach based on molecular typing. This approach integrates traditional methods such as surgery, chemotherapy, and radiotherapy with novel therapies, including endocrine therapy, targeted drugs such as CDK4/6 inhibitors and anti-HER2 antibody-drug conjugates, and immune checkpoint inhibitors, significantly enhancing patient survival rates. Despite these medical advancements, the psychological and social burdens imposed by the disease and its treatments persist as critical challenges in clinical management[4,5]. Depressive symptoms, the most prevalent psychological complication among breast cancer patients, not only drastically diminish patients' quality of life but also impact treatment compliance and the anti-tumor immune response through mechanisms such as neuroendocrine regulation, ultimately leading to poorer prognoses[6]. Globally, the incidence rate of depressive symptoms among breast cancer patients stands at a substantial 32.2%[7]. Wang et al's systematic review, based on evidence-based medicine, confirmed a significant positive correlation between depressive status and the risk of breast cancer recurrence, all-cause mortality, and breast cancer-specific mortality, highlighting depressive symptoms as an independent prognostic factor for breast cancer[8]. The research conducted by Mao et al[9] analyzed the clinical data of 360 middle-aged and young breast cancer patients and constructed a nomogram risk prediction model based on tumor grading, monthly income, pain score, family support, and physical activity. This model was used to identify patients at high risk of depressive symptoms at an early stage. The model demonstrated high predictive efficacy and provided a scientific basis for targeted psychological intervention[9]. Consequently, the early identification and prevention of depressive symptoms in breast cancer patients hold vital clinical significance. This manuscript aims to systematically review early detection methods and preventive strategies for depressive symptoms in this patient group. By synthesizing existing research evidence, it proposes comprehensive intervention plans under a multidisciplinary collaboration model, striving to provide a scientific basis and practical recommendations for clinical practice, thereby aiming for the comprehensive management of both the physical and mental health of breast cancer patients.
ANALYSIS OF RISK FACTORS FOR DEPRESSIVE SYMPTOMS IN PATIENTS WITH BREAST CANCER
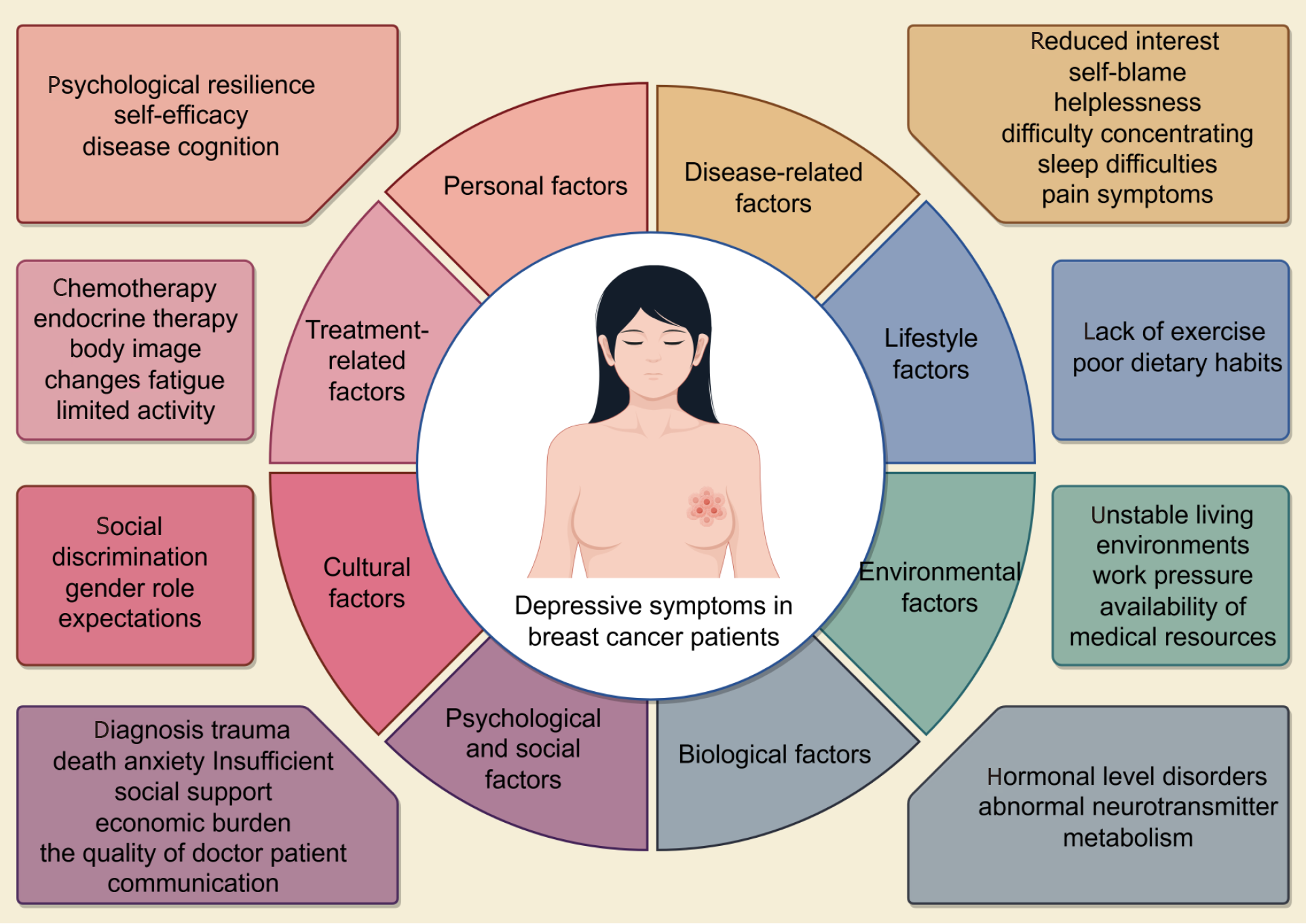
The development and manifestation of depressive symptoms in breast cancer patients result from a complex interplay of multiple factors. These risk factors include disease-related, treatment-related, psychological, social, personal, biological, lifestyle, cultural, social background, and environmental influences (Figure 1). The mechanism underlying these depressive symptoms is intricate.
Figure 1
Risk factors for depressive symptoms in breast cancer patients.
Depressive symptoms in breast cancer patients typically present as psychological and physical symptoms. Psychologically, patients frequently experience persistent low mood, diminished interest, self-blame, feelings of helplessness, and difficulty concentrating. Physically, sleep difficulties are commonly reported among these patients, and when combined with pain symptoms, they form a significant symptom cluster. In contrast, the frequency of other common physical symptoms such as generalized pain, fatigue, and vomiting is relatively low, possibly due to a decline in language expression abilities or decreased interest, which are symptoms associated with depression[10]. Treatment-related factors significantly influence depressive symptoms. Chemotherapy, for instance, affects neurotransmitter metabolism by initiating inflammatory responses, impairs neuroplasticity, disrupts emotional regulation and cognitive functions, and alters the intestinal microbiota community. This alteration exacerbates systemic inflammation, creating a vicious cycle that significantly worsens depressive symptoms[11]. Endocrine therapies, such as aromatase inhibitors, disrupt hormonal balances, affecting the function of the hypothalamic-pituitary-adrenal axis, reducing the concentration of monoamine neurotransmitters in the synaptic cleft, and increasing the risk of depression[12]. Additionally, treatment side effects, including changes in body image, fatigue, and limited physical activity, profoundly impact mental health[13]. In terms of psychological and social factors, the trauma of a cancer diagnosis and the anxiety of potential death are primary psychological stressors for breast cancer patients[14]. Insufficient social support, economic burden, and the quality of doctor-patient communication significantly influence the emergence and progression of depressive symptoms in breast cancer patients[5,15]. Financial strain serves not only as an independent predictor of depression but also directly intensifies the depression experienced by patients and their family caregivers. Additionally, it indirectly heightens depressive emotions through the mediating effect of fear of cancer recurrence[16]. Personal factors such as psychological resilience, self-efficacy, and disease cognition are crucial protective elements for the mental health of these patients, offering significant buffering mechanisms[17-19]. Biologically, disorders in hormonal levels due to chemotherapy and endocrine therapy, along with abnormal neurotransmitter metabolism, constitute significant biological underpinnings for depression. Inflammatory responses and genetic comorbidities also contribute to the risk of depression through mechanisms such as immune response regulation, cell cycle control, and gene expression[20]. Furthermore, an imbalance in soluble cyclooxygenase-mediated metabolism by the liver may play a pivotal role in linking depression with comorbid breast cancer[21]. Lifestyle factors, including inadequate exercise and poor dietary habits, potentially worsen depression by influencing the intestinal microbiota community and inflammatory responses[22]. Cultural factors encompass varying cultural perceptions of breast cancer and depression, social discrimination, and expectations related to gender roles, potentially increasing psychological stress[23]. Environmental factors such as unstable living conditions, work stress, and the availability of medical resources can also impact the mental well-being of patients[24].
In summary, the development of depressive symptoms in breast cancer patients results from the interplay of multiple factors with a complex underlying mechanism. Future research should further explore these interactions and devise targeted intervention strategies to enhance the mental health of these individuals.
SCREENING OF DEPRESSIVE SYMPTOMS IN BREAST CANCER PATIENTS AND THE APPLICATION OF BIOMARKERS IN THE EARLY IDENTIFICATION PROCESS
Early identification of depressive symptoms in breast cancer patients is crucial for timely intervention and improving prognosis. Research indicates that depressive symptoms not only significantly diminish patients' quality of life but also contribute to adverse events, potentially impacting survival rates and disease outcomes[25]. Therefore, in the comprehensive management of breast cancer, standardized screening and systematic assessment of depressive symptoms are essential clinical strategies. Commonly used tools in clinical settings include the Patient Health Questionnaire-9, Hospital Anxiety and Depression Scale, and Beck Depression Inventory. These instruments are highly reliable and valid across different administration modes, and their ease of use makes them well-suited for clinical practice[26].
Additionally, laboratory tests serve as supplementary tools for early detection of depressive symptoms. In their study, Yu et al[27] investigated the immunopathological mechanisms of depression in breast cancer patients and identified potential biomarkers. They found that elevated levels of inflammatory markers such as C-reactive protein, interleukin (IL)-6, and tumor necrosis factor-α are closely linked to the development of depression. These markers not only influence the progression of breast cancer but may also exacerbate depressive symptoms by affecting neurotransmitter metabolism, including the tryptophan metabolic pathway and immune function[27]. Perez-Tejada et al[28] examined monoamine levels in breast cancer patients, discovering that high levels of kynurenine and low levels of dopamine (DA) were significantly associated with depressive symptoms, particularly among young and middle-aged women. In this group, a lower DA level had a more pronounced predictive effect on depressive symptoms. Additionally, the study highlighted a statistically significant negative conditional effect of 5-hydroxytryptamine levels on depressive symptoms in young women. These findings reveal the importance of evaluating physiological indicators such as monoamine levels to identify high-risk individuals before depressive symptoms manifest, thus providing a scientific foundation for early psychological interventions[28]. The research conducted by He et al[29] involved plasma marker detection and metabolic characteristic analysis comparing breast cancer patients with healthy controls. They discovered that levels of glial fibrillary acidic protein and lipocalin 2 were significantly correlated with depressive symptoms. Furthermore, metabolomics analysis identified specific metabolic alterations in breast cancer patients[29]. These findings offer potential biomarkers for the early detection of depressive and anxiety symptoms in this patient group and establish a groundwork for future research and clinical applications.
PREVENTION OF DEPRESSIVE SYMPTOMS IN BREAST CANCER PATIENTS: COMPREHENSIVE INTERVENTION FROM A MULTIDISCIPLINARY PERSPECTIVE
The prevention of depressive symptoms in breast cancer patients is a comprehensive endeavor rooted in the biopsychosocial medical model, which necessitates collaboration among Western medicine, traditional Chinese medicine (TCM), and various disciplines. The oncology department assumes a pivotal role in medical interventions, focusing on the impacts of treatment-related factors on patients' psychological states. It is essential to collaborate with psychiatrists to optimize drug selection and treatment timing.
The psychiatric and psychology departments provide core professional support within the prevention system. The psychological interventions they offer are crucial in preventing and alleviating depressive symptoms. Evidence-based cognitive behavioral therapy, through a structured and goal-oriented approach, effectively assists patients in reconstructing their cognitive patterns, enhancing their emotional regulation capabilities, and significantly reducing anxiety and depressive symptoms[30]. Through systematic meditation training, mindfulness-based therapy helps patients develop a non-judgmental awareness of the present moment, which diminishes excessive concerns about disease prognosis[31]. Supportive psychotherapy plays a vital role by establishing a therapeutic doctor-patient relationship, offering emotional support, and providing a space for emotional expression, combined with disease knowledge education, to significantly reduce psychological stress[32]. The nursing team acts as a critical bridge within the prevention system, implementing a standardized psychological assessment system to promptly identify high-risk patients. Nurses also deliver continuous psychological support through health education, relaxation training, and support group facilitation. Social workers contribute by creating a multi-level support system that includes establishing family support networks, integrating social resources, and providing social adaptation training. Additionally, exercise interventions have been shown to significantly improve depressive symptoms in breast cancer patients. Moderate aerobic exercise such as walking, swimming, and yoga can promote the release of endorphins, enhance mood, improve physical function, and boost self-efficacy, thus helping patients better manage the psychological stress associated with their condition[33,34]. According to TCM, the depressive symptoms in breast cancer patients are primarily associated with liver qi stagnation and imbalance of qi and blood. TCM emphasizes the significant role of physical, psychological, emotional, and mental well-being in the onset, progression, and prognosis of cancer[35]. Clinically, it is observed that breast cancer patients often experience long-term emotional suppression, leading to liver qi stagnation, which then impacts the spleen and stomach, disrupting their function and causing a deficiency in qi and blood biochemistry. This results in a pathological state characterized by qi stagnation and blood stasis. Thus, TCM approaches the treatment of breast cancer-related depression by soothing the liver, dispelling depression, regulating qi and blood, and combining psychological counseling with pharmacotherapy to treat both mind and body. TCM monomers and compounds, known for their rich biological activities, can provide dual anti-depressive and anti-tumor effects through multi-target and multi-pathway regulation[36-38]. The Modified Xiaoyao Pill, for example, regulates serotonin levels, reduces the expression of inflammatory factors (IL-6, IL-1β, tumor necrosis factor-alpha), and inhibits the JAK2/STAT3 signaling pathway, demonstrating dual antidepressant and anti-tumor effects in a mouse model of breast cancer complicated with depression[39]. Acupuncture, as a traditional Chinese medical therapy, stimulates specific acupoints to regulate the functions of the nervous and endocrine systems, promoting the balance of "qi" in the body and thereby alleviating depression and anxiety symptoms[40]. Baduanjin, a form of traditional Chinese Qigong exercise, uses slow and gentle movements combined with breathing regulation to enhance qi and blood circulation, boost physical fitness, and relieve psychological stress[41]. For patients with moderate to severe depressive symptoms or those unresponsive to psychological interventions, pharmacological intervention is necessary. Western medicine typically prescribes serotonin reuptake inhibitors as the first-line treatment, with careful consideration of potential interactions with chemotherapy drugs[42].
In summary, the prevention of depressive symptoms in breast cancer patients demands a multidisciplinary approach, integrating various interventions from medicine, psychology, nursing, social work, and TCM. This creates a comprehensive and systematic prevention system that improves patients' psychological well-being and quality of life.
CONCLUSION
Early identification of depressive symptoms in breast cancer patients is crucial for enhancing their mental health and quality of life. This process involves the use of standardized screening tools and clinical interviews and relies on the collaborative efforts of a multidisciplinary team, including oncologists, psychiatrists, nurses, and social workers, to ensure the timely detection of emotional changes in patients. The integration of modern technologies plays a significant role in supporting this process. For example, emotional recognition technology powered by artificial intelligence (AI) can automatically detect potential depressive symptoms by analyzing patients’ voices, facial expressions, and textual content[43]. Additionally, wearable devices such as smart wristbands and heart rate monitors can continuously monitor physiological indicators such as heart rate variability and sleep quality. When combined with mental health screening tools, these data enable healthcare providers to detect emotional fluctuations in patients earlier and with greater accuracy[44].
Prevention strategies should incorporate a blend of Western medicine, TCM, and multidisciplinary collaboration while optimizing modern technologies to enhance intervention effects. Western medicine interventions typically focus on pharmacological and psychological therapies, complemented by lifestyle modifications such as moderate exercise and a healthy diet. TCM interventions emphasize the holistic and integral approach to both the human body and the disease, using techniques such as acupuncture, massage, and other TCM modalities to adjust patients' overall physical and mental state, alleviate emotional fluctuations, and improve physical functions.
A comprehensive intervention that combines Western and TCM with multidisciplinary collaboration can provide personalized and all-encompassing support for patients, reduce the side effects of drugs, and enhance treatment outcomes. The integration of modern technologies allows for more precise and efficient comprehensive interventions. Intelligent algorithms can assimilate data from Western medicine, TCM, and multidisciplinary sources to create personalized, comprehensive intervention plans for patients. These plans can be continuously evaluated and dynamically adjusted through remote monitoring systems, ensuring real-time adaptation of treatment strategies. Furthermore, big data analysis can elucidate differences in intervention effects among various patient groups, offering a scientific basis for precision medicine.
Through the implementation of multi-level comprehensive interventions and modern technologies, depressive symptoms in breast cancer patients can be more effectively identified and managed, substantially improving their mental health and overall quality of life.
Early identification and prevention of depressive symptoms in breast cancer patients are crucial, both clinically and socially. Throughout the treatment process, these patients frequently face dual burdens of physical and psychological stress, and the incidence of depressive symptoms is notably high. These symptoms impact treatment outcomes and quality of life and may also expedite the progression of the disease. By recognizing depressive symptoms early, healthcare providers can implement timely interventions to prevent symptom deterioration and enhance the overall rehabilitation outcomes for patients. Additionally, the execution of preventive strategies can minimize the initial occurrence of depression, thereby assisting patients in more effectively managing the psychological challenges posed by their condition. Indeed, early identification and prevention are not only critical for improving the mental health of breast cancer patients but also integral to achieving comprehensive health management. By employing a comprehensive intervention model that melds modern technology with integrated Chinese and Western medicine and multidisciplinary collaboration, the approach to mental health becomes more intelligent, personalized, and precise. This model provides more comprehensive and individualized support for breast cancer patients and other high-risk groups, significantly enhancing their quality of life and setting new directions for the future development of mental health care.
Looking forward, the continual advancements in technologies such as AI, big data, and telemedicine are poised to revolutionize the mental health management of breast cancer patients. These developments promise a new era of increased precision and efficiency, enabling more effective management of mental health conditions and better patient outcomes.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade A
Novelty: Grade A
Creativity or Innovation: Grade A
Scientific Significance: Grade A
P-Reviewer: Jin H S-Editor: Liu H L-Editor: A P-Editor: Zhao YQ