Published online Feb 15, 2011. doi: 10.4291/wjgp.v2.i1.15
Revised: October 28, 2011
Accepted: November 4, 2011
Published online: February 15, 2011
A 67-year-old man visited our hospital with a history of continuous hematochezia leading to hemorrhagic shock. An abdominal computed tomography scan revealed a large mass in the ascending colon invading the duodenum and pancreatic head as well as extravasation of blood from the gastroduodenal artery (GDA) into the colon. Colonoscopy revealed an irregular ulcerative lesion and stenosis in the ascending colon. Therefore, right hemicolectomy combined with pylorus-preserving pancreaticoduodenectomy was performed. Histologically, the tumor was classified as a moderately differentiated adenocarcinoma. Moreover, cancer cells were mainly located in the colon but had also invaded the duodenum and pancreas and involved the GDA. Immunohistochemically, the tumor cells were positive for cytokeratin (CK)20 and carcinoembryonic antigen (CEA) but not for CK7 and carbohydrate antigen (CA)19-9. The patient died 23 d after the surgery because he had another episode of arterial bleeding from the anastomosis site. Although En bloc resection of the tumor with pancreaticoduodenectomy and colectomy performed for locally advanced colon cancer can ensure long-term survival, patients undergoing these procedures should be carefully monitored, particularly when the tumor involves the main artery.
- Citation: Iwata T, Konishi K, Yamazaki T, Kitamura K, Katagiri A, Muramoto T, Kubota Y, Yano Y, Kobayashi Y, Yamochi T, Ohike N, Murakami M, Gokan T, Yoshikawa N, Imawari M. Right colon cancer presenting as hemorrhagic shock. World J Gastrointest Pathophysiol 2011; 2(1): 15-18
- URL: https://www.wjgnet.com/2150-5330/full/v2/i1/15.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v2.i1.15
Colorectal cancers (CRCs) invading the adjacent organs are not uncommon in clinical practice, with an incidence of 5.5%-16.7%[1]. However, CRCs invading the pancreas or duodenum are rare; Saiura et al[2] reported that the incidence of such CRCs was 0.39% of the 3 074 patients who had undergone surgical resection. Moreover, hematochezia caused by arterial bleeding is extremely rare as a presentation of CRCs. In this report, we describe a case of CRC invading the pancreatic head and duodenum presenting hematochezia and also discuss the relevant literature.
A 67-year-old man visited the local physician for abdominal pain and hematochezia in June 2007. He received blood transfusion because he had severe anemia. He was later transferred to the Showa University Hospital because he developed shock as a result of continuous lower gastrointestinal tract bleeding. Laboratory tests on admission revealed that the hemoglobin level was 5.1 g/dL and that the serum levels of carcinoembryonic antigen (CEA) were slightly elevated (10.1 ng/mL), while those of carbohydrate antigen 19-9 (CA19-9) were normal.
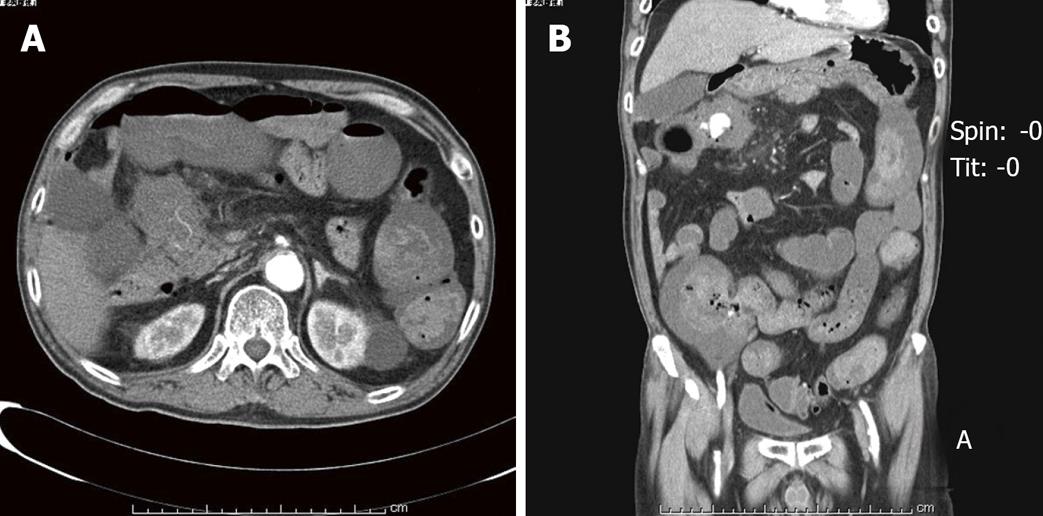
An abdominal computed tomography (CT) scan (Figure 1) revealed a large mass in the ascending colon and extravasation of blood from the gastroduodenal artery (GDA) into the colon. Therefore, we performed transcatheter arterial embolization (TAE) to control arterial bleeding from the GDA. Colonoscopy was performed after the patient’s general condition had improved. It revealed an irregular ulcerative lesion and stenotic changes in the ascending colon. The colonoscopic appearance of the tumor was similar to that of Borrmann type 3 tumors; however, histological examination of the endoscopic biopsy showed only necrotic tissue. Gastrografin enema study showed a stenotic lesion with irregular margins in the ascending colon adjacent to the hepatic flexure. CT showed a primary tumor that invaded the duodenum and pancreatic head. (Figure 1A)
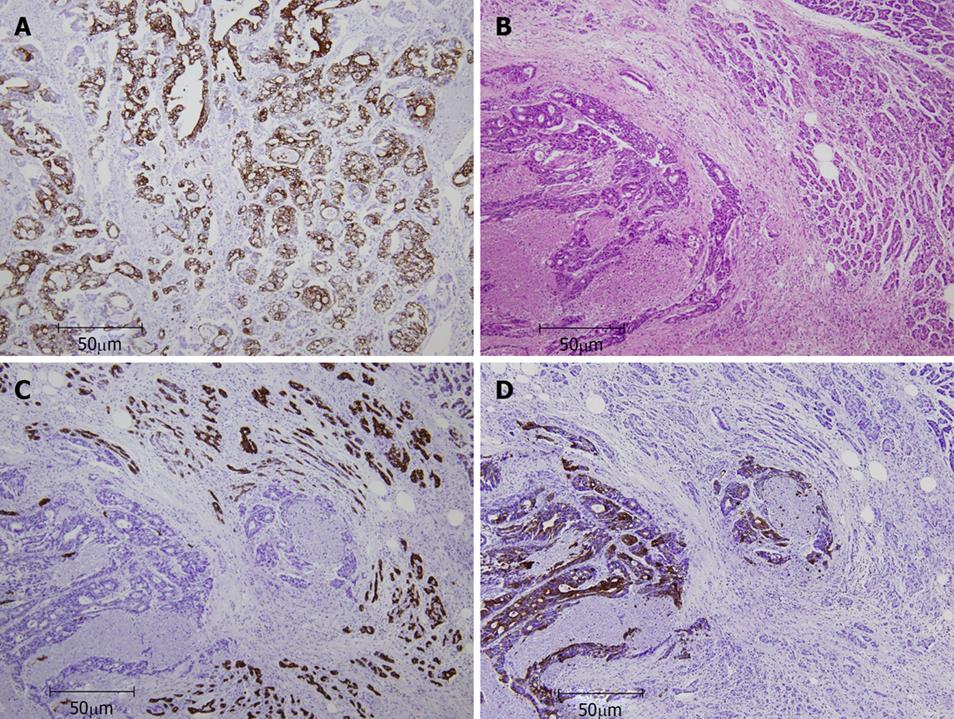
On account of the obstructive nature of the tumor, right hemicolectomy combined with pylorus-preserving pancreaticoduodenectomy (PD) was performed. During the surgery, we observed a bulky mass directly invading the duodenum, pancreas, and portal vein. Macroscopically, the resected specimen appeared as an irregular, huge mass involving the ascending colon, pancreatic head, duodenum, and portal vein. Microscopically, the tumor was a moderately differentiated adenocarcinoma with foci of poor differentiation. The tumor cells had infiltrated the serosal layer and showed marked lymphatic and venous invasion. Moreover, cancer cells were mainly located in the colon but had also invaded the duodenum and pancreas and involved the GDA. Two of the 23 resected lymph nodes revealed tumor cell infiltration. The immunohistochemical examination showed that the tumor cells were positive for cytokeratin (CK) 20, CEA, and MUC1, and focally positive for MUC2, but not for CK7 and CA19-9. Immunohistochemical staining of pancreatic tissue clearly showed that the tumor cells were positive for CK20 but not for CK7 (Figure 2C). In contrast, the normal pancreatic tissues stained positively for CK7 but not for CK20 (Figure 2D). As was the case with the pancreatic tumor cells, the colonic tumor cells showed positive immunostaining for CK20 but not for CK7 (Figure 2A). These immunohistochemical findings suggest that the tumor cells originated from the colon but not from the pancreas. On the basis of all these findings, the tumor was T3N1M0 consistent and stage IIIb colon cancer.
The postoperative course was uneventful, and the patient was discharged from our hospital 18th d after the surgery. However, the patient suddenly developed hematochezia and hemorrhagic shock 3 d later after the discharge. CT revealed extravasation of blood into the abdominal cavity near the site of anastomosis. TAE was performed to stop the arterial bleeding. However, he died 23 d after the surgery. Autopsy was not performed.
Although approximately 10% of CRCs have been reported to show adherence to adjacent organs, the incidence of direct invasion to the pancreatic head or duodenum is less than 1%[1-4]. Right-sided colon cancers may involve the liver, pancreas, or duodenum. Patients who undergo resection with an adequate surgical margin have a prognosis similar to that of patients without involvement of adjacent organs on a stage-matched basis[5,6]. Local recurrence is frequently observed in patients who undergo dissection of adhesions[7,8]. Thus, right hemicolectomy combined with PD (en bloc resection) can achieve radical resection of the tumor, which can improve the survival in right-sided cancer with pancreatic and/or duodenal invasion.
Saiura et al[2] suggest that PD for advanced colon cancer invading the pancreas improves the long-term survival of the patient, unless the tumor is a node-positive or mucinous/poorly differentiated adenocarcinoma. In our case, en bloc resection together with the dissection of adhesions was performed because CT revealed pancreatic and duodenal invasion of the colon cancer, and lymph node metastases were detected in CT performed before surgery. However, the patient died within 30 d of the surgery because of another episode of arterial bleeding at the anastomosis site. Although we attempted TAE for the feeder artery, the patient developed multiple organ failure. Mortality rates have been reported to be higher in patients with multiple resections compared to those treated by conventional colorectal resection (12% vs 6%, respectively)[9]. With recent advances in surgical management, the operation risk associated with PD has been decreasing. However, high-volume centers have reported that mortality rates after PD are 1%-6%[10-12]. We should take into account the operative risk for extended colorectal resection combined with PD.
CK7 and CK20 phenotyping using immunohistochemical staining is useful for the differential diagnosis of the origin of metastasis. Chu et al[13]suggest that 95% of CRC were CK7-negative/CK20-positive, whereas none of the pancreatic cancer cells showed this staining pattern. Immunohistochemical analysis of colonic and pancreatic tumors showed CK7-negativity and CK20-positivity (Figure 2). Immunohistochemically, CEA-positivity and CA19-9-negativity were consistent with the results of the CK7/CK20 expression pattern, which is often observed in CRC. Immunohistochemical analysis using a combination of different antigens enables clinicians to obtain information for identifying the primary tumor.
Severe hematochezia from arterial bleeding, followed by the development of hemorrhagic shock, is a rare presentation of CRC[8]. The common causes of lower gastrointestinal bleeding are diverticular diseases, angiodysplasia, colitis, or ulcers. In this case, however, the bleeding was caused by the tumor involvement of GDA with pancreatic and duodenal invasion.
In summary, severe hematochezia from arterial bleeding is a rare complication in patients with CRC. Although en block resection with PD and colectomy for locally advanced colon cancer can promote long-term survival, patients undergoing these procedures should be carefully monitored whenever the tumor involves the main artery.
Peer reviewer: Yong-Liang Zhu, PhD, Associate Science Professor, Department of Gastroenterology, Second Affiliated Hospital, Zhejiang University School of Medicine, Jiefang road 88#, Hangzhou 310009, Zhejiang Province, China
S- Editor Zhang HN L- Editor Hughes D E- Editor Liu N
| 1. | Berrospi F, Celis J, Ruiz E, Payet E. En bloc pancreaticoduodenectomy for right colon cancer invading adjacent organs. J Surg Oncol. 2002;79:194-197; discussion 198. |
| 2. | Saiura A, Yamamoto J, Ueno M, Koga R, Seki M, Kokudo N. Long-term survival in patients with locally advanced colon cancer after en bloc pancreaticoduodenectomy and colectomy. Dis Colon Rectum. 2008;51:1548-1551. |
| 3. | Eldar S, Kemeny MM, Terz JJ. Extended resections for carcinoma of the colon and rectum. Surg Gynecol Obstet. 1985;161:319-322. |
| 4. | Perez RO, Coser RB, Kiss DR, Iwashita RA, Jukemura J, Cunha JE, Habr-Gama A. Combined resection of the duodenum and pancreas for locally advanced colon cancer. Curr Surg. 2005;62:613-617. |
| 5. | Orkin BA, Dozois RR, Beart RW Jr, Patterson DE, Gunderson LL, Ilstrup DM. Extended resection for locally advanced primary adenocarcinoma of the rectum. Dis Colon Rectum. 1989;32:286-292. |
| 6. | Curley SA, Evans DB, Ames FC. Resection for cure of carcinoma of the colon directly invading the duodenum or pancreatic head. J Am Coll Surg. 1994;179:587-592. |
| 7. | McGlone TP, Bernie WA, Elliott DW. Survival following extended operations for extracolonic invasion by colon cancer. Arch Surg. 1982;117:595-599. |
| 8. | Anand AC, Patnaik PK, Bhalla VP, Chaudhary R, Saha A, Rana VS. Massive lower intestinal bleeding--a decade of experience. Trop Gastroenterol. 2001;22:131-134. |
| 9. | Gall FP, Tonak J, Altendorf A. Multivisceral resections in colorectal cancer. Dis Colon Rectum. 1987;30:337-341. |
| 10. | Edge SB, Schmieg RE Jr, Rosenlof LK, Wilhelm MC. Pancreas cancer resection outcome in American University centers in 1989-1990. Cancer. 1993;71:3502-3508. |
| 11. | Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg. 2006;244:10-15. |
| 12. | Gordon TA, Burleyson GP, Tielsch JM, Cameron JL. The effects of regionalization on cost and outcome for one general high-risk surgical procedure. Ann Surg. 1995;221:43-49. |
| 13. | Chu P, Wu E, Weiss LM. Cytokeratin 7 and cytokeratin 20 expression in epithelial neoplasms: a survey of 435 cases. Mod Pathol. 2000;13:962-972. |