Published online Apr 24, 2021. doi: 10.5306/wjco.v12.i4.282
Peer-review started: January 7, 2021
First decision: February 15, 2021
Revised: February 19, 2021
Accepted: March 24, 2021
Article in press: March 24, 2021
Published online: April 24, 2021
Processing time: 102 Days and 23.7 Hours
Sarcomatoid carcinoma is a rare subtype of non-small-cell lung cancer, commonly associated with locally advanced disease, early metastasis, and poor prognosis. Tongue metastasis from lung cancer is a rare condition that may occur in advanced stage of the disease.
The patient was a 70-year-old female with a history of resected pulmonary sarcomatoid carcinoma (PSC) who presented with subacute tongue swelling, imparting the clinical impression of a lingual abscess. However, histologic examination of the partial glossectomy revealed a high-grade, poorly differentiated spindle and epithelioid carcinoma consistent with metastatic PSC.
Although uncommon, clinicians should be cognizant of the possibility of a metastatic process to the tongue mimicking a benign or inflammatory process. A high index of suspicion for metastatic disease should be maintained when tongue swelling is observed in patients with a known history of PSC.
Core Tip: Tongue metastasis from pulmonary sarcomatoid carcinoma is an uncommon phenomenon. A high index of suspicion for metastatic disease should be maintained in patients with a known history of pulmonary sarcomatoid carcinoma when tongue swelling or radiologic image indicating a lesion in the tongue, especially near the tongue base, is observed, and appropriate investigations should be undertaken.
- Citation: Guo MN, Jalil A, Liu JY, Miao RY, Tran TA, Guan J. Tongue swelling as a manifestation of tongue metastasis from pulmonary sarcomatoid carcinoma: A case report. World J Clin Oncol 2021; 12(4): 282-289
- URL: https://www.wjgnet.com/2218-4333/full/v12/i4/282.htm
- DOI: https://dx.doi.org/10.5306/wjco.v12.i4.282
Sarcomatoid carcinoma is a rare biphasic tumor expressing both malignant mesenchymal (sarcomatoid) and epithelial (carcinomatous) components[1]. Pulmonary sarcomatoid carcinoma (PSC) is a poorly differentiated subtype of non-small-cell lung cancer (NSCLC)[2], commonly associated with aggressive clinical behaviors such as locally advanced disease, early metastasis, and poor prognosis. Tongue metastases are rare clinical events that may occur in advanced stage of the disease[3].
We herein report a rare case of tongue metastasis from a pleomorphic carcinoma, a subtype of PSC. To the best of our knowledge, this is the first documented case of tongue metastasis by this subtype of PSC.
A 70-year-old female presented with a 2-wk-history of tongue swelling and altered mental status.
Six months prior to admission, the patient underwent left upper lung lobectomy for pulmonary pleomorphic carcinoma, which is considered a subtype of PSC. The neoplasm was positive for mesenchymal-epithelial transition (MET) exon 14 skipping and PIK3CA mutations, with a programmed death-ligand 1 (PD-L1) positivity of 75%. The disease was staged as T4N1M0. She was started with capmatinib for stage IV PSC with MET exon 14 skipping mutation.
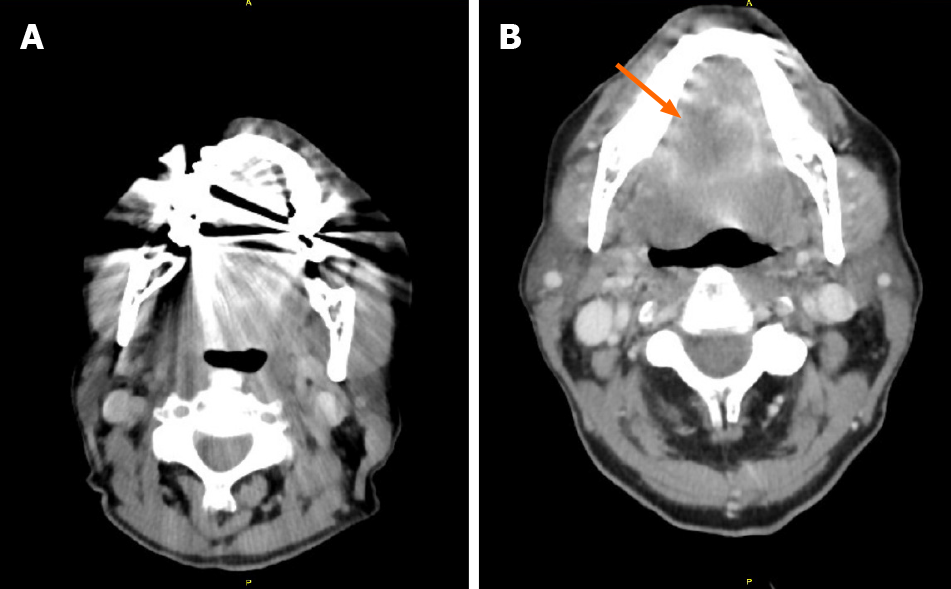
One month prior, she underwent left vocal cord injection for left vocal cord paralysis. Two weeks prior, she developed tongue swelling, dysphagia and odynophagia. A computed tomography (CT) of the neck with contrast was grossly unremarkable (Figure 1A), although visualization was limited due to dental streak artifact and motion artifact. The patient was started with methylprednisolone (Medrol) dose pack by her oncologist with capmatinib on hold as it was concerned that her tongue swelling could be an allergic reaction to capmatinib. However, her tongue swelling continued to worsen to the point that she was unable to take anything by mouth. She became more lethargic that prompted her presentation to the emergency department.
She had a prior medical history of atrial fibrillation, deep venous thrombosis, and bilateral hip osteoarthritis.
She was a former 25 pack/year smoker, but had stopped smoking 25 years prior to this presentation.
On arrival, patient's peripheral capillary oxygen saturation (SpO2) was 84% on room air. Physical examination revealed that the tongue and floor of the mouth were severely edematous; the deep oral tongue felt firm to palpation; the overlying mucosa was intact and of normal color; the submental space was mildly full; and cervical lymphadenopathy was not palpable.
Laboratory studies revealed polymorphonuclear leukocytosis with white blood cell count of 20.85 × 103/μL.
Repeated CT of the neck with contrast (Figure 1B) identified a 2.7 cm × 3.2 cm × 1.9 cm lesion, which were not clearly visible in the CT one week earlier.
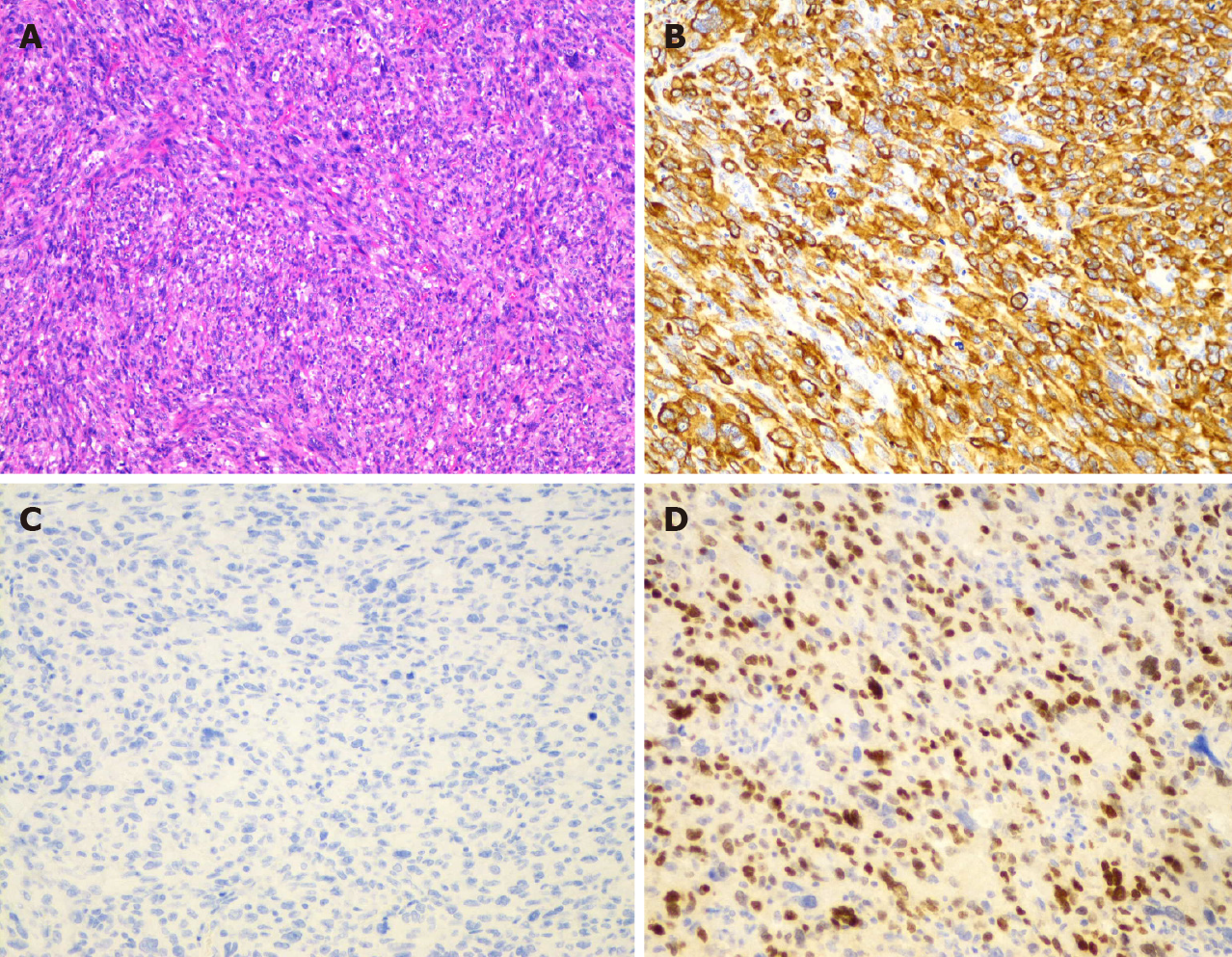
Histologic examination of the tongue mass showed a high-grade, poorly differentiated spindle and epithelioid neoplasm (Figure 2) that was positive for cytokeratin AE1/AE3 and TTF-1, but negative for p40. With positive staining for TTF-1, the tongue mass was considered a metastatic pleomorphic carcinoma of pulmonary origin to the tongue.
Given the rapid interval change, an abscess was favored, with a differential diagnostic consideration of a necrotic mass. Patient was intubated for airway protection and admitted to the intensive care unit. She was started on empirical antibiotics with vancomycin and piperacillin/tazobactam. She then underwent midline partial glossectomy that revealed a submucosal mass without involvement of the tongue surface. It extended into the base of the tongue and the floor of the mouth.
The patient was extubated after the surgery with satisfactory oxygen saturation on room air and mentation back to normal. She then underwent percutaneous endoscopic gastrostomy tube placement for her persistent dysphagia. She was discharged home in a stable condition. To date, the patient has been receiving chemo-immunotherapy with carboplatin, Nab-paclitaxel, and pembrolizumab, with regular follow-ups with her oncologist.
Sarcomatoid carcinoma is a biphasic tumor expressing both malignant mesenchymal (sarcomatoid) and epithelial (carcinomatous) components[1]. It can occur in various anatomical sites, most frequently in the head and neck, kidneys, and lungs. PSC is a very rare, poorly differentiated subtype of NSCLC, representing 0.1% to 0.4% of all lung malignancies[2]. According to the 2015 World Health Organization classification of lung tumors, PSC is sub-classified into five subtypes[4]: pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma, and pulmonary blastoma.
It is more common in men in their sixth decade of age[5]. It is linked to heavy smoking and asbestos exposure. Compared to conventional NSCLC, patients with PSC have shorter overall survival and higher recurrence rate. Distant metastasis appears more frequently than local relapse. Besides common metastatic sites for NSCLC, PSC also frequently metastasizes to the kidneys and gastrointestinal tract including the esophagus, small bowel, colon, and rectum[6].
Metastasizing to the oral cavity is uncommon, constituting 1%-3% of all oral malignancies[7]. Most metastases occur in the mandible, and oral soft tissue involvement is rare. The gingiva is the most frequent site for oral soft tissue metastases (57%), followed by the tongue (27%) and tonsils (8%). The most common cancers that metastasize to the oral cavity are tumors from the lung, breast, skin, gastrointestinal tract, liver, and male genitourinary tract[8]. Metastases of primary lung cancers to the tongue are rare, with an incidence varying between 0.2% to 1.6%[9]. In general, histologic analysis of primary lung cancers metastasizing to the oral cavity reveals adenocarcinoma or squamous-cell carcinoma.
Tongue metastasis usually present with a submucosal mass, commonly with intact overlying mucosa, but occasionally with ulceration or polypoid appearance. In one study[9], there were 12 cases of lingual metastases out of 5933 patients with different types of malignancies, with tongue base the most commonly affected site due to the relative immobility and rich vascular supply of lymphatics and blood. The tumor of our patient was submucosal, infiltrating the tongue muscles, and involving the tongue base, all of which are common features of metastasis.
Due to its rarity and lack of specific gross characteristics, at the time of detection, tongue metastasis may be mistakenly diagnosed as abscess, edema, or hemorrhage[8]. Common symptoms include pain, bleeding, discomfort, dysphagia, or dyspnea. Several imaging techniques, including ultrasonography, CT, and magnetic resonance imaging can be utilized for evaluation.
In our case, the patient presented with tongue swelling and associated dysphagia, odynophagia, and airway compromise. Clinically, it was initially considered an allergic reaction to her medication and later an abscess, while tongue metastasis was judged to be less likely. There were two factors that have compromised an initial accurate diagnosis. Firstly, the initial CT image could not be adequately viewed because of the artifacts from dental filling. The tongue lesion was only discovered on the following neck CT but not in the first one that was performed one week earlier. Secondly, the rapid progression of the disease, the presence of leukocytosis at presentation, and a history of recent invasive procedure to the adjacent anatomic area (injection for vocal cord paralysis), all of which place an acute pathologic process like abscess high on our list of differential diagnosis. Although clinical presentation with acute symptoms is uncommon for tongue tumors, it could occur due to necrosis or hemorrhage into the tumor. This case report provides two important lessons in patients presenting with space occupying lesions in unusual locations who already have pre-existing PSC. Firstly, accurate diagnosis by symptoms and image studies can be difficult, while pathology remains the most accurate diagnostic method. Secondly, the new lesion should be considered as the same pathologic process unless proven otherwise.
The literature on lung cancer metastasizing to the tongue is limited with only 12 cases reported from 1979 to 2020 (Table 1). Most primary pulmonary tumors were either squamous cell carcinoma or adenocarcinoma except for a single report of PSC. The patient was a 60-year-old man who had metastasis to the lateral border of the tongue two months after radical treatment for a spindle cell carcinoma, a subtype of PSC[10].
| Ref. | Year | Basic information | Tongue metastasis as the initial presentation | Symptoms on presentation | Tongue metastasis location | Lung cancer pathology | Tongue as the sole metastatic site | Treatment | Outcome after diagnosis of tongue metastasis |
| Lee et al[11] | 2018 | 63-yr-old; male; smoker | Yes | Dysphagia, painful tongue mass | Tip | Squamous cell carcinoma | Yes | Chemotherapy, tongue mass excision | Death after 8 mo |
| Cheng et al.[12] | 2017 | 56-yr-old; male; smoker | No | Painful tongue nodule without ulceration, hoarseness | Base | Squamous cell carcinoma | Yes | Chemotherapy | Death after 7 mo |
| Jeba et al[13] | 2016 | 45-yr-old; male; smoker | Yes | Tongue swelling without ulceration, dysarthria, dysphagia, hoarseness | Left anterior two-third, not crossing midline | Adenocarcinoma | No | Chemotherapy | Lost to follow-up |
| Ganesh et al[10] | 2014 | 60-yr-old; male; unknown smoking history | No | Tongue swelling, left earache | Left lateral border | Spindle cell carcinoma (sarcomatoid carcinoma) | Yes | Patient refused treatment | NA |
| Mavili et al[8] | 2010 | 58-yr-old; female; unknown smoking history | Yes | Painful tongue swelling, dyspnea | Right anterior | Adenocarcinoma | Yes | NA | Death after 2 mo |
| Wu et al[14] | 2009 | 36-yr-old; female; unknown smoking history | No | Dysarthria, tongue swelling with deviation to left | Base | Adenocarcinoma | No | Chemo/target therapy and radiation | Death after 3 mo |
| Hatoum et al[15] | 2008 | 63-yr-old; female; smoker | Yes | Painful tongue mass without ulceration, dysarthria, dysphagia | Entire right side, not involving the base | Adenocarcinoma | Yes | Chemotherapy | NA |
| Kurt et al[16] | 2006 | 57-yr-old; male; smoker | No | Painful tongue nodule without ulceration | Anterior | Squamous cell carcinoma | No | Chemotherapy | Lost to follow-up |
| Terashima et al[17] | 2004 | 63-yr-old; male; smoker | Yes | Painful tongue nodule without ulceration, dysarthria, dysphagia | Left side involving base and midline | Squamous cell carcinoma | No | Chemo-radiation | Death after 5 mo |
| Mui et al[18] | 1999 | 65-yr-old; male; smoker | Yes | Tongue foreign body sensation and pain with ulceration, dysphagia, intermittent blood-streaked saliva | Right posterolateral | Large cell carcinoma | No | Chemo-radiation | Death after 4 mo |
| Shehab et al[19] | 1994 | 70-yr-old; female; smoker | No | Tongue mass with ulceration | Right posterior one-third | Squamous cell carcinoma | No | Radiation | Death after 28 mo |
| Kim et al[20] | 1979 | 74-yr-old; male; unknown smoking history | Yes | Tongue mass | Left anterior two-third | Adenocarcinoma | Yes | Radiation | Death during treatment |
Surgical treatment of PSC is the main therapeutic strategy for resectable tumors. The effects of chemotherapy and radiotherapy are limited in advanced stages. MET mutation and PD-L1 overexpression are associated with a particular propensity for sarcomatoid carcinoma[21]. A higher frequency of MET exon 14 mutations has been reported in PSCs compared to other NSCLC, with a prevalence ranging between 22% and 32%[22,23]. Capmatinib is a highly selective MET inhibitor with antitumor activity in NSCLC. In May 2020, oral capmatinib received its first global approval in the United States for the treatment of metastatic NSCLC with MET exon 14 skipping mutation. Our patient was started on this new medication but failed to achieve a good response. PD-L1 is expressed in this type of tumors in 70%-90% of cases. There are several case reports demonstrating good response in PSC patients treated with immunotherapy[24,25], and our patient is now switched to combined chemo-immunotherapy.
Tongue metastasis from PSC is an uncommon phenomenon. To the best of our knowledge, the current case is the first case report in the literature of a primary pulmonary pleomorphic carcinoma metastasizing to the tongue and the second case report of tongue metastasis from PSC. A high index of suspicion for metastatic disease should be maintained in patients with a known history of PSC when tongue swelling or radiologic image indicating a lesion in the tongue, especially near the tongue base, is observed, and appropriate investigations should be undertaken.
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fang ZY S-Editor: Gao CC L-Editor: A P-Editor: Yuan YY
| 1. | Shen XZ, Liu F. Primary sarcomatoid carcinoma of the mandibular gingiva: clinicopathological and radiological findings. Singapore Med J. 2014;55:e152-e155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Yendamuri S, Caty L, Pine M, Adem S, Bogner P, Miller A, Demmy TL, Groman A, Reid M. Outcomes of sarcomatoid carcinoma of the lung: a Surveillance, Epidemiology, and End Results Database analysis. Surgery. 2012;152:397-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 165] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 3. | Ito H, Onizawa K, Satoh H. Non-small-cell lung cancer metastasis to the oral cavity: A case report. Mol Clin Oncol. 2017;6:422-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, Chirieac LR, Dacic S, Duhig E, Flieder DB, Geisinger K, Hirsch FR, Ishikawa Y, Kerr KM, Noguchi M, Pelosi G, Powell CA, Tsao MS, Wistuba I; WHO Panel. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol. 2015;10:1243-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2160] [Cited by in RCA: 3121] [Article Influence: 346.8] [Reference Citation Analysis (0)] |
| 5. | Mochizuki T, Ishii G, Nagai K, Yoshida J, Nishimura M, Mizuno T, Yokose T, Suzuki K, Ochiai A. Pleomorphic carcinoma of the lung: clinicopathologic characteristics of 70 cases. Am J Surg Pathol. 2008;32:1727-1735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary pleomorphic (spindle) cell carcinoma: peculiar clinicopathologic manifestations different from ordinary non-small cell carcinoma. Lung Cancer. 2001;34:91-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 135] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Kumar G, Manjunatha B. Metastatic tumors to the jaws and oral cavity. J Oral Maxillofac Pathol. 2013;17:71-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 8. | Mavili E, Oztürk M, Yücel T, Yüce I, Cağli S. Tongue metastasis mimicking an abscess. Diagn Interv Radiol. 2010;16:27-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Zegarelli DJ, Tsukada Y, Pickren JW, Greene GW Jr. Metastatic tumor to the tongue. Report of twelve cases. Oral Surg Oral Med Oral Pathol. 1973;35:202-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 61] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Ganesh A, Abraham S, Thomas S, Anila K. Radically treated carcinoma lung with early metastasis to the tongue: A case report and review of literature. Clin Cancer Investig J. 2014;3:530-532. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Lee S, Kim M, Won C. Lingual metastasis to the tip of the tongue as the first sign of metastatic spread in lung cancer: a case report and review of the literature. Korean J Otorhinolaryngol-Head Neck Surg. 2018;61:489-491. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Cheng X, Hu Z, Han YP, Bai C. A case report of tongue metastasis from lung squamous cell carcinoma and literature review. Medicine (Baltimore). 2017;96:e8208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Jeba J, Backianathan S, Ishitha G, Singh A. Oral and gastrointestinal symptomatic metastases as initial presentation of lung cancer. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Wu X, Li H, Wang Y, Fu Y. [A case report of tongue metastasis from lung carcinoma.]. Zhongguo Fei Ai Za Zhi. 2009;12:1217-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Hatoum HA, Habib JG, Tawil A, Chakhachiro Z, Otrock ZK, Husari A, Shamseddine A. Adenocarcinoma of the lung presenting as a metastatic tongue mass. South Med J. 2008;101:770-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Kurt M, Bulut N, Aksoy S, Kosemehmetoglu K, Kars A. Anterior tongue metastasis from lung cancer. South Med J. 2006;99:784-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Terashima T, Matsuzaki T, Kawada I, Nishida J, Tanaka Y, Morishita T, Takeyasu Y, Yamane GY, Uchiyama T. Tongue metastasis as an initial presentation of a lung cancer. Intern Med. 2004;43:727-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Mui S, Smith AE. Lingual metastasis as the initial presentation of a large cell lung carcinoma. Otolaryngol Head Neck Surg. 1999;121:305-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Shehab Z, Desousa S, Pahor AL. Metastasis in tongue from carcinoma of bronchus: a case report. J Laryngol Otol. 1994;108:1099-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Kim RY, Perry SR, Levy DS. Metastatic carcinoma to the tongue: a report of two cases and a review of the literature. Cancer. 1979;43:386-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Boland JM, Mansfield AS, Roden AC. Pulmonary sarcomatoid carcinoma-a new hope. Ann Oncol. 2017;28:1417-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Tong JH, Yeung SF, Chan AW, Chung LY, Chau SL, Lung RW, Tong CY, Chow C, Tin EK, Yu YH, Li H, Pan Y, Chak WP, Ng CS, Mok TS, To KF. MET Amplification and Exon 14 Splice Site Mutation Define Unique Molecular Subgroups of Non-Small Cell Lung Carcinoma with Poor Prognosis. Clin Cancer Res. 2016;22:3048-3056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 352] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 23. | Liu X, Jia Y, Stoopler MB, Shen Y, Cheng H, Chen J, Mansukhani M, Koul S, Halmos B, Borczuk AC. Next-Generation Sequencing of Pulmonary Sarcomatoid Carcinoma Reveals High Frequency of Actionable MET Gene Mutations. J Clin Oncol. 2016;34:794-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 260] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 24. | Kanazu M, Uenami T, Yano Y, Nakatsubo S, Hosono Y, Ishijima M, Akazawa Y, Yamaguchi T, Urasaki K, Mori M, Yokota S. Case series of pleomorphic carcinomas of the lung treated with nivolumab. Thorac Cancer. 2017;8:724-728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 25. | Senoo S, Ninomiya T, Makimoto G, Nishii K, Kano H, Watanabe H, Hata Y, Kubo T, Tanaka T, Hotta K, Maeda Y, Kiura K. Rapid and Long-term Response of Pulmonary Pleomorphic Carcinoma to Nivolumab. Intern Med. 2019;58:985-989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |