Published online Oct 24, 2022. doi: 10.5306/wjco.v13.i10.848
Peer-review started: April 19, 2022
First decision: May 31, 2022
Revised: June 8, 2022
Accepted: September 21, 2022
Article in press: September 21, 2022
Published online: October 24, 2022
Processing time: 183 Days and 21 Hours
Situs inversus totalis (SIT) is a rare congenital condition in which the structure of the abdominal and thoracic cavities is the mirror image of normal. This anatomic reversal makes laparoscopic surgery difficult when treating colorectal cancer.
We describe the successful laparoscopic hemicolectomy of a 68-year-old Chinese woman with SIT and ascending colon cancer. Based on preoperative imaging and careful consideration of the patient’s anatomy, the position of the surgeon was modified such that the surgeon stood between her legs, while the surgical assistant and endoscopist stood to the surgeon’s left. Trocar position was also adjusted appropriately. The surgery lasted 178 min, during which the patient lost 50 mL of blood. Pathology analysis of the resected tumor confirmed an adenocarcinoma in clinical stage pT3N0M0, without lymph node involvement. The patient experienced no postoperative complications and was discharged 10 d after surgery.
This case illustrates that careful positioning of the surgeon can facilitate laparoscopic surgery of SIT patients.
Core Tip: Situs inversus totalis (SIT) is a rare congenital anomaly in which the organs in the chest and abdomen are located in a mirror image reversal of their normal positions. We present a rare case of SIT accompanied by colon cancer. After careful consideration of the patient’s anatomy, we modified the position of the surgeon to enable successful laparoscopic hemicolectomy. This case highlights that careful positioning of the surgeon can make laparoscopic surgery feasible and safe for SIT patients.
- Citation: Hu JL, Li QY, Wu K. Ascending colon cancer and situs inversus totalis – altered surgeon position for successful laparoscopic hemicolectomy: A case report. World J Clin Oncol 2022; 13(10): 848-852
- URL: https://www.wjgnet.com/2218-4333/full/v13/i10/848.htm
- DOI: https://dx.doi.org/10.5306/wjco.v13.i10.848
Situs inversus totalis (SIT) is a rare congenital anomaly in which organs in the chest and abdomen are positioned in the mirror image of normal. Incidence in the general population ranges from 1 per 8000 to 1 per 25000[1], and SIT patients with colon cancer are even rarer. Surgery in SIT patients, particularly laparoscopic procedures, are considered more difficult because of the anatomical abnormality[2,3].
Here, we report the case of a 68-year-old patient with SIT and ascending colon cancer who successfully underwent laparoscopic hemicolectomy with radical lymph node dissection. The success of the procedure was due to careful consideration of the patient’s anatomy and optimization of the surgical team’s position.
A 68-year-old Chinese woman visited our hospital in December 2020 due to gradual enlargement of a mass in the left lower abdomen.
The patient had experienced intermittent bloody stool for nearly 1 year.
The patient did not have any history of past illnesses.
The patient had no remarkable personal or family history.
The patient was 142 cm tall and weighed 35 kg, corresponding to a body mass index of 17.4 kg/m2. Physical examination revealed a mass measuring 4 cm × 5 cm in the left lower abdomen.
Laboratory tests indicated no anemia, normal electrolytes, and no dysfunction of the liver or kidneys. The level of carcinoembryonic antigen in serum was slightly elevated (8.37 ng/mL; normal, < 2.5 ng/mL), while levels of carbohydrate antigen (CA) 12-5 and CA 19-9 were normal.
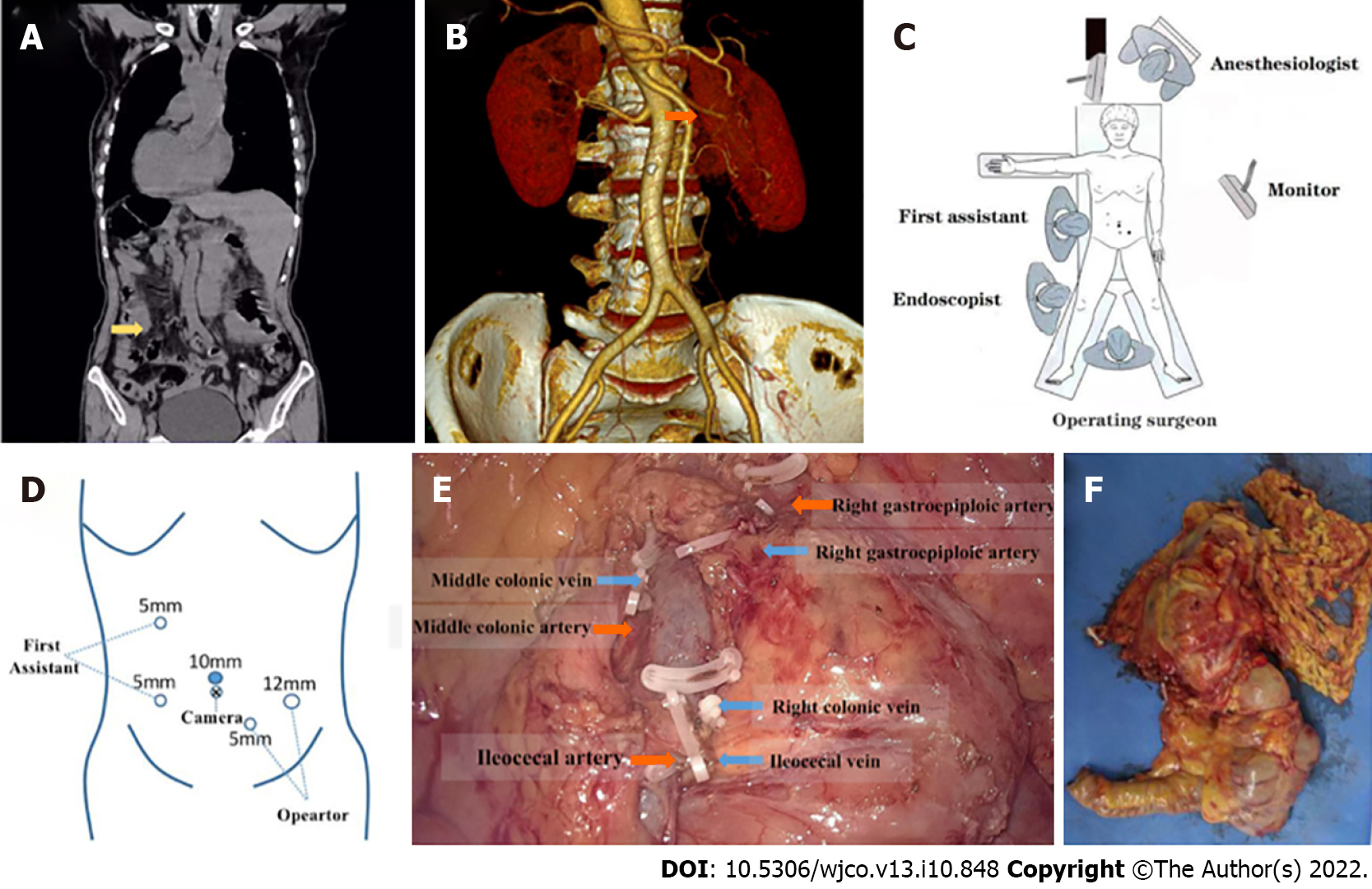
Chest and abdominal computed tomography (CT) revealed that the structure of the thoracic cavity and all abdominal organs were inverted from the normal position, leading to a diagnosis of SIT (Figure 1A). A mass in the ascending colon was confirmed (Figure 1A), and no evidence of distant metastasis was found. CT angiography showed that the superior mesenteric artery was located on the left side (Figure 1B). Colonoscopy revealed a mass in the ascending colon that occupied the complete diameter of the lumen, which together with intestinal stenosis prevented the passage of the colonoscope.
The patient was diagnosed with colon cancer and SIT.
Laparoscopic hemicolectomy with radical lymphadenectomy was performed under general anesthesia. The patient was placed in a modified lithotomy position, with her head down and legs apart. The surgeon stood between her legs, and the first assistant and endoscopist stood on the surgeon’s left, which is the opposite of the usual position for surgery (Figure 1C). The trocar placement was adjusted in order to facilitate surgical procedures (Figure 1D). The ileocolic vessels were carefully dissected, then the colon was dissected and reconstructed uneventfully (Figure 1E).
Pathology of resected tumor tissue revealed it to be moderately differentiated adenocarcinoma in stage pT3N0M0 involving invasion of the serosa (Figure 1F). All 22 resected regional lymph nodes were negative.
The entire surgery lasted 178 min, during which total blood loss was 50 mL. After surgery, the patient received six courses of chemotherapy with oxaliplatin and capecitabine, which proceeded uneventfully. At 12-mo follow-up, the patient reported being in good condition, and no symptoms or recurrence were noted.
SIT may arise from inherited or spontaneous genetic mutations that affect embryonic development[4]. Organ function is normal in most patients with SIT, and there are no obvious clinical symptoms, so most are diagnosed with the condition on the basis of X-ray imaging, ultrasonography, magnetic resonance imaging, or CT as in the present case. SIT can lead to misdiagnosis of colon cancer because the cancer manifests as the mirror opposite of the typical manifestations of obstruction, constipation, and diarrhea in the case of left colon cancer, or of anemia, weight loss, and fatigue in the case of right colon cancer. Gastroscopy, colonoscopy, and CT are recommended to avoid misdiagnosis of cancer patients with SIT. As reported for other SIT patients[5], colonoscopy was successful in our patient, who was in the right decubitus position.
The success of treatment in the present case was due to the clinical team’s experience and a clear understanding of the patient’s anatomy, leading the team to adjust their normal positions for surgery. The team also remained flexible during the procedure in order to adapt to last-minute discoveries of vascular anomalies. Both CT angiography and CT colonography are useful for investigating anatomy and planning laparoscopic procedures[3,6,7]. Laparoscopic surgery, which is increasingly applied to a broad range of patients[8], can be a good option for SIT patients, following appropriate planning based on careful imaging[6,9-12]. While laparoscopic procedures on SIT patients can be more challenging for right-handed surgeons than for left-handed ones[13], adjusting the surgeon’s position can help compensate for this[6].
Several adjustments to the laparoscopic procedures were made to compensate for our patient’s SIT. The position of the surgical team was reversed from normal, and the trocar positions were correspondingly different, similar to those used to treat colorectal cancer on the left side. The surgeon in our case was right-handed, so he ligated the ileocolic vessels and mobilized the ascending colon using the right hand through a 12-mm trocar in the right lower quadrant. In this way, the surgeon compensated for the normal requirement to use the left hand during laparoscopic right hemicolectomy. In fact, the surgeon and his associates were able to complete the procedures smoothly despite the limited operating space due to the patient’s small stature.
Our case report highlights that with careful preoperative imaging and planning, the surgical team can adjust their positions around the patient and the placement of trocars accordingly, allowing a safe and effective procedure. In this way, SIT patients with cancer can benefit from the minimal invasiveness of laparoscopic surgery like patients with normal anatomy.
Our case describes the successful laparoscopic hemicolectomy and radical lymphadenectomy of a SIT patient with ascending colon cancer. It highlights the importance of careful imaging assessment and preoperative planning, with the corresponding optimization of the surgical team’s positioning around the patient. Laparoscopic surgery of SIT patients can be challenging but it remains a safe and effective minimally invasive option if appropriate steps are taken.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Carannante F, Italy; Wang P S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Kigasawa Y, Takeuchi H, Kawakubo H, Fukuda K, Nakamura R, Takahashi T, Wada N, Kitagawa Y. Laparoscopy-assisted distal gastrectomy in a case of gastric cancer with situs inversus totalis: a case report. Asian J Endosc Surg. 2017;10:47-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Xu Q, Liu W, Lin C, Dang Y. Transverse colon cancer with obstruction in a patient with situs inversus totalis: A case report and review of literature. Asian J Surg. 2020;43:1186-1188. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Yaegashi M, Kimura T, Sakamoto T, Sato T, Kawasaki Y, Otsuka K, Wakabayashi G. Laparoscopic sigmoidectomy for a patient with situs inversus totalis: effect of changing operator position. Int Surg. 2015;100:638-642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Reish O, Aspit L, Zouella A, Roth Y, Polak-Charcon S, Baboushkin T, Benyamini L, Scheetz TE, Mussaffi H, Sheffield VC, Parvari R. A Homozygous Nme7 Mutation Is Associated with Situs Inversus Totalis. Hum Mutat. 2016;37:727-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Choi DH, Park JW, Kim BN, Han KS, Hong CW, Sohn DK, Lim SB, Choi HS, Jeong SY. Colonoscopy in situs inversus totalis patients. Am J Gastroenterol. 2008;103:1311-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Sasaki K, Nozawa H, Kawai K, Hata K, Kiyomatsu T, Tanaka T, Nishikawa T, Otani K, Kaneko M, Emoto S, Murono K, Watanabe T. Laparoscopic hemicolectomy for a patient with situs inversus totalis: A case report. Int J Surg Case Rep. 2017;41:93-96. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Chen W, Liang JL, Ye JW, Luo YX, Huang MJ. Laparoscopy-assisted resection of colorectal cancer with situs inversus totalis: A case report and literature review. World J Gastrointest Endosc. 2020;12:310-316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 8. | Hoyuela C, Juvany M, Carvajal F. Single-incision laparoscopy vs standard laparoscopy for colorectal surgery: A systematic review and meta-analysis. Am J Surg. 2017;214:127-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Kudo T, Matsuda T, Urakawa N, Hasegawa H, Kanaji S, Yamashita K, Oshikiri T, Kakeji Y. Laparoscopic sigmoidectomy with splenic flexure mobilization for colon cancer in situs inversus totalis: Preoperative assessment and preparation. Asian J Endosc Surg. 2022;15:168-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Kojima Y, Sakamoto K, Tomiki Y, Sugimoto K, Okazawa Y, Makino Y. Laparoscopic right colectomy for a patient with situs inversus totalis. J Surg Case Rep. 2019;2019:rjz080. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Kim YW, Ryu H, Kim DS, Kim IY. Double primary malignancies associated with colon cancer in patients with situs inversus totalis: two case reports. World J Surg Oncol. 2011;9:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Fujiwara Y, Fukunaga Y, Higashino M, Tanimura S, Takemura M, Tanaka Y, Osugi H. Laparoscopic hemicolectomy in a patient with situs inversus totalis. World J Gastroenterol. 2007;13:5035-5037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 49] [Cited by in RCA: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Oms LM, Badia JM. Laparoscopic cholecystectomy in situs inversus totalis: The importance of being left-handed. Surg Endosc. 2003;17:1859-1861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |