Published online Feb 15, 2018. doi: 10.4291/wjgp.v9.i1.1
Peer-review started: April 10, 2017
First decision: May 26, 2017
Revised: July 5, 2017
Accepted: October 30, 2017
Article in press: October 30, 2017
Published online: February 15, 2018
Processing time: 309 Days and 8.3 Hours
Acute cholangitis is bacterial infection of the extra-hepatic biliary system. As it is caused by gallstones blocking the common bile duct in most of the cases, its prevalence is greater in ethnicities with high prevalence of gallstones. Biliary obstruction of any cause is the main predisposing factor. Diagnosis is established by the presence of clinical features, laboratory results and imaging studies. The treatment modalities include administration of intravenous fluid, antibiotics, and drainage of the bile duct. The outcome is good if the treatment is started early, otherwise it could be grave.
Core tip: Acute cholangitis is a serious medical problem unless treated early. High clinical suspicion is essential to diagnose this condition. The different diagnostic criteria, treatment options, including different modalities of biliary drainage, and prognosis are described in this article.
- Citation: Ahmed M. Acute cholangitis - an update. World J Gastrointest Pathophysiol 2018; 9(1): 1-7
- URL: https://www.wjgnet.com/2150-5330/full/v9/i1/1.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v9.i1.1
Acute cholangitis is a clinical entity caused by bacterial infection of the biliary system, most commonly secondary to partial or complete obstruction of the bile duct or hepatic ducts. The diagnosis is established by the characteristic clinical symptoms and signs of infection, abnormal laboratory studies suggestive of infection and biliary obstruction, and abnormal imaging studies suggestive of biliary obstruction[1]. The main importance of this condition is that it is a very treatable condition if treated appropriately, but the mortality can be high if there is delay in treatment. There are other varieties of cholangitis, which include primary biliary cholangitis, primary sclerosing cholangitis, IgG4-related autoimmune cholangitis and recurrent pyogenic cholangitis or Oriental cholangiohepatitis[2]. We will be exclusively discussing here acute bacterial cholangitis, also called ascending cholangitis. The term ascending cholangitis comes from the migration of bacteria from the duodenum into the common bile duct. But, rarely, translocation of bacteria from the portal vein into the bile duct can also occur.
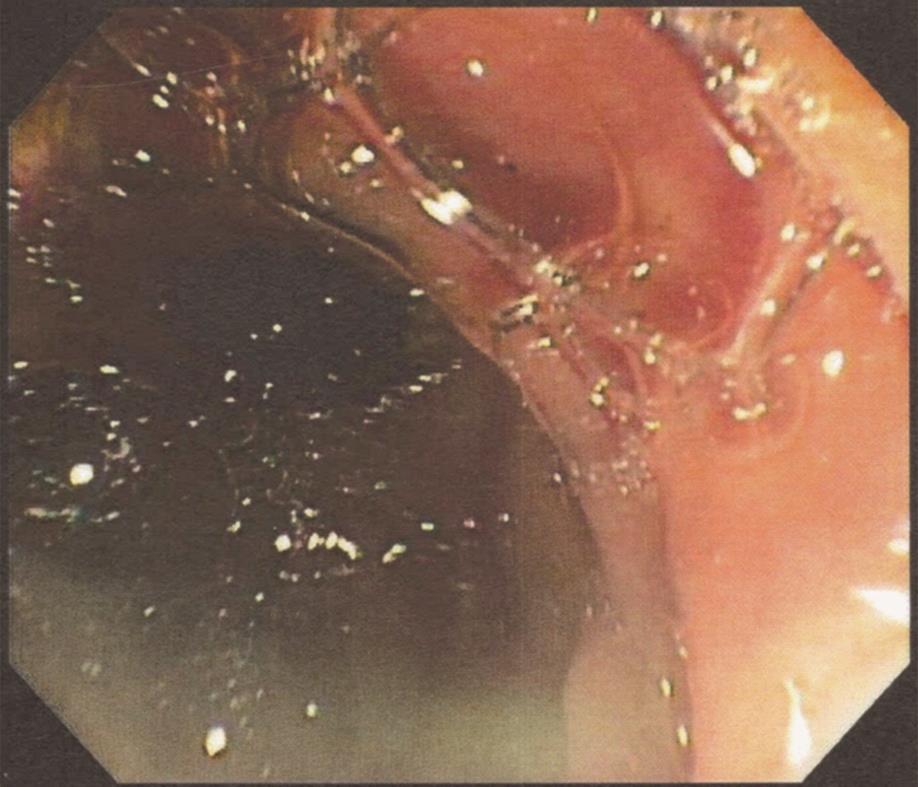
The biliary obstruction is most commonly caused by choledocholithiasis. Other causes of obstruction include benign or malignant stricture of the bile duct or hepatic ducts, pancreatic cancer, ampullary adenoma or cancer, porta hepatis tumor or metastasis, biliary stent obstruction (due to microbial biofilm formation, biliary sludge deposition and duodenal reflux of food content), primary sclerosing cholangitis, amyloid deposition in the biliary system[3], Mirizzi syndrome (gallstone impacted in cystic duct or neck of the gall bladder causing compression on common bile duct or common hepatic duct), Lemmel’s syndrome (peri-ampullary diverticulum causing distal biliary obstruction), round worm (Ascaris lumbricoides) or tapeworm (Taenia saginata) infestation of the bile duct[4], acquired immunodeficiency syndrome (commonly known as AIDS) cholangiopathy and strictured bilioenteric anastomoses[5]. Choledochocele and narrow-caliber bile duct are other risk factors for acute cholangitis. Recently, there was an outbreak of cholangitis due to carbapenem-resistant Enterobacteriaceae (CRE) as a result of exposure to contaminated duodenoscope[6]. Post-endoscopic retrograde cholangiopancreatography (ERCP) acute cholangitis can occur in 0.5% to 2.4% cases (Figure 1)[7]. As cholelithiasis is the most important risk factor, the same risk factors may play important roles in the development of acute cholangitis, particularly high fat (triglyceride) intake, sedentary life styles, obesity and rapid weight loss. Heavy alcohol consumption may lead to cirrhosis of the liver, which is a risk factor for gallstone formation.
The prevalence of cholelithiasis varies in different ethnicities. Gallstones are found in 10% to 15% of the white population in the United States. It is much more prevalent in native Americans (60%-70%) and Hispanics but less common in Asians and African Americans[8]. Many patients get admitted to the hospital with gallstone disease and 6% to 9% of them are diagnosed with acute cholangitis[9]. Males and females are equally affected. The average age of patients presenting with acute cholangitis is 50 to 60 years. Less than 200000 cases of cholangitis occur per year in the United States.
Biliary obstruction is an important factor in the pathogenesis of cholangitis. When bile flow occurs, presence of bacteria in the bile is not that significant because bacterial concentration does not increase and the intraductal pressure does not increase. Normally, there are different defensive mechanisms to prevent cholangitis. The bile salts have bacteriostatic activity and the biliary epithelium secretes IgA and mucous which probably act as anti-adherent factors. Kupffer cells on the biliary epithelium and the tight junction between the cholangiocytes prevent translocation of bacteria from the hepatobiliary system into the portal venous system. Normal bile flow flushes out any bacteria into the duodenum.
The sphincter of Oddi also prevents any migration of bacteria from the duodenum into the biliary system. In case of biliary obstruction, bile becomes stagnant in the biliary system, the intraductal pressure increases, the tight junction between cholangiocytes widen, Kupffer cells malfunction and the production of IgA is decreased[10]. “Choledochal pressure” plays an important role in the pathogenesis of acute cholangitis. The normal biliary ductal pressure is 7 to 14 cm of water (H2O). When the intraductal pressure exceeds 25 cm of H2O, cholangiovenous and cholangiolymphatic reflux can occur, leading to bacteremia and endotoxinemia[11]. Besides this, systemic release of inflammatory mediators like tumor necrosis factor (TNF), soluble TNF receptors, interleukin (IL)-1, IL-6 and IL-10 leads to profound hemodynamic compromise.
The most frequently found pathogens isolated in acute cholangitis are coliform organisms[12,13]. These include Escherechia coli (25%-50%), Klebsiella species (15%-20%), Enterococcus species (10%-20%) and Enterobacter species (5%-10%). Sometimes, anaerobic bacteria like Bacteroids fragilis and Clostridium perfringens can also cause acute cholangitis, particularly in patients with previous biliary surgery and in the elderly population[14]. Parasitic infestation of the biliary system by the liver flukes Clonorchis sinensis, Opisthorchis viverrini and Opisthorchis felineus and the roundworm Ascaris lumbricoides may lead to cholangitis[15].
The presentation depends on the severity of cholangitis. Classically, patients present with high fever persisting for more than 24 h, abdominal pain and jaundice (Charcot’s triad or hepatic fever). The right upper quadrant abdominal pain is generally mild. When the cholangitis becomes more severe, patients become hypotensive and confused (Reynold’s pentad). Charcot’s triad has low sensitivity (26.4%) and high specificity (95.9%). Although the presence of Charcot’s triad is suggestive of acute cholangitis, it is not diagnostic. Charcot’s triad is present in 26.4% to 72% of patients with acute cholangitis[16].
To improve the sensitivity of Charcot’s triad, TG07 diagnostic criteria for acute cholangitis was made at the International Consensus Meeting held in Tokyo in 2006. TG07 criteria included: A: Clinical: (1) history of biliary disease; (2) fever and/or chills; (3) jaundice; and (4) abdominal pain (RUQ or epigastric); B: Lab data: (5) evidence of inflammatory response; (6) abnormal liver function tests; C: Imaging findings: (7) biliary dilatation or evidence of an etiology (stone, stricture, stent, etc.). Suspected diagnosis: 2 or more items in A. Definite diagnosis: (1) Charcot’s triad (2 + 3 + 4); and (2) two or more items in A plus both items in B plus item C.
The sensitivity and specificity of diagnosing acute cholangitis in TG07 were 82.6% and 79.8% respectively. In 2012, TG13, a new Tokyo guideline for the diagnosis of acute cholangitis was published[17]. The criteria included: (1) Systemic inflammation: A-1: Fever (body temperature > 38 °C and/or shaking chills; A-2: Lab data: Evidence of inflammatory response – white blood cell (WBC) count < 4000/cmm or > 10000/cmm, C-reactive protein (CRP) - ≥ 1 mg/dL; and (2) Cholestasis: B-1: Jaundice-total bilirubin ≥ 2 mg/dL; B-2: Lab data: Abnormal liver function tests. Alkaline phosphatase (IU) > 1.5 × upper limit of normal; Gamma-glutamyl transpeptidase (IU) > 1.5 × upper limit of normal; Aspartate aminotransferase (IU) > 1.5 × upper limit of normal; Alanine aminotransferase (IU) > 1.5 × upper limit of normal. Imaging: C-1: Biliary dilatation; C-2: Evidence of etiology on imaging (stricture, stone stent, etc.).
Suspected diagnosis: One item in A + one item in either B or C. Definite diagnosis: One item in A, one item in B and one item in C. The sensitivity of diagnosing acute cholangitis improved to 91.8% but the specificity remained similar (77.7%) in TG13. The false positive rate of diagnosing acute cholecystitis also decreased to 5.9% in TG13 in comparison to Charcot’s triad (11.9%) and TG07 (15.5%).
Physical examination may show high temperature, tachycardia, hypotension, jaundice, right upper quadrant or epigastric tenderness and altered mental status.
Severity of acute cholangitis: two clinical factors determine the severity of acute cholangitis: (1) response to initial medical treatment; and (2) organ dysfunction[1].
Grade I is mild acute cholangitis. Patients do not have any organ dysfunction and do not meet the criteria of moderate acute cholangitis. They respond to the initial antibiotic treatment.
Grade II is moderate acute cholangitis. Patients do not have any organ dysfunction and do not respond to the initial antibiotic treatment. Any two of the five conditions should be present: (1) leukocytosis (WBC > 12000/cmm) or leukopenia (WBC < 4000/cmm); (2) high temperature (≥ 39 °C); (3) elderly (age > 75 years); (4) hyperbilirubinemia (total bilirubin ≥ 5 mg/dL); and (5) hypoalbuminemia (< 0.7 × lower limit of normal).
Grade III is severe acute cholangitis. Patients do not respond to initial medical treatment and have organ dysfunction in at least one of the following organs/systems: (1) cardiovascular system: hypotension requiring dopamine infusion ≥ 5 μg/kg per minute, or any dose of norepinephrine; (2) nervous system: disturbance of consciousness; (3) respiratory system: PaO2/FiO2 ratio < 300; (4) renal system: oliguria, serum creatinine > 2 mg/dL; (5) hepatic system: platelet-international normalized ratio (INR) > 1.5; and (6) hematological system: platelet count < 100000/cmm.
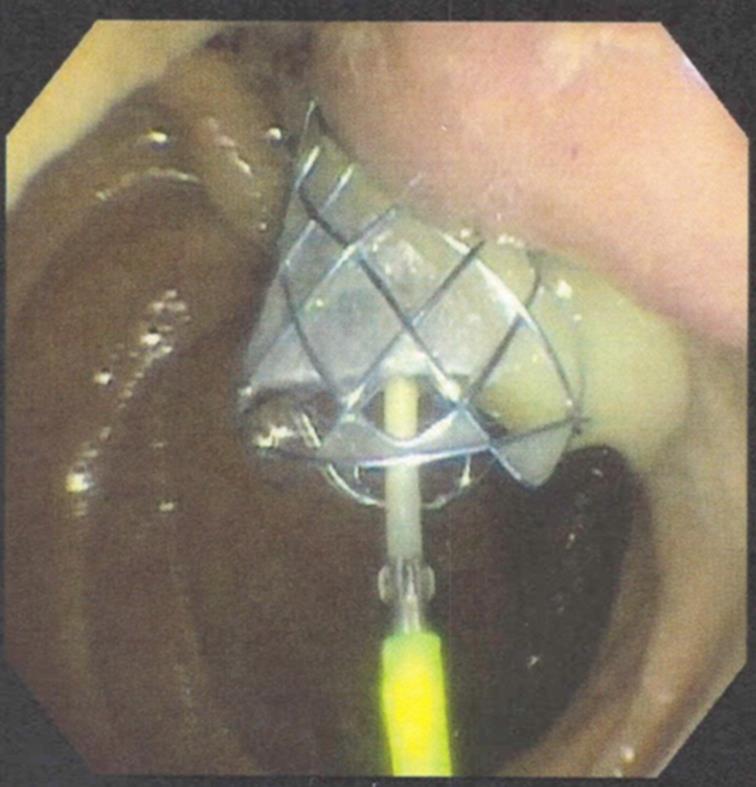
Sometimes we make the diagnosis of acute suppurative cholangitis (ASC) when we notice pus extruding from the ampulla of Vater during ERCP (Figures 1 and 2). ASC does not always mean severe acute cholangitis. Sometimes, patients with severe acute cholangitis do not have pus in the bile duct, and sometimes patients with ASC are not that sick[18]. Severe acute cholangitis or toxic cholangitis is present in 5% of all cases of cholangitis[19].
Differential diagnoses of acute cholangitis[20]: (1) acute cholecystitis; (2) cirrhosis of liver; (3) acute hepatitis; (4) liver abscess; (5) septic shock due to any cause; (6) right sided diverticulitis; and (7) righted sided pyelonephritis.
Recurrent acute cholangitis can occur when pigment stone is formed in the intrahepatic ducts leading to stricture formation, mainly in the lateral segment of the left lobe or posterior segment of the right lobe[21]. This condition is also called oriental cholangiohepatitis as it occurs almost exclusively in the natives of Southeast Asia. The exact mechanism is not known but related to malnutrition, ascariasis (Ascaris Lumbricoides) and clonorchiasis (Clonorchis sinensis). Transient portal bacteremia allows entrance of bacteria (E. coli, Klebsiella, Pseudomona, Proteus, anaerobes) into the biliary system, initiating a vicious cycle of infection and stone formation[22]. This condition may cause cholangiocarcinoma in 5% of cases.
Lab tests should include complete blood count, erythrocyte sedimentation rate or CRP, complete metabolic profile including renal and hepatic function, prothrombin time and INR. Blood culture should be done as early as possible. TG13 guideline also recommends collection of bile sample during the drainage procedure. Bile culture can be positive in 59% to 93% of acute cholangitis cases.
Imaging studies may include ultrasound of the abdomen, regular or helical computed tomography (CT), magnetic resonance cholangiopancreaticography (MRCP) and endoscopic ultrasound (EUS). CT without contrast is more sensitive than abdominal ultrasound in detecting common bile duct stones[23]. Among these, MRCP (82.2% accuracy in detecting choledocholithiasis) and EUS (96.9% accuracy in detecting choledocholithiasis) are the most sensitive imaging modalities, which can detect the level and cause of biliary obstruction[24]. Transabdominal ultrasound is able to detect choledocholithiasis in 30% of cases, and CT in 42% of cases. Although MRCP is being increasingly used in the setting of acute cholangitis, its sensitivity in detecting less than 6 mm stone is low[11].
Patients with cholangitis should be managed at the hospital, as this is considered as an emergent condition. Patients should be resuscitated first. As cholangitis is due to infection and obstruction of the biliary system, we have to treat both aspects. Intravenous fluid and antibiotics should be started as soon as possible. Fresh frozen plasma or vitamin K may be required for correction of coagulopathy. The choice of antibiotics depends on multiple factors, including the patient’s renal function, hepatic function, drug allergies, comorbidities, hospital-acquired (multiple or resistant organisms like Pseudomonas, CRE, vancomycin-resistant enterococcus or methicillin-resistant Staphylococcus aureus) or community-acquired infection (single agent like E. coli, Klebsiella, or Enterococcus), and also on the severity of cholangitis. The empiric antibiotics should cover both Gram-negative and anaerobic organisms. The initial choice should be piperacillin-tazobactam, ticarcillin-clavulanate, ceftriaxone plus metronidazole or ampicillin-sulbactam. If the patient is sensitive to penicillin, ciprofloxacin plus metronidazole, carbapenems or gentamicin plus metronidazole are good choices[25]. The antibiotics should be further evaluated and adjusted according to the blood culture results. Blood culture is positive in 21% to 71% of cases of acute cholangitis[26]. The dose of the antibiotics should be adjusted according to renal and hepatic functions. Ideally, the antibiotics should be continued for 7 to 10 d[12].
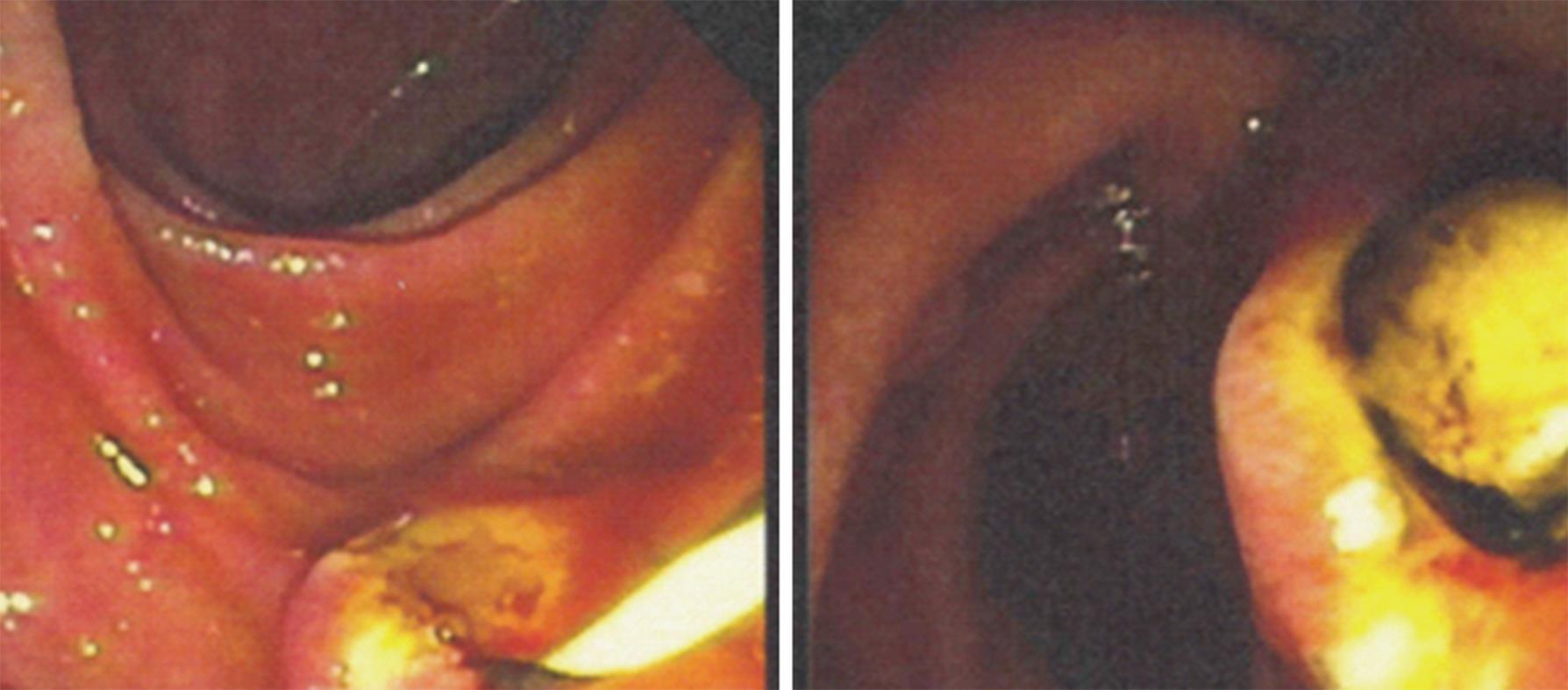
Because of high biliary intraductal pressure, biliary secretion of antibiotics is impaired. So, biliary drainage is the next step. It can be best done by therapeutic ERCP. Depending on the etiology of biliary obstruction, intervention should be done. For example, in case of choledocholithiasis, sphincterotomy and stone extraction (Figures 3-5) should be done with or without transpapillary biliary stent placement. Sometimes, there is an increased risk of bleeding from biliary sphincterotomy if the patient is coagulopathic or on anti-platelet agents. In those cases, biliary stent can be placed temporarily without sphincterotomy. In case of biliary stricture, transpapillary biliary stent placement should give adequate drainage. If there is blockage of the existing stent due to growth of bacterial biofilm and formation of bile sludge, the old stent should be removed and replaced with a new one[27].
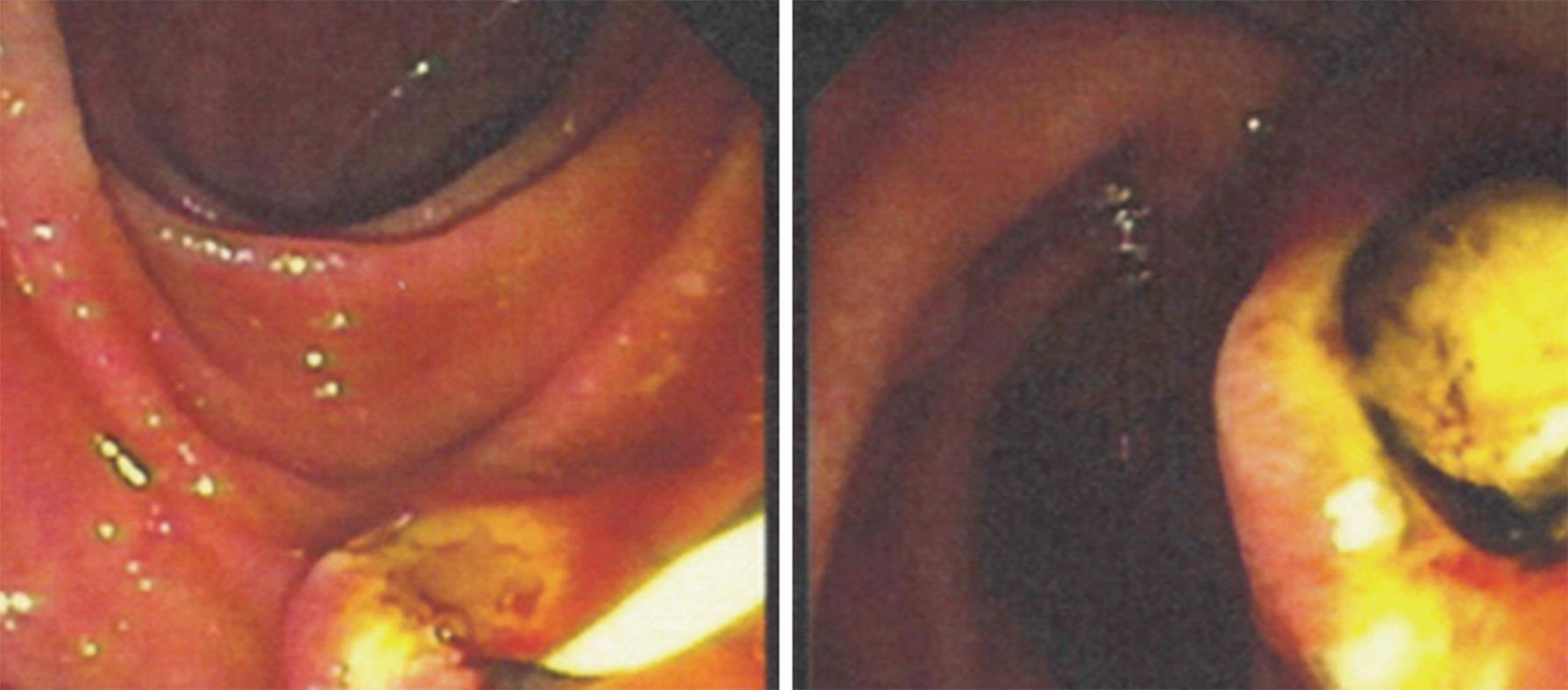
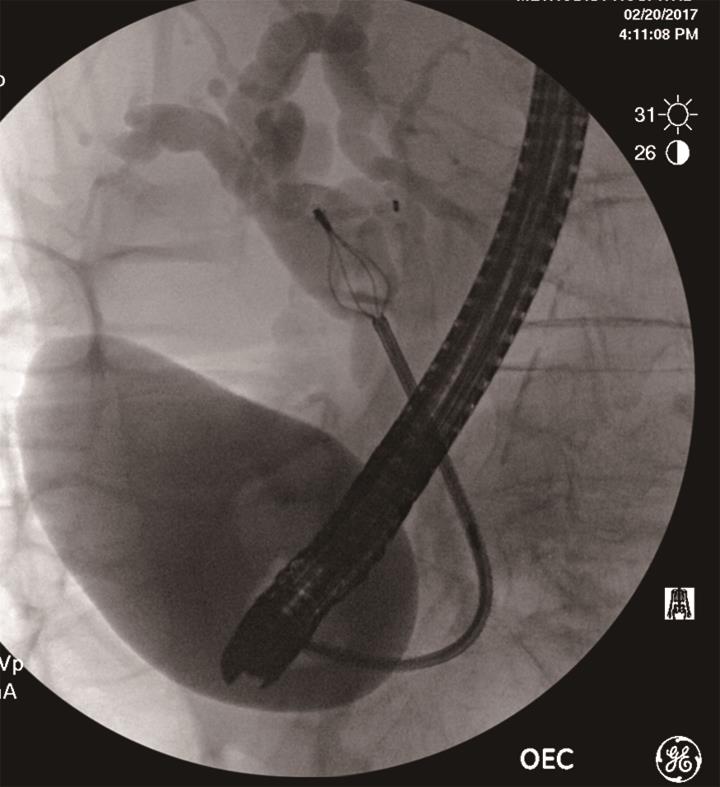
Other modalities of biliary drainage include endoscopic nasobiliary drainage (ENBD) by nasobiliary catheter (Figure 6), percutaneous transhepatic biliary drainage (PTBD), EUS-guided drainage and open surgical drainage (T-tube drainage after laparotomy).
In clinical practice, ENBD is done much less frequently, as compared to biliary stent placement. ENBD has the advantages that repeat cholangiogram could be done when the location of biliary stricture is not known, thick pus or purulent bile can be drained more effectively, washing can be done if the tube is clogged, biliary aspirate can be cultured and no additional sphincterotomy is required. The disadvantages are that it is uncomfortable to the patient and a confused patient may pull it out[28].
PTBD is generally done in case of failed ERCP or if the patient has multiple comorbidities and is not a good candidate for ERCP. There is no need for intravenous sedation or anesthesia for PTBD. The disadvantages include patient’s discomfort, increased length of hospital stay, risks of biliary peritonitis, intraperitoneal hemorrhage and sepsis[29]. It is contraindicated in patients with ascites, coagulopathies and intrahepatic biliary obstructions.
EUS-guided biliary drainage can be performed when ERCP is unsuccessful due to various reasons like ampullary obstruction, gastric outlet obstruction or surgically altered anatomy (Roux-en-Y surgery, gastric bypass, etc.), and intrahepatic bile ducts are not dilated[30]. Urgent EUS-guided choledochoduodenostomy with placement of a covered metallic stent is an option in the setting of acute cholangitis[31], mainly in tertiary care centers.
Surgical drainage is reserved when other modalities of biliary drainage are contra-indicated or fail. It is done rarely now-a-days because of high morbidity and mortality of 20% to 60%[32]. To avoid prolonged surgery, choledochotomy with T-tube drainage without choledocholithotomy is recommended[33]. Laparoscopic choledochotomy with stone extraction can be done in case of failed endoscopic extraction of common bile duct stone[34].
In patients with surgically altered anatomy like Roux-en-Y anastomosis or hepaticojejunostomy, balloon enteroscope-assisted ERCP with biliary drainage is done with variable success rate, of 40% to 95%[35].
Timing of biliary drainage: In grade I or mild acute cholangitis: Biliary drainage should be done in 24 h to 48 h. In grade II or moderate acute cholangitis (i.e., patient has not responded to antibiotics in first 24 h): Early biliary drainage, and in grade III or severe acute cholangitis: Urgent biliary drainage should be done. Following endoscopic management of acute cholangitis, laparoscopic cholecystectomy is recommended in patients with gallstone disease[36]. The various techniques of performing laparoscopic cholecystectomy safely have been described over the last few decades[37-39].
Management of recurrent pyogenic cholangitis (Oriental cholangiohepatitis) requires a multidisciplinary team (endoscopist, interventional radiologist and surgeon). Initial treatment includes administration of intravenous fluid and antibiotics, endoscopic treatment with stricture dilation, stone extraction and stent placement for biliary drainage or percutaneous biliary drainage in case of failed ERCP. Segmental hepatic resection should be considered in case of localized disease[40]. Orthotopic liver transplantation has also been reported in case of diffuse disease and end-stage liver disease due to recurrent acute cholangitis[41,42].
The prognosis depends on the timing of biliary drainage, administration of antibiotics and comorbidities of the patient. Early biliary drainage leads to rapid clinical improvement. But, if biliary drainage is delayed, patients can deteriorate quickly and die. The overall mortality acute cholangitis is less than 10% after biliary drainage[43]. In the pre-ERCP era, severe acute cholangitis was associated with a mortality of more than 50%[44]. Emergency surgery for severe acute cholangitis also carries a high mortality, of about 30%[45].
Poor prognostic factors in the setting of acute cholangitis include old age, high fever, leukocytosis, hyperbilirubinemia and hypoalbuminemia[11]. Patients with comorbidities like cirrhosis, malignancy, liver abscess and coagulopathy also carry poor prognosis.
Patients with high pre-biliary drainage serum creatinine is also associated with higher mortality[46]. A recent study also suggested that serum IL-7 level of less than 6.0 and serum procalcitonin level of more than 0.5 was associated with higher mortality[47].
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Hori H, Sergi CM, Tamori A S- Editor: Qi Y L- Editor: Filipodia E- Editor: Song XX
| 1. | Wada K, Takada T, Kawarada Y, Nimura Y, Miura F, Yoshida M, Mayumi T, Strasberg S, Pitt HA, Gadacz TR. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:52-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 208] [Cited by in RCA: 137] [Article Influence: 7.6] [Reference Citation Analysis (1)] |
| 2. | Lee SP, Roberts JR, Kuver R. The changing faces of cholangitis. F1000Res. 2016;5:pii: F1000. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Clough J, Shah R. Primary Amyloidosis Presenting as Common Bile Duct Obstruction With Cholangitis. ACG Case Rep J. 2015;2:107-109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Uygur-Bayramiçli O, Ak O, Dabak R, Demirhan G, Ozer S. Taenia saginata a rare cause of acute cholangitis: a case report. Acta Clin Belg. 2012;67:436-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 5. | Mosler P. Management of acute cholangitis. Gastroenterol Hepatol (N Y). 2011;7:121-123. [PubMed] |
| 6. | Epstein L, Hunter JC, Arwady MA, Tsai V, Stein L, Gribogiannis M, Frias M, Guh AY, Laufer AS, Black S. New Delhi metallo-β-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA. 2014;312:1447-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 318] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 7. | Kimura Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Windsor JA, Mayumi T, Yoshida M. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:8-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 124] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Shaffer EA. Gallstone disease: Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20:981-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 486] [Article Influence: 25.6] [Reference Citation Analysis (6)] |
| 9. | What if it’s acute cholangitis? Drug Ther Bull. 2005;43:62-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Sung JY, Costerton JW, Shaffer EA. Defense system in the biliary tract against bacterial infection. Dig Dis Sci. 1992;37:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 148] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Buyukasik K, Toros AB, Bektas H, Ari A, Deniz MM. Diagnostic and therapeutic value of ERCP in acute cholangitis. ISRN Gastroenterol. 2013;2013:191729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | van den Hazel SJ, Speelman P, Tytgat GN, Dankert J, van Leeuwen DJ. Role of antibiotics in the treatment and prevention of acute and recurrent cholangitis. Clin Infect Dis. 1994;19:279-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Jain MK, Jain R. Acute bacterial cholangitis. Curr Treat Options Gastroenterol. 2006;9:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Kinney TP. Management of ascending cholangitis. Gastrointest Endosc Clin N Am. 2007;17:289-306, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Lim JH. Liver flukes: the malady neglected. Korean J Radiol. 2011;12:269-279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Kiriyama S, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yokoe M. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20:24-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 197] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 17. | Kiriyama S, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Yokoe M. New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci. 2012;19:548-556. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 135] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 18. | Boey JH, Way LW. Acute cholangitis. Ann Surg. 1980;191:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 177] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Lipsett PA, Pitt HA. Acute cholangitis. Front Biosci. 2003;8:s1229-s1239. [PubMed] |
| 20. | Scott TM, Rosh AJ. Acute Cholangitis Differential Diagnoses. Medscape. Updated November 21, 2016. Available from: http://www.medscape.com. |
| 21. | Lim JH. Oriental cholangiohepatitis: pathologic, clinical, and radiologic features. AJR Am J Roentgenol. 1991;157:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 91] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Okuno WT, Whitman GJ, Chew FS. Recurrent pyogenic cholangiohepatitis. AJR Am J Roentgenol. 1996;167:484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Gallix BP, Aufort S, Pierredon MA, Garibaldi F, Bruel JM. [Acute cholangitis: imaging diagnosis and management]. J Radiol. 2006;87:430-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | de Lédinghen V, Lecesne R, Raymond JM, Gense V, Amouretti M, Drouillard J, Couzigou P, Silvain C. Diagnosis of choledocholithiasis: EUS or magnetic resonance cholangiography? A prospective controlled study. Gastrointest Endosc. 1999;49:26-31. [RCA] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 135] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 25. | Qureshi WA. Approach to the patient who has suspected acute bacterial cholangitis. Gastroenterol Clin North Am. 2006;35:409-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Tanaka A, Takada T, Kawarada Y, Nimura Y, Yoshida M, Miura F, Hirota M, Wada K, Mayumi T, Gomi H. Antimicrobial therapy for acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:59-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Donelli G, Guaglianone E, Di Rosa R, Fiocca F, Basoli A. Plastic biliary stent occlusion: factors involved and possible preventive approaches. Clin Med Res. 2007;5:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 28. | Nagino M, Takada T, Kawarada Y, Nimura Y, Yamashita Y, Tsuyuguchi T, Wada K, Mayumi T, Yoshida M, Miura F. Methods and timing of biliary drainage for acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:68-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Clouse ME, Evans D, Costello P, Alday M, Edwards SA, McDermott WV Jr. Percutaneous transhepatic biliary drainage. Complications due to multiple duct obstructions. Ann Surg. 1983;198:25-29. [PubMed] |
| 30. | Karaliotas C, Sgourakis G, Goumas C, Papaioannou N, Lilis C, Leandros E. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Surg Endosc. 2008;22:1826-1831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Artifon EL, Ferreira FC, Sakai P. Endoscopic ultrasound-guided biliary drainage. Korean J Radiol. 2012;13 Suppl 1:S74-S82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Minaga K, Kitano M, Imai H, Yamao K, Kamata K, Miyata T, Omoto S, Kadosaka K, Yoshikawa T, Kudo M. Urgent endoscopic ultrasound-guided choledochoduodenostomy for acute obstructive suppurative cholangitis-induced sepsis. World J Gastroenterol. 2016;22:4264-4269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Liu CL, Fan ST. Acute cholangitis. Holzheimer RG, Mannick JA, editors. Munich: Zuckschwerdt 2001; . |
| 34. | Tsuyuguchi T, Takada T, Kawarada Y, Nimura Y, Wada K, Nagino M, Mayumi T, Yoshida M, Miura F, Tanaka A. Techniques of biliary drainage for acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:35-45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Itoi T, Tsuyuguchi T, Takada T, Strasberg SM, Pitt HA, Kim MH, Belli G, Mayumi T, Yoshida M, Miura F. TG13 indications and techniques for biliary drainage in acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20:71-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 36. | Poon RT, Liu CL, Lo CM, Lam CM, Yuen WK, Yeung C, Fan ST, Wong J. Management of gallstone cholangitis in the era of laparoscopic cholecystectomy. Arch Surg. 2001;136:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 37. | Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101-125. [PubMed] |
| 38. | Callery MP. Avoiding biliary injury during laparoscopic cholecystectomy: technical considerations. Surg Endosc. 2006;20:1654-1658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 39. | Hori T, Oike F, Furuyama H, Machimoto T, Kadokawa Y, Hata T, Kato S, Yasukawa D, Aisu Y, Sasaki M. Protocol for laparoscopic cholecystectomy: Is it rocket science? World J Gastroenterol. 2016;22:10287-10303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 40. | Cosenza CA, Durazo F, Stain SC, Jabbour N, Selby RR. Current management of recurrent pyogenic cholangitis. Am Surg. 1999;65:939-943. [PubMed] |
| 41. | Jeyarajah DR. Recurrent Pyogenic Cholangitis. Curr Treat Options Gastroenterol. 2004;7:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 42. | Strong RW, Chew SP, Wall DR, Fawcett J, Lynch SV. Liver transplantation for hepatolithiasis. Asian J Surg. 2002;25:180-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Zhang WZ, Chen YS, Wang JW, Chen XR. Early diagnosis and treatment of severe acute cholangitis. World J Gastroenterol. 2002;8:150-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Andrew DJ, Johnson SE. Acute suppurative cholangitis, a medical and surgical emergency. A review of ten years experience emphasizing early recognition. Am J Gastroenterol. 1970;54:141-154. [PubMed] |
| 45. | Lai EC, Tam PC, Paterson IA, Ng MM, Fan ST, Choi TK, Wong J. Emergency surgery for severe acute cholangitis. The high-risk patients. Ann Surg. 1990;211:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 82] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 46. | Tai DI, Shen FH, Liaw YF. Abnormal pre-drainage serum creatinine as a prognostic indicator in acute cholangitis. Hepatogastroenterology. 1992;39:47-50. [PubMed] |
| 47. | Suwa Y, Matsuyama R, Goto K, Kadokura T, Sato M, Mori R, Kumamoto T, Taguri M, Miyasho T, Endo I. IL-7 and procalcitonin are useful biomarkers in the comprehensive evaluation of the severity of acute cholangitis. J Hepatobiliary Pancreat Sci. 2017;24:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (1)] |