Published online Nov 24, 2019. doi: 10.5306/wjco.v10.i11.369
Peer-review started: May 20, 2019
First decision: August 2, 2019
Revised: September 4, 2019
Accepted: September 25, 2019
Article in press: September 25, 2019
Published online: November 24, 2019
Processing time: 192 Days and 17.1 Hours
Infiltration of the breast by leukemic cells is uncommon but may manifest as an oncological emergency requiring prompt management. Extramedullary relapse of T-cell acute lymphoblastic leukemia (T-ALL) within the breast is exceedingly rare and there is paucity of data in the literature regarding this entity. No consensus exists on management of isolated extramedullary breast relapses of T-ALL. Herein, we report a case of isolated extramedullary breast relapse of T-ALL treated with breathing adapted radiation therapy (BART) using the active breathing control (ABC) system.
The patient was a 33-year-old female with diagnosis of T-ALL. She received intensive systemic chemotherapy that resulted in complete remission of her disease, and then underwent allogeneic hematopoietic stem cell transplantation. After a 15 mo period without symptoms and signs of progression, the patient presented with palpable masses in both breasts. She complained from severe pain and swelling of the breasts. Imaging workup showed bilateral breast lesions, and diagnosis of breast infiltration by leukemic cells was confirmed after immunohistopathological evaluation. The patient suffering from severe pain, discomfort, and swelling of both breasts due to leukemic infiltration was referred to the Radiation Oncology Department for symptomatic palliation. Whole breast irradiation was delivered to both breasts of the patient with BART using the ABC system. The patient had complete resolution of her symptoms after treatment with BART.
BART with the ABC system resulted in complete resolution of the patient’s symptoms due to leukemic infiltration of both breasts with T-ALL. This contemporary treatment technique should be preferred for radiotherapeutic management of patients with leukemic infiltration of the breasts to achieve effective symptomatic palliation.
Core tip: Although exceedingly rare, leukemic infiltration of the breasts by T-cell acute lymphoblastic leukemia (T-ALL) may manifest as an oncological emergency requiring prompt management. In this case report, we present the first case in the literature treated by breathing adapted radiation therapy using the active breathing control system for management of isolated extramedullary relapse of T-ALL in both breasts.
- Citation: Sager O, Dincoglan F, Demiral S, Uysal B, Gamsiz H, Ozcan F, Colak O, Elcim Y, Dirican B, Beyzadeoglu M. Breathing adapted radiation therapy for leukemia relapse in the breast: A case report. World J Clin Oncol 2019; 10(11): 369-374
- URL: https://www.wjgnet.com/2218-4333/full/v10/i11/369.htm
- DOI: https://dx.doi.org/10.5306/wjco.v10.i11.369
A considerable proportion of patients with leukemia suffer from relapse during the course of their disease, mostly in the bone marrow[1]. The central nervous system and testes are frequent locations and sanctuary sites for extramedullary relapses. Involvement of the breast by leukemia is uncommon but may manifest as an oncological emergency requiring prompt management[2-4]. Acute myeloid leukemia constitutes the most common type of acute leukemia in adults, and is also the most common type infiltrating the breasts. Isolated extramedullary relapse of T-cell acute lymphoblastic leukemia (T-ALL) within the breast is exceedingly rare and there is paucity of data in the literature regarding this entity[5-7]. No consensus exists on management of isolated extramedullary breast relapses of T-ALL. Herein, we report a case of isolated extramedullary breast relapse of T-ALL treated with breathing adapted radiation therapy (BART) using the active breathing control (ABC) system.
The patient was a 33-year-old female with diagnosis of T-ALL. Initial laboratory data showed increased leukocyte count of 105 × 109 per liter (L), decreased hemoglobin level of 7.8 mg per deciliter (mg/dL), and decreased platelet count of 28 × 109/L. She received intensive systemic chemotherapy including L-asparaginase, prednisone, vincristine, and intrathecal methotrexate, hydrocortisone, and cytosine arabinoside, which resulted in complete remission of her disease, and then underwent allogeneic hematopoietic stem cell transplantation. After a 15 mo period without symptoms and signs of progression, the patient presented with palpable masses in both breasts. She complained from severe pain and swelling of the breasts.
Polymerase chain reaction analysis of bone marrow aspirates demonstrated complete allogeneic hematopoietic chimerism, and there were no leukemic lesions at other sites including the bone marrow and cerebrospinal fluid. Imaging workup included bilateral mammography, doppler ultrasonography and breast magnetic resonance imaging (MRI). On ultrasonography, lesions were detected in the upper inner quadrant of the right breast with mixed echo and significant hyperechogenicity. Another lesion was detected in the left breast with mixed echo and significant hyperechogenicity. Doppler ultrasonographic assessment showed vascularization in these breast lesions. Diffusion-weighted and dynamic contrast-enhanced breast MRI revealed significant diffusion restriction and type 2 and 3 contrast patterns. Lesion on the right breast was heterogeneously hypointense with contrast enhancement. The lesion in the left breast also showed contrast enhancement, and was hypointense on T1 weighted sequencing, and hyperintense on fat suppressed MRI.
The patient was referred for biopsy, and diagnosis of breast infiltration by leukemic cells was confirmed after immunohistopathological evaluation. Immun-ohistopathological assessment revealed presence of small to medium size lymphoblastic cells with narrow cytoplasm and hyperchromatic nuclei. Atypical cells were positive for terminal deoxynucleotidyl transferase, cluster of differentiation 3 (CD3), CD5, and CD34 on immunohistochemical analysis. Paired box gene 5 was weakly positive. Myeloperoxidase, CD10, CD117, and CD20 were negative. The Ki-67 proliferation index was 40%.
After multidisciplinary expert consultation, the patient suffering from severe pain, discomfort, and swelling of both breasts due to leukemic infiltration was referred to the Radiation Oncology Department for symptomatic palliation.
Whole breast irradiation was delivered to both breasts of the patient with BART using the ABC system (Elekta, United Kingdom). Total radiation dose was 50 Gy delivered in 25 daily 2-Gy fractions over 5 wk. The patient was trained for compliance with the ABC system before computed tomography (CT) simulation as per our institutional protocol[8]. Reproducible moderate deep inspiration breath holding (mDIBH) by use of the ABC system has been achieved after the training session, and planning CT images were acquired at the CT-simulator (GE Lightspeed RT, GE Healthcare, Chalfont St. Giles, United Kingdom) at mDIBH. A breast board was used for reproducible positioning and immobilization of the patient at each treatment fraction. After acquisition of the planning CT images, three-dimensional image data sets were transferred to the contouring workstation via the network. Delineation of both breast target volumes and critical organs including the spinal cord, heart, and lungs was performed at the Advantage Sim MD simulation and localization software (Advantage SimMD, GE, United Kingdom). Structure sets including the contoured target volumes and critical organs were sent to the treatment planning workstation. Radiation treatment planning for whole breast irradiation of both breasts was performed by using PrecisePLAN treatment planning system (PrecisePLAN, Elekta, United Kingdom). BART was delivered at the linear accelerator (Synergy, Elekta, United Kingdom) under image guidance for setup verification using electronic portal imaging device (Iview, Elekta, United Kingdom) and kilo-voltage cone beam CT (X-ray volumetric imaging, Elekta, United Kingdom).
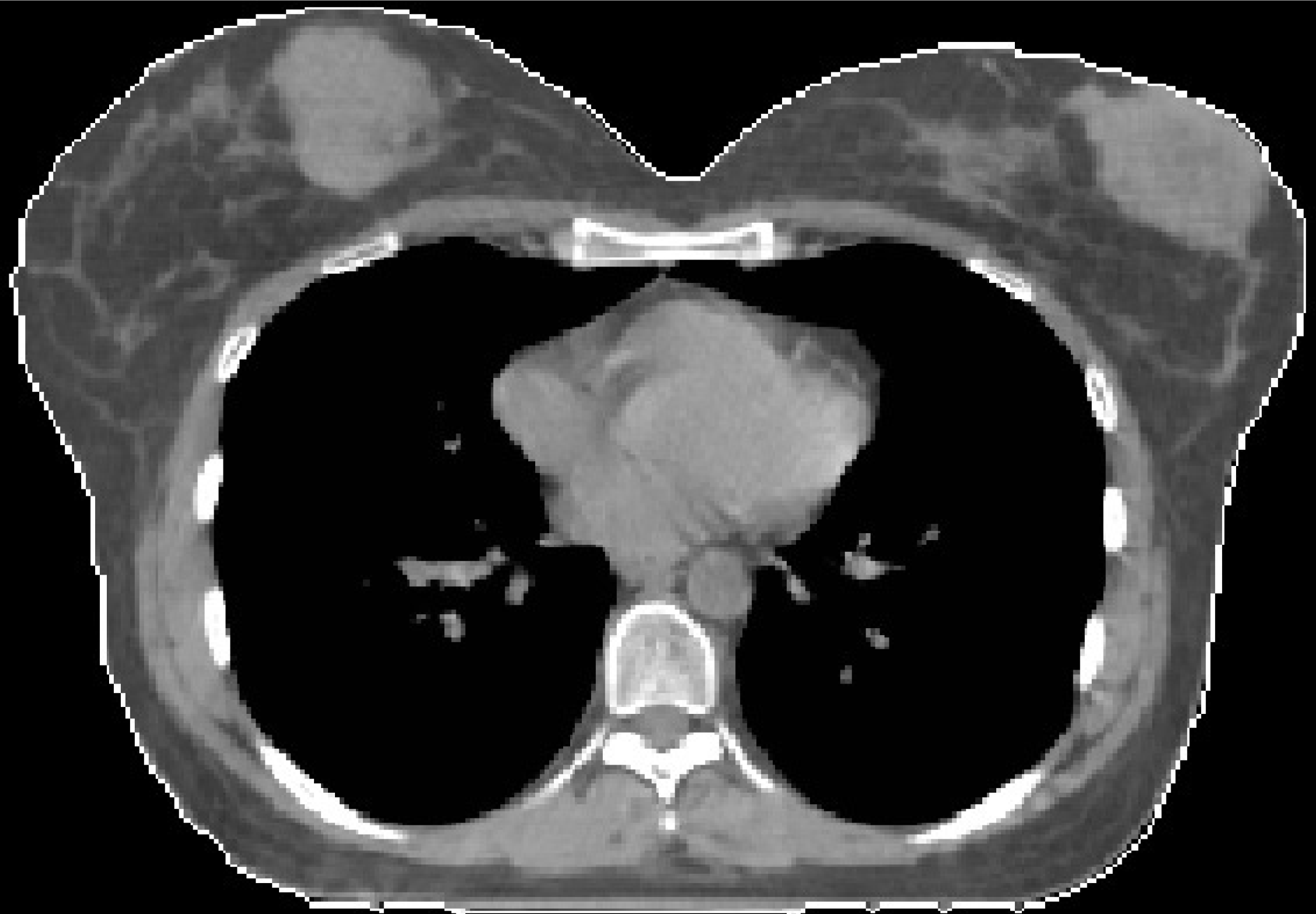
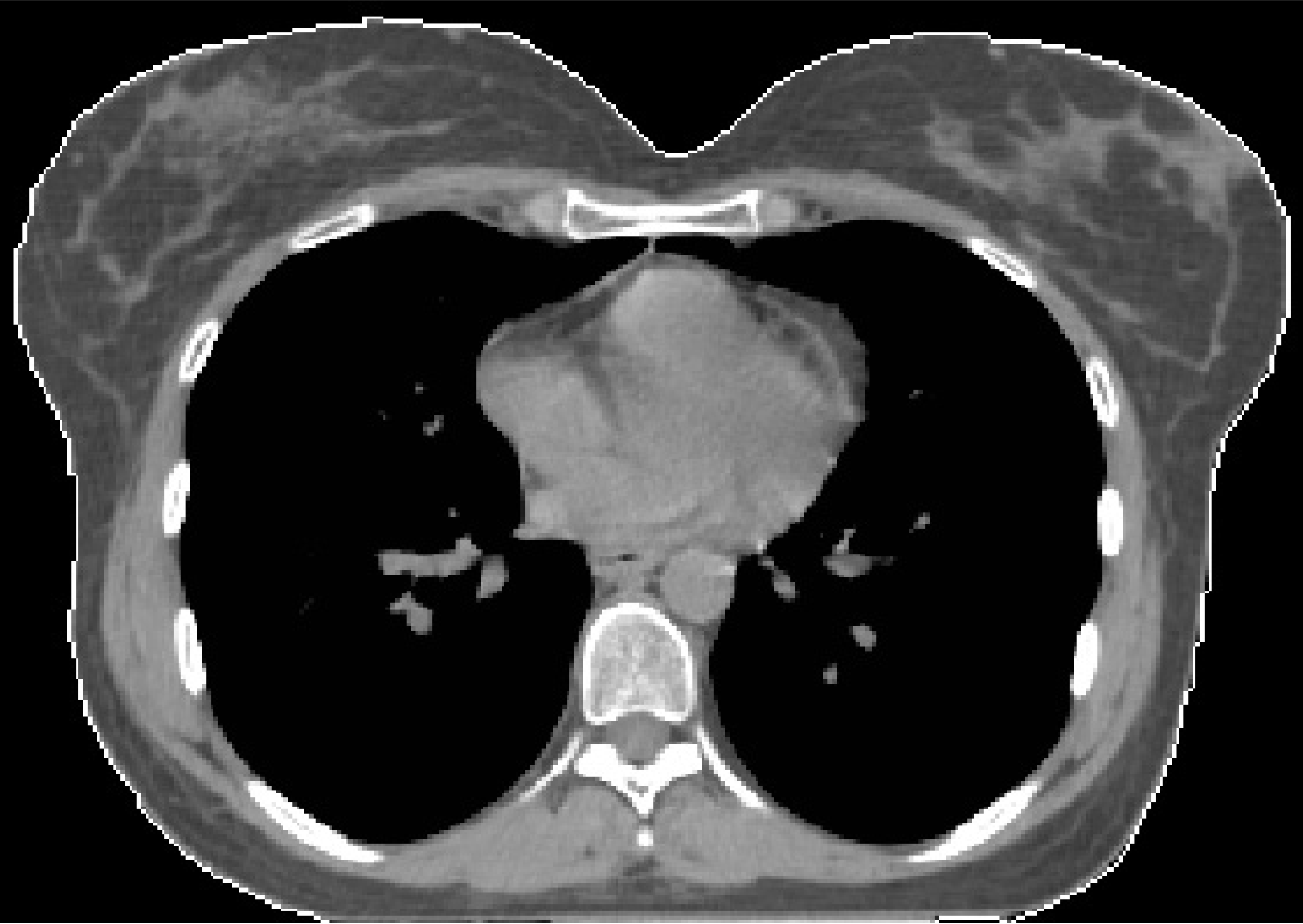
Compliance of the patient with treatment procedure was excellent and there was no need for any treatment breaks. The patient had complete resolution of her symptoms after treatment with BART. The timeline of the disease course is shown in Table 1. Axial CT images of the patient before and after treatment with BART are shown in Figures 1 and 2, respectively.
| Timeline of the disease course | |
| Initial diagnosis of T-ALL | May 2017 |
| Complete remission after chemotherapy | July 2017 |
| Allogeneic hematopoietic stem cell transplantation | August 2017 |
| Presentation with palpable masses in both breasts | November 2018 |
| Diagnosis of extramedullary breast relapse of T-ALL | December 2018 |
| Bilateral whole breast irradiation with BART using ABC | January 2019 |
| Complete resolution of symptoms and breast lesions | February 2019 |
There is paucity of data regarding extramedullary relapse of ALL in the breast. Although rare, extramedullary relapse should be vigilantly considered in differential diagnosis of a breast lump when a history of leukemia is present[9,10].
As a local treatment modality, radiation therapy has been judiciously used for management of extramedullary leukemia relapse in sanctuary sites such as the CNS and testes[11-13]. Regarding isolated extramedullary relapses of ALL within the breast, there is no consensus on standard management. Nevertheless, complete resolution of breast lesions by use of irradiation has also been reported in other studies consistent with our findings[14-16]. Future trials are clearly needed to shed light on optimal management of isolated extramedullary relapses of ALL in the breast.
Extramedullary relapse of T-ALL in the breast is exceedingly rare. To the best of our knowledge, management of leukemic infiltration of both breasts by T-ALL by use of BART has not been previously addressed in the literature. BART has been the primary mode of radiotherapeutic management of breast cancer in our department given the reported dosimetric benefits and significantly improved normal tissue sparing with incorporation of breath holding at moderate deep inspiration during treatment simulation and delivery[8,17,18].
Briefly, mDIBH with the ABC system was developed for management of respiratory motion for thoracoabdominal tumors and has been used for this purpose in both conventionally fractionated radiotherapy regimens and Stereotactic Body Radiation Therapy applications[8,17-21]. In addition to respiratory motion management, an additional benefit of mDIBH with the ABC system for breast cancer includes minimizing exposure of the heart particularly for left-sided breast cancer patients along with improved sparing of other critical organs, which has been supported in previous studies[8,17,18].
Given the benefits of BART, this contemporary technique was adapted for management of our patient with bilateral breast lesions and led to complete resolution of her symptoms. Bilateral whole breast irradiation using BART for leukemic infiltration of both breasts with T-ALL has not been subject to any previous reports. However, there is no standard management in the setting of leukemic infiltration of both breasts with T-ALL, and treatment decisions regarding management of this exceedingly rare entity are individualized based on patient and tumor characteristics along with institutional experiences. Incorporation of contemporary techniques such as BART at mDIBH with the ABC system may offer improved radiotherapeutic management of these patients, particularly in the setting of bilateral breast irradiation.
BART with the ABC system resulted in complete resolution of the patient’s symptoms due to leukemic infiltration of both breasts with T-ALL. This contemporary treatment technique should be preferred for radiotherapeutic management of patients with leukemic infiltration of the breasts to achieve effective symptomatic palliation.
Manuscript source: Invited manuscript
Specialty type: Oncology
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Demonacos C, Gabriel S S-Editor: Ma RY L-Editor: Filipodia E-Editor: Liu MY
| 1. | Savaşan S, Abella E, Karanes C, Ravindranath Y. Recurrent breast relapses in a patient with acute lymphoblastic leukaemia following allogeneic bone marrow transplantation. Acta Haematol. 1998;99:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Aslan H, Pourbagher A. Breast Involvement by Hematologic Malignancies: Ultrasound and Elastography Findings with Clinical Outcomes. J Clin Imaging Sci. 2017;7:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Glazebrook KN, Zingula S, Jones KN, Fazzio RT. Breast imaging findings in haematological malignancies. Insights Imaging. 2014;5:715-722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Surov A, Wienke A, Abbas J. Breast leukemia: an update. Acta Radiol. 2012;53:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Demirsoy ET, Atesoglu EB, Tarkun P, Gedük A, Erdem BE, Hacihanefioglu A, Erçin MC. Isolated Breast Relapse of Acute Lymphoblastic Leukemia After Allogeneic Hematopoietic Stem Cell Transplantation. Indian J Hematol Blood Transfus. 2016;32:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Liu B, Liu B, Wang X, Guo L, Liu X, Han W, Dong L, Liu M. Complete response of extramedullary relapse in breast of acute T lymphoblastic leukemia after bone marrow transplantation to chemoradiotherapy: a case report and literature review. BMC Cancer. 2016;16:875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Bayrak IK, Yalin T, Ozmen Z, Aksoz T, Doughanji R. Acute lymphoblastic leukemia presented as multiple breast masses. Korean J Radiol. 2009;10:508-510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Dincoglan F, Beyzadeoglu M, Sager O, Oysul K, Kahya YE, Gamsiz H, Uysal B, Demiral S, Dirican B, Surenkok S. Dosimetric evaluation of critical organs at risk in mastectomized left-sided breast cancer radiotherapy using breath-hold technique. Tumori. 2013;99:76-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 9. | Besina S, Rasool Z, Samoon N, Akhtar OS. Acute lymphoblastic leukemia presenting as a breast lump: A report of two cases. J Cytol. 2013;30:201-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Shin HC. Relapse of Biphenotypic Acute Leukemia as a Breast Mass. J Breast Cancer. 2016;19:455-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Locatelli F, Schrappe M, Bernardo ME, Rutella S. How I treat relapsed childhood acute lymphoblastic leukemia. Blood. 2012;120:2807-2816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 222] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 12. | Tombolini V, Banelli E, Capua A, Giona F, Vitturini A. Radiation treatment of testicular relapse in acute lymphoblastic leukemia. Acta Radiol Oncol. 1986;25:29-32. [PubMed] |
| 13. | Pinnix CC, Yahalom J, Specht L, Dabaja BS. Radiation in Central Nervous System Leukemia: Guidelines From the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys. 2018;102:53-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Chim CS, Shek TW, Liang R. Isolated relapse of acute lymphoblastic leukemia in the breast masquerading as gynecomastia. Am J Med. 2000;108:677-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Driss M, Salem A, Mrad K, Abbes I, Sassi S, Ben Romdhane K. Acute lymphoblastic leukemia relapse in the breast: fine needle aspiration diagnosis of a rare presentation. Acta Cytol. 2010;54:361-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Sung PH, Im C, Hyun SY, Shim KY, Lee JI, Kong JH. Unusual isolated extramedullary relapse of acute lymphoblastic leukemia in the breast despite complete donor hematopoietic chimerism after allogeneic hematopoietic stem cell transplantation. Korean J Intern Med. 2018;33:218-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Kunheri B, Kotne S, Nair SS, Makuny D. A dosimetric analysis of cardiac dose with or without active breath coordinator moderate deep inspiratory breath hold in left sided breast cancer radiotherapy. J Cancer Res Ther. 2017;13:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Remouchamps VM, Vicini FA, Sharpe MB, Kestin LL, Martinez AA, Wong JW. Significant reductions in heart and lung doses using deep inspiration breath hold with active breathing control and intensity-modulated radiation therapy for patients treated with locoregional breast irradiation. Int J Radiat Oncol Biol Phys. 2003;55:392-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 293] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 19. | Sager O, Beyzadeoglu M, Dincoglan F, Oysul K, Kahya YE, Gamsiz H, Uysal B, Demiral S, Dirican B, Surenkok S. Evaluation of active breathing control-moderate deep inspiration breath-hold in definitive non-small cell lung cancer radiotherapy. Neoplasma. 2012;59:333-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Gamsiz H, Beyzadeoglu M, Sager O, Demiral S, Dincoglan F, Uysal B, Onal E, Dirican B. Evaluation of stereotactic body radiation therapy in the management of adrenal metastases from non-small cell lung cancer. Tumori. 2015;101:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Gamsiz H, Beyzadeoglu M, Sager O, Dincoglan F, Demiral S, Uysal B, Surenkok S, Oysul K, Dirican B. Management of pulmonary oligometastases by stereotactic body radiotherapy. Tumori. 2014;100:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |