Published online Aug 12, 2020. doi: 10.4291/wjgp.v11.i5.104
Peer-review started: January 17, 2020
First decision: April 9, 2020
Revised: April 24, 2020
Accepted: June 27, 2020
Article in press: June 27, 2020
Published online: August 12, 2020
Processing time: 199 Days and 9.7 Hours
Inflammatory bowel disease (IBD) causes systemic vascular inflammation. The increased risk of venous as well as arterial thromboembolic phenomena in IBD is well established. More recently, a relationship between IBD and atherosclerotic cardiovascular disease (ASCVD) has been postulated. Systemic inflammatory diseases, such as rheumatoid arthritis and systemic lupus erythematosus, have well characterized cardiac pathologies and treatments that focus on prevention of disease associated ASCVD. The impact of chronic inflammation on ASCVD in IBD remains poorly characterized. This manuscript aims to review and summarize the current literature pertaining to IBD and ASCVD with respect to its pathophysiology and impact of medications in order to encourage further research that can improve understanding and help develop clinical recommendations for prevention and management of ASCVD in patients with IBD.
Core tip: Chronic inflammation in patients with inflammatory bowel disease (IBD) leads to increased risk of atherosclerotic cardiovascular disease (ASCVD). However, the role and potential impact of IBD therapy in modifying ASCVD risk, and vice-versa, remains poorly understood. Herein, we highlight the importance of ASCVD as an extraintestinal manifestation of IBD, discuss the pathophysiology common to both diseases, and explore the role of non-traditional risk factors of ASCVD in IBD. We intend to identify avenues for further clinical and translational research that may help develop clinical recommendations for the management of ASCVD risk in patients with IBD.
- Citation: Weissman S, Sinh P, Mehta TI, Thaker RK, Derman A, Heiberger C, Qureshi N, Amrutiya V, Atoot A, Dave M, Tabibian JH. Atherosclerotic cardiovascular disease in inflammatory bowel disease: The role of chronic inflammation. World J Gastrointest Pathophysiol 2020; 11(5): 104-113
- URL: https://www.wjgnet.com/2150-5330/full/v11/i5/104.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v11.i5.104
Inflammatory bowel disease (IBD) is a chronic, systemic, relapsing and remitting inflammatory disorder of the gut due to immune and endothelial dysfunction in genetically susceptible hosts[1]. The two main phenotypic patterns of IBD are Crohn’s disease (CD) and ulcerative colitis (UC)[2]. In addition to the primary gastrointestinal manifestations of IBD, a wide-range of extra-intestinal manifestations (EIMs) have also been reported[3,4]. One of the well-recognized EIMs of IBD is the increased risk of thromboembolic phenomena[5-7]. Several recent studies have demonstrated a two to four-fold increased risk of atherosclerotic cardiovascular disease (ASCVD) in patients with IBD as compared to the general population[8]. There is growing evidence that atherosclerosis involves dysregulation of innate and adaptive immune systems along with platelet and endothelial dysfunction. Hence, it is believed that the underlying chronic inflammatory process in patients with IBD, similar to other chronic inflammatory disorders, may drive ASCVD risk[9,10]. The goal of this manuscript is to review the association between ASCVD and IBD as well as identify avenues for further research that may help develop clinical recommendations for the management of ASCVD risk in patients with IBD.
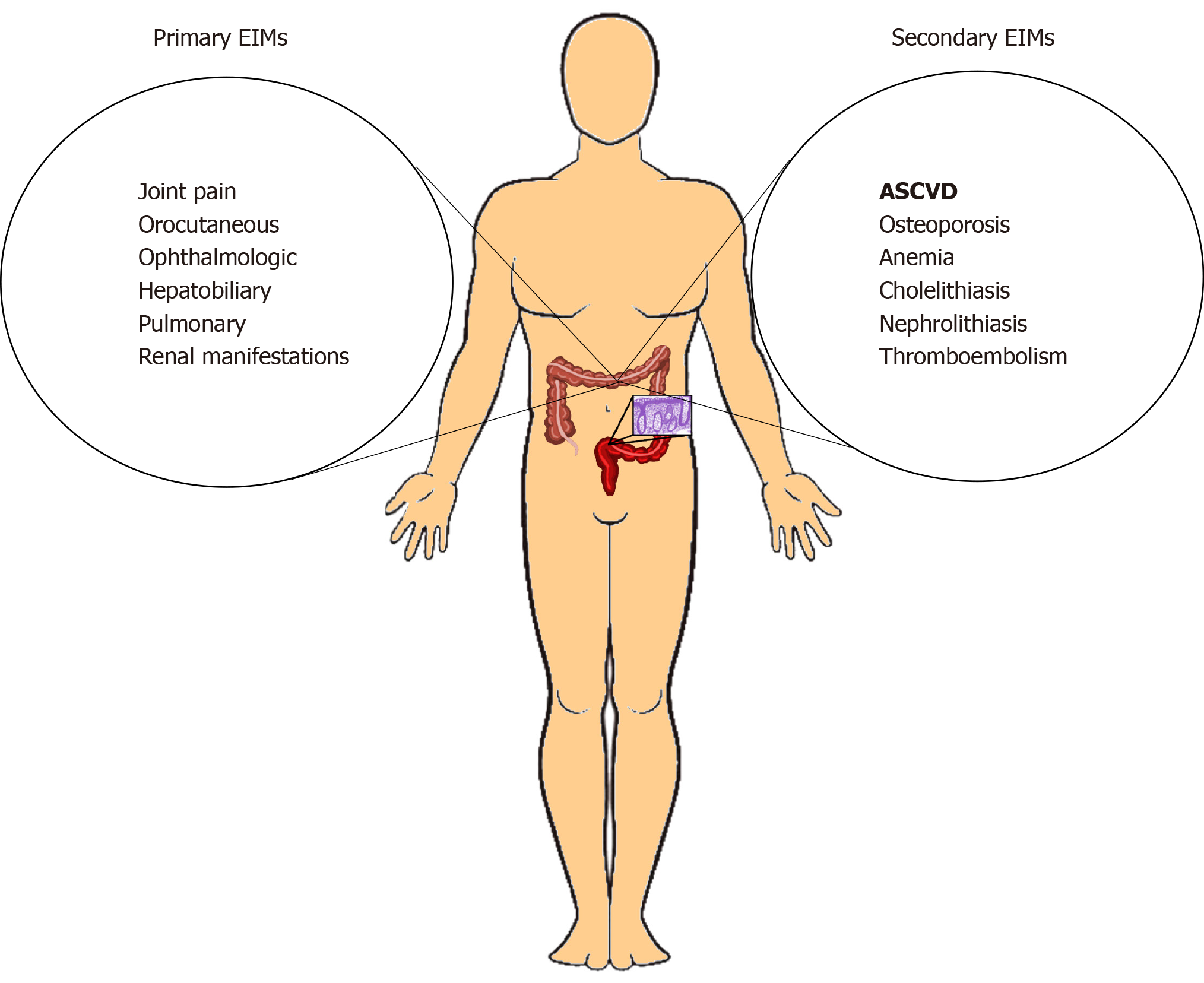
Patients with IBD are exposed to chronic, persistent, systemic inflammation over the course of their lifespan. This predisposes them to a wide range of sequelae across multiple organ systems. The EIMs associated with IBD are traditionally classified as primary and secondary[11]. Primary EIMs include joint, orocutaneous, ophthalmological, hepatobiliary, pulmonary, and renal manifestations (Figure 1). Among these, some parallel IBD disease activity (episcleritis, pyoderma gangrenosum, erythema nodosum, aphthous stomatitis, peripheral arthropathy) and others do not (uveitis, ankylosing spondylitis, primary biliary cirrhosis, alopecia areata, thyroid autoimmune disease). Secondary EIMs are complications related to IBD and include osteoporosis, anemia, cholelithiasis, nephrolithiasis, and thromboembolism (Figure 1)[10].
The relationship between IBD and venous thromboembolic phenomena has been well characterized[12-14]. Patients with IBD have a 1.7 to 5.9 times increased risk of venous thromboembolism as compared to the general population[14,15,16]. The underlying pathophysiologic mechanism of thromboembolic phenomena in IBD merits further investigation.
Labeling ASCVD as an EIM of IBD adds valuable understanding to the role of chronic inflammation in the two disease processes. Currently, we do not have enough knowledge regarding the effect of decreasing IBD disease burden on ASCVD and vice versa to categorize it as primary versus secondary EIM. There are no clinical human trials and long-term prospective data to assess whether ASCVD will follow the trajectory of gut inflammation in patients with IBD. Whether there is a specific time point in vascular disease after which reversibility is unachievable needs to be evaluated. The answer to these questions will help us more appropriately place ASCVD in the subcategories of EIM related to IBD. With current knowledge it can be categorized as a secondary EIM (Figure 1).
The incidence of ASCVD is increased in patients with IBD as reported by multiple population-based and few retrospective case control studies[17-22]. Indeed, there is a two to four-fold increased risk of myocardial infarction (MI), stroke and heart failure (HF) in patients with IBD. Data from Danish and other European cohort studies, for example have shown an association between ischemic heart disease (IHD) and IBD[17,20-22]. A Canadian study reported an increased risk of IHD (IRR 1.26; 95%CI: 1.11-1.44) and cerebrovascular accidents in patients with IBD (IRR 1.32; 95%CI: 1.05–1.66)[22]. Panhwar et al[8] analyzed inpatient and outpatient data from the Unites States and reported a two-fold increased risk of MI in patients with IBD[8].
Some studies and meta-analyses, however, have shown conflicting data[23,24]. Several reasons may account for this; for example, large retrospective cohort studies rely on billing data that are prone to miscoding. In addition, many studies lack data on disease activity and medication use that can influence the inflammatory process and hence the ASCVD events and risk. Studies that have assessed disease activity through indirect measures like steroid use or inpatient admissions have shown a more consistent positive association between the two inflammatory processes[19,20]. A pattern that has emerged over the years shows an increased risk of ASCVD with active disease and in younger and female patients as compared to the general population[9,20]. Notably, there are data showing increased subclinical atherosclerosis in patients with IBD as assessed by modalities such as carotid femoral pulse wave velocity, carotid intimal thickening, and flow-mediated dilatation (FMD)[24,25].
The effect of ASCVD related mortality in patients with IBD is debatable[12,23,26-29]. This can be attributed to multiple factors. Some studies assess mortality over the short duration of inpatient admission that might undermine the effect of long standing chronic inflammation[23,29,30]. Given the increased overall mortality among patients with IBD, it is possible that survivorship and participation bias are obscuring the potential IBD-ASCVD relationship[16]. Some studies lack rigorous matching of the control population[30]. Prospective studies with age matched control groups evaluating the role of IBD medications may be able to better assess the relationship between IBD and ASCVD.
Traditional risk factors for ASCVD are age (men > 45 years, women > 55 years), male gender, family history of coronary artery disease (CAD), obesity [body mass index (BMI) > 30], hypertension, diabetes, dyslipidemia, tobacco use, alcohol use, and chronic kidney disease. However, patients with IBD tend to have lower BMI and no significant lipid abnormality[18]. Aspects like age and gender have shown deviation from the general population. Nontraditional risk factors of arterial thromboembolism in patients with IBD merit further investigation.
IBD is characterized by high levels of C-reactive protein and various biomarkers that are associated with ASCVD, such as oxidized-low density lipoprotein, fibrinogen, matrix metallopeptidase, nuclear factor kappa-B, and interferon-γ. These are known to cause endothelial dysfunction, platelet aggregation, and hasten the development of ASCVD[31].
In a retrospective case control study, 356 IBD and 712 matched control patients, were assessed with an average follow up time of four and a half years. An increased incidence of ASCVD in patients with IBD despite having a lower burden of traditional risk factors was reported[18]. Furthermore, some non-traditional risk factors, such as white blood cells or perhaps even chronic inflammation, may have had a more robust impact on ASCVD in patients with IBD as compared to the traditional risk factors of hypertension, obesity, and hyperlipidemia[18]. We discuss in this manuscript (pathophysiology section) the biomarkers that link the two disease processes and have the potential for further translational research.
A higher risk of venous thromboembolism during active disease is well studied[9] Even though some studies have shown contrary results regarding the relationship between ASCVD and IBD, a consistent pattern of increased incidence of MI during periods of active disease has been evident[12,23,32,33]. A Danish cohort study evaluated 20795 patients with IBD and 199978 matched controls and showed increased risk of MI, stroke, and cardiovascular death during periods of active IBD. During periods of remission, these risks were similar to controls[17]. A French cohort study assessed MI, stroke and peripheral vascular disease in patients 30 days before and after hospital admission, which was taken as a surrogate marker for IBD flare, and found an increased risk of arterial thromboembolic events suggesting the importance of ongoing inflammation and its affect beyond the length of hospital admission[20]. A recent study from Olmsted County, Minnesota, showed an increased risk of MI and HF in patients with IBD with more active and extensive disease[19].
There have been no prospective studies to assess disease activity by stool, blood or clinical markers and correlate it with ASCVD events over short-term or long-term. Most studies have used surrogate markers of inflammation like steroid use, hospitalization or escalation of therapy for disease activity[34]. Studies that measure disease activity and its duration in a prospective manner are needed to better assess the outcomes of ASCVD in patients with IBD.
Multiple studies have shown that ASCVD tends to occur in women and younger patients with IBD as compared to the general population[8,35-39]. In a meta-analysis by Sun et al, data from 27 studies showed pooled relative risk for ASCVD, CAD, and MI was 1.25 (95%CI: 1.08-1.44), 1.17 (95%CI: 1.07-1.27) and 1.12 (95%CI: 1.05-1.21), respectively. An association was particularly noted in women with IBD[40]. The meta-analysis by Singh et al[40] identified an overall 19% increased risk of IHD among patients with IBD, however subgroup analysis found the risk among women with IBD to be 26% and the risk among men fell below the level of statistical significance. A Danish population based study that showed an increased risk of IHD in patients with IBD (IRR 1.22, 95%CI: 1.14-1.30) noted that the risk was higher in women (IRR 1.33, 95%CI: 1.21- 1.46) and younger patients of age 15-34 years (IRR 1.37, 95%CI: 0.98-1.93)[37]. An Asian cohort study showed that the adjusted hazard ratio for acute coronary syndrome in patients with IBD, compared with controls, was highest in 20 to 39 year age group at 3.28 (95%CI: 1.73-6.22), as compared to the overall risk of 1.70 (95%CI: 1.45-1.99)[36]. Recently published study from a large United States database reported higher prevalence of IHD in patients with UC and CD as compared to non-IBD patients [UC 6.9% vs CD 9.0% vs non-IBD 4.0%, OR for UC 2.09 (2.04-2.13), and CD 2.79 (2.74–2.85)]. In this patient cohort, the prevalence of MI was highest among younger patients with IBD[8].
It has been shown that patients with other chronic inflammatory conditions, e.g., psoriasis, also have evidence of ASCVD at a younger age than general population[38]. Younger CD patients have more aggressive disease with more disease burden early during their life and hence it is important to assess their risk of other pro-inflammatory conditions like atherosclerosis[35]. Investigating and identifying the factors that influence this increased risk (e.g., disease duration and severity) in patients with IBD will help start early intervention with appropriate therapy and thereby decrease inflammatory burden, aimed at long-term risk modification.
Atherosclerosis is the most common cause of ischemic cardiomyopathy and vascular disease. Chronic inflammation involving the innate and adaptive immune system along with endothelial and platelet dysfunction is present in both atherosclerosis and IBD.
Endothelial cells, lymphocytes, monocytes, macrophages are all involved in the pathogenesis of atherosclerosis from formation of foam cells to development of plaque[39,41-44]. Disruption of the endothelium early in the process of atherosclerosis leads to upregulation of adhesion molecules, deposition of lipoproteins in the subendothelial and recruitment of circulating monocytes from the spleen and bone marrow. Some of the adhesions molecules like VCAM1, P-selectin, and ICAM1 are notable in this pathway that lead to expression of chemokines like CCR1, CCR5 and CX3C receptor 1[45-48]. Many of these adhesions’ molecules have been implicated in the pathogenesis of IBD and as potential therapeutic drug targets. Vedolizumab is an anti-integrin molecule that prevents recruitment of white blood cells to the gut by inhibiting binding of α4β7 adhesion molecules on the monocytes to the endothelial cells and is widely used to treat CD and UC[49]. Exploring the effect of such medications on ASCVD risk in IBD patients is a potential avenue of research. Further in the process of atherosclerosis, the recruited monocytes differentiate into activated macrophages and take up the apoB containing lipoproteins leading to lipid accumulation and formation of macrophage driven foam cells that overtime lay the foundation of a necrotic lipid core[50-52]. The role of endothelial dysfunction in patients with IBD has been evaluated in a small study through nitric oxide mediated dilatation of the vessels[41]. Endothelial dysfunction as assessed by FMD has been shown to be impaired in patients with active UC[42].
In addition to the innate immune system (macrophages) and endothelial dysfunction (adhesion molecules), the adaptive immune system (T and B lymphocytes, dendritic cells) is involved in the pathogenesis of atherosclerosis. Activation of T helper 1(TH) leads to production of pro-inflammatory cytokines [interleukin (IL)-1, IL-6, tumor necrosis factor] that activate local inflammatory cascade[53]. These cytokines are also involved in the pathogenesis of IBD through activation of TH1 and TH17 cells in CD and TH2 cells in UC. The JAK and STAT pathways that act downstream of cytokine mediated lymphocyte activation are implicated in the activation of IL-6 in atherosclerosis and IBD[54]. The JAK inhibitors are being extensively explored as a therapeutic target in IBD and tofacitinib (JAK 1/3 inhibitor) is currently used for treatment of moderate to severe UC[55]. Infliximab and other anti TNF medications are known therapeutic targets in IBD[56,57].
Translational research assessing pathways and cytokines of innate and adaptive immune system and, vascular endothelial dysfunction that are common to both inflammatory processes will help identify biomarkers that can be used to assess, risk stratify and develop focused preventive and treatment modalities to reduce ASCVD risk in patients with IBD.
Numerous studies have examined an overlap in treatment between IBD and heart disease, with relative success (Table 1). In a retrospective matched case–control study Ungaro et al[43] assessed statin use in patients with IBD. Statin use was associated with a significantly decreased risk of IBD (OR: 0.68, 95%CI: 0.64-0.72), CD (OR: 0.64, 95%CI: 0.59-0.71), and UC (OR: 0.70, 95%CI: 0.65-0.76)[43]. Two studies developed animal models of IBD by chemically inducing CD and UC and showed that captopril was implicated in reducing transforming growth factor-beta1 expression and colitis-associated fibrosis[44,58]. Clopidogrel also reduced disease activity index and colonic mucosal damage index in mice – thus providing an additional link between treatment of IBD and ASCVD[58].
| Ref. | Study type | The number of patients | Efficacy in treatment overlap |
| Ungaro et al[43] | Retrospective matched case-control study | A total of 9617 cases and 46665 controls were included in the analysis | Statistically significant decreased risk of new onset IBD in patients taking statin therapy |
| Wengrower et al[44] | Chemically induced colitis, animal model | A total of 40 male rats were divided into normal control, captopril only, induced-colitis control, and induced-colitis with captopril arms | A significant reduction in fibrosis, levels of TGF-beta1 mRNA, and protein was found in patients with IBD taking captopril |
| Patel et al[58] | Chemically induced Crohn’s and UC, animal model | A total of 48 mice, divided into induced Crohn’s and UC arms, further divided into normal, disease, disease with standard therapy, and disease with clopidogrel | A statistically significant reduction in disease activity and colonic mucosal damage was seen in mice on clopidogrel |
| Rungoe et al[37] | Nationwide, population-based retrospective cohort study | A total of 28833 patients with IBD were compared to matched non-IBD patients from a dataset of 4.6 million | A statistically significant reduction in risk of ischemic heart disease was seen in patients given 5-ASA |
| Zanoli et al[61] | Multicenter prospective longitudinal study | 334 patients with IBD were followed for 4 yr | In patients with IBD anti-TNFα therapy reduced aortic pulse-wave velocity (a surrogate for cardiovascular risk) |
In addition to studies showing benefit for patients with IBD taking ASCVD medications, there have been studies assessing the role of anti-inflammatory medications for ASCVD in the general population. In a multicenter randomized control (CANTOS) trial by Ridker et al[59], canakinumab, a human monoclonal antibody targeted at IL-1, showed a 15% reduction in deaths from heart attacks and strokes combined. Further analysis of the CANTOS trial demonstrated that patients receiving canakinumab that achieved IL-6 levels below 1.65 ng/L had a 32% reduction in major ASCVD events, whereas those at or above 1.65 ng/L received no ASCVD-related benefits[54]. Although there was an increase in fatal infections in the treatment group resulting in no overall mortality benefit, it was clearly illustrated that treatment of inflammation independent of lipid levels resulted in fewer cardiovascular events, and IL-6 could be a potential common mechanism. In addition, a nationwide retrospective cohort study noted that for patients with IBD taking 5-aminosalicylic acid (5-ASA), the incidence of IHD was significantly less compared to those not taking 5-ASA[37]. A meta-analysis assessing anti-TNF use in IBD has given us some direction regarding medications that can influence disease activity and ASCVD in patients with IBD[60]. A multicenter prospective longitudinal study in patients with IBD evaluated arterial pulse wave velocity (a surrogate marker of subclinical atherosclerosis) found improvement with long-term anti–TNF therapy suggesting that reduction of inflammation can lead to improvement in endothelial dysfunction[61].
Clinicians should be aware of the harmful effects of chronic inflammation on the heart. ASCVD risk is increased among patients with IBD especially during periods of active disease. ASCVD in patients with IBD tends to favor non-traditional risk factors like younger age and female gender. The role of inflammatory markers of IBD as risk factors for ASCVD needs further investigation. Appropriate risk stratification is important in all age groups but especially in those that are diagnosed at an early age and carry the disease burden over a long time. Early escalation of care with more aggressive anti-inflammatory therapy may have a beneficial effect on chronic inflammatory processes like ASCVD, but this needs to be evaluated. Prospective studies assessing the role of IBD medications on ASCVD risk and events will help tailor therapy in patients with IBD based on the mechanism of the drug and subsequently help us move towards personalized medicine.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chiba T, Yang MS S-Editor: Dou Y L-Editor: A E-Editor: Wang LL
| 1. | Swanson GR, Burgess HJ, Keshavarzian A. Sleep disturbances and inflammatory bowel disease: a potential trigger for disease flare? Expert Rev Clin Immunol. 2011;7:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Sandborn WJ. Current directions in IBD therapy: what goals are feasible with biological modifiers? Gastroenterology. 2008;135:1442-1447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Mekhjian HS, Switz DM, Melnyk CS, Rankin GB, Brooks RK. Clinical features and natural history of Crohn's disease. Gastroenterology. 1979;77:898-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 234] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, Jewell DP, Karban A, Loftus EV, Peña AS, Riddell RH, Sachar DB, Schreiber S, Steinhart AH, Targan SR, Vermeire S, Warren BF. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19 Suppl A:5A-36A. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2148] [Cited by in RCA: 2368] [Article Influence: 215.3] [Reference Citation Analysis (0)] |
| 5. | Tabibian JH, Streiff MB. Inflammatory bowel disease-associated thromboembolism: a systematic review of outcomes with anticoagulation versus catheter-directed thrombolysis. Inflamm Bowel Dis. 2012;18:161-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Tabibian JH, Roth BE. Local thrombolysis: a newer approach to treating inflammatory bowel disease-related thromboembolism. J Clin Gastroenterol. 2009;43:391-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Tabibian JH, Lada SJ, Tabibian N. Combined inferior vena cava & renal vein thromboses: case and synopsis of thromboembolism in inflammatory bowel disease. Medscape J Med. 2008;10:6. [PubMed] |
| 8. | Panhwar MS, Mansoor E, Al-Kindi SG, Sinh P, Katz J, Oliveira GH, Cooper GS, Ginwalla M. Risk of Myocardial Infarction in Inflammatory Bowel Disease: A Population-based National Study. Inflamm Bowel Dis. 2019;25:1080-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 82] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 9. | Grainge MJ, West J, Card TR. Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet. 2010;375:657-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 556] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 10. | Conti P, Shaik-Dasthagirisaeb Y. Atherosclerosis: a chronic inflammatory disease mediated by mast cells. Cent Eur J Immunol. 2015;40:380-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 11. | Garber A, Regueiro M. Extraintestinal Manifestations of Inflammatory Bowel Disease: Epidemiology, Etiopathogenesis, and Management. Curr Gastroenterol Rep. 2019;21:31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 12. | Sridhar AR, Parasa S, Navaneethan U, Crowell MD, Olden K. Comprehensive study of cardiovascular morbidity in hospitalized inflammatory bowel disease patients. J Crohns Colitis. 2011;5:287-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Saleh T, Matta F, Yaekoub AY, Danescu S, Stein PD. Risk of venous thromboembolism with inflammatory bowel disease. Clin Appl Thromb Hemost. 2011;17:254-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Novacek G, Weltermann A, Sobala A, Tilg H, Petritsch W, Reinisch W, Mayer A, Haas T, Kaser A, Feichtenschlager T, Fuchssteiner H, Knoflach P, Vogelsang H, Miehsler W, Platzer R, Tillinger W, Jaritz B, Schmid A, Blaha B, Dejaco C, Eichinger S. Inflammatory bowel disease is a risk factor for recurrent venous thromboembolism. Gastroenterology. 2010;139:779-787, 787.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 184] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 15. | Tan VP, Chung A, Yan BP, Gibson PR. Venous and arterial disease in inflammatory bowel disease. J Gastroenterol Hepatol. 2013;28:1095-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Schicho R, Marsche G, Storr M. Cardiovascular complications in inflammatory bowel disease. Curr Drug Targets. 2015;16:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 17. | Kristensen SL, Ahlehoff O, Lindhardsen J, Erichsen R, Jensen GV, Torp-Pedersen C, Nielsen OH, Gislason GH, Hansen PR. Disease activity in inflammatory bowel disease is associated with increased risk of myocardial infarction, stroke and cardiovascular death--a Danish nationwide cohort study. PLoS One. 2013;8:e56944. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 178] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 18. | Yarur AJ, Deshpande AR, Pechman DM, Tamariz L, Abreu MT, Sussman DA. Inflammatory bowel disease is associated with an increased incidence of cardiovascular events. Am J Gastroenterol. 2011;106:741-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 206] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 19. | Aniwan S, Pardi DS, Tremaine WJ, Loftus EV. Increased Risk of Acute Myocardial Infarction and Heart Failure in Patients With Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2018;16:1607-1615.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 20. | Kirchgesner J, Beaugerie L, Carrat F, Andersen NN, Jess T, Schwarzinger M; BERENICE study group. Increased risk of acute arterial events in young patients and severely active IBD: a nationwide French cohort study. Gut. 2018;67:1261-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 108] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 21. | Kappelman MD, Horvath-Puho E, Sandler RS, Rubin DT, Ullman TA, Pedersen L, Baron JA, Sørensen HT. Thromboembolic risk among Danish children and adults with inflammatory bowel diseases: a population-based nationwide study. Gut. 2011;60:937-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 242] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 22. | Bernstein CN, Wajda A, Blanchard JF. The incidence of arterial thromboembolic diseases in inflammatory bowel disease: a population-based study. Clin Gastroenterol Hepatol. 2008;6:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 183] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 23. | Dorn SD, Sandler RS. Inflammatory bowel disease is not a risk factor for cardiovascular disease mortality: results from a systematic review and meta-analysis. Am J Gastroenterol. 2007;102:662-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Zanoli L, Signorelli SS, Inserra G, Castellino P. Subclinical Atherosclerosis in Patients With Inflammatory Bowel Diseases: A Systematic Review and Meta-Analysis. Angiology. 2017;68:463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Wu GC, Leng RX, Lu Q, Fan YG, Wang DG, Ye DQ. Subclinical Atherosclerosis in Patients With Inflammatory Bowel Diseases: A Systematic Review and Meta-Analysis. Angiology. 2017;68:447-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Mitchell NE, Harrison N, Junga Z, Singla M. Heart Under Attack: Cardiac Manifestations of Inflammatory Bowel Disease. Inflamm Bowel Dis. 2018;24:2322-2326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 27. | Osterman MT, Yang YX, Brensinger C, Forde KA, Lichtenstein GR, Lewis JD. No increased risk of myocardial infarction among patients with ulcerative colitis or Crohn's disease. Clin Gastroenterol Hepatol. 2011;9:875-880. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 28. | Bewtra M, Kaiser LM, TenHave T, Lewis JD. Crohn's disease and ulcerative colitis are associated with elevated standardized mortality ratios: a meta-analysis. Inflamm Bowel Dis. 2013;19:599-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 114] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 29. | Dave M, Mehta K, Badheka A, Loftus E. Inflammatory Bowel Disease Does Not Impact Mortality, but Increases Length of Hospitalization in Patients with Acute Myocardial Infarction. Am J Gastroenterol. 2013;108. [DOI] [Full Text] |
| 30. | Barnes EL, Beery RM, Schulman AR, McCarthy EP, Korzenik JR, Winter RW. Hospitalizations for Acute Myocardial Infarction Are Decreased Among Patients with Inflammatory Bowel Disease Using a Nationwide Inpatient Database. Inflamm Bowel Dis. 2016;22:2229-2237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 31. | Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6103] [Cited by in RCA: 6340] [Article Influence: 317.0] [Reference Citation Analysis (0)] |
| 32. | Ha C, Magowan S, Accortt NA, Chen J, Stone CD. Risk of arterial thrombotic events in inflammatory bowel disease. Am J Gastroenterol. 2009;104:1445-1451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 173] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 33. | Ruisi P, Makaryus JN, Ruisi M, Makaryus AN. Inflammatory bowel disease as a risk factor for premature coronary artery disease. J Clin Med Res. 2015;7:257-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 34. | Aarestrup J, Jess T, Kobylecki CJ, Nordestgaard BG, Allin KH. Cardiovascular Risk Profile Among Patients With Inflammatory Bowel Disease: A Population-based Study of More Than 100 000 Individuals. J Crohns Colitis. 2019;13:319-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 58] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 35. | Herzog D, Fournier N, Buehr P, Rueger V, Koller R, Heyland K, Nydegger A, Spalinger J, Schibli S, Petit LM, Braegger CP; Swiss IBD Cohort Study Group. Age at disease onset of inflammatory bowel disease is associated with later extraintestinal manifestations and complications. Eur J Gastroenterol Hepatol. 2018;30:598-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 36. | Tsai MS, Lin CL, Chen HP, Lee PH, Sung FC, Kao CH. Long-term risk of acute coronary syndrome in patients with inflammatory bowel disease: a 13-year nationwide cohort study in an Asian population. Inflamm Bowel Dis. 2014;20:502-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 37. | Rungoe C, Basit S, Ranthe MF, Wohlfahrt J, Langholz E, Jess T. Risk of ischaemic heart disease in patients with inflammatory bowel disease: a nationwide Danish cohort study. Gut. 2013;62:689-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 169] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 38. | Santilli S, Kast DR, Grozdev I, Cao L, Feig RL, Golden JB, Debanne SM, Gilkeson RC, Orringer CE, McCormick TS, Ward NL, Cooper KD, Korman NJ. Visualization of atherosclerosis as detected by coronary artery calcium and carotid intima-media thickness reveals significant atherosclerosis in a cross-sectional study of psoriasis patients in a tertiary care center. J Transl Med. 2016;14:217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 39. | Ruparelia N, Chai JT, Fisher EA, Choudhury RP. Inflammatory processes in cardiovascular disease: a route to targeted therapies. Nat Rev Cardiol. 2017;14:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 356] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 40. | Singh S, Singh H, Loftus EV, Pardi DS. Risk of cerebrovascular accidents and ischemic heart disease in patients with inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:382-93.e1: quiz e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 215] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 41. | Hatoum OA, Binion DG, Otterson MF, Gutterman DD. Acquired microvascular dysfunction in inflammatory bowel disease: Loss of nitric oxide-mediated vasodilation. Gastroenterology. 2003;125:58-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 200] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 42. | Principi M, Mastrolonardo M, Scicchitano P, Gesualdo M, Sassara M, Guida P, Bucci A, Zito A, Caputo P, Albano F, Ierardi E, Di Leo A, Ciccone MM. Endothelial function and cardiovascular risk in active inflammatory bowel diseases. J Crohns Colitis. 2013;7:e427-e433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 43. | Ungaro R, Chang HL, Côté-Daigneault J, Mehandru S, Atreja A, Colombel JF. Statins Associated With Decreased Risk of New Onset Inflammatory Bowel Disease. Am J Gastroenterol. 2016;111:1416-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 44. | Wengrower D, Zanninelli G, Pappo O, Latella G, Sestieri M, Villanova A, Faitelson Y, Pines M, Goldin E. Prevention of fibrosis in experimental colitis by captopril: the role of tgf-beta1. Inflamm Bowel Dis. 2004;10:536-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 45. | Cybulsky MI, Gimbrone MA. Endothelial expression of a mononuclear leukocyte adhesion molecule during atherogenesis. Science. 1991;251:788-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1152] [Cited by in RCA: 1136] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 46. | Heidt T, Sager HB, Courties G, Dutta P, Iwamoto Y, Zaltsman A, von Zur Muhlen C, Bode C, Fricchione GL, Denninger J, Lin CP, Vinegoni C, Libby P, Swirski FK, Weissleder R, Nahrendorf M. Chronic variable stress activates hematopoietic stem cells. Nat Med. 2014;20:754-758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 437] [Cited by in RCA: 590] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 47. | Combadière C, Potteaux S, Rodero M, Simon T, Pezard A, Esposito B, Merval R, Proudfoot A, Tedgui A, Mallat Z. Combined inhibition of CCL2, CX3CR1, and CCR5 abrogates Ly6C(hi) and Ly6C(lo) monocytosis and almost abolishes atherosclerosis in hypercholesterolemic mice. Circulation. 2008;117:1649-1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 496] [Cited by in RCA: 547] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 48. | Tacke F, Alvarez D, Kaplan TJ, Jakubzick C, Spanbroek R, Llodra J, Garin A, Liu J, Mack M, van Rooijen N, Lira SA, Habenicht AJ, Randolph GJ. Monocyte subsets differentially employ CCR2, CCR5, and CX3CR1 to accumulate within atherosclerotic plaques. J Clin Invest. 2007;117:185-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 960] [Cited by in RCA: 1085] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 49. | Feagan BG, Rutgeerts P, Sands BE, Hanauer S, Colombel JF, Sandborn WJ, Van Assche G, Axler J, Kim HJ, Danese S, Fox I, Milch C, Sankoh S, Wyant T, Xu J, Parikh A; GEMINI 1 Study Group. Vedolizumab as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2013;369:699-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1576] [Cited by in RCA: 1865] [Article Influence: 155.4] [Reference Citation Analysis (1)] |
| 50. | Ley K, Miller YI, Hedrick CC. Monocyte and macrophage dynamics during atherogenesis. Arterioscler Thromb Vasc Biol. 2011;31:1506-1516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 451] [Cited by in RCA: 431] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 51. | Robbins CS, Hilgendorf I, Weber GF, Theurl I, Iwamoto Y, Figueiredo JL, Gorbatov R, Sukhova GK, Gerhardt LM, Smyth D, Zavitz CC, Shikatani EA, Parsons M, van Rooijen N, Lin HY, Husain M, Libby P, Nahrendorf M, Weissleder R, Swirski FK. Local proliferation dominates lesional macrophage accumulation in atherosclerosis. Nat Med. 2013;19:1166-1172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 682] [Cited by in RCA: 824] [Article Influence: 68.7] [Reference Citation Analysis (0)] |
| 52. | Khallou-Laschet J, Varthaman A, Fornasa G, Compain C, Gaston AT, Clement M, Dussiot M, Levillain O, Graff-Dubois S, Nicoletti A, Caligiuri G. Macrophage plasticity in experimental atherosclerosis. PLoS One. 2010;5:e8852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 374] [Cited by in RCA: 418] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 53. | Ait-Oufella H, Taleb S, Mallat Z, Tedgui A. Recent advances on the role of cytokines in atherosclerosis. Arterioscler Thromb Vasc Biol. 2011;31:969-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 417] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 54. | Ridker PM, Libby P, MacFadyen JG, Thuren T, Ballantyne C, Fonseca F, Koenig W, Shimokawa H, Everett BM, Glynn RJ. Modulation of the interleukin-6 signalling pathway and incidence rates of atherosclerotic events and all-cause mortality: analyses from the Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS). Eur Heart J. 2018;39:3499-3507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 388] [Article Influence: 64.7] [Reference Citation Analysis (0)] |
| 55. | Sandborn WJ, Su C, Sands BE, D'Haens GR, Vermeire S, Schreiber S, Danese S, Feagan BG, Reinisch W, Niezychowski W, Friedman G, Lawendy N, Yu D, Woodworth D, Mukherjee A, Zhang H, Healey P, Panés J; OCTAVE Induction 1, OCTAVE Induction 2, and OCTAVE Sustain Investigators. Tofacitinib as Induction and Maintenance Therapy for Ulcerative Colitis. N Engl J Med. 2017;376:1723-1736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 896] [Cited by in RCA: 1189] [Article Influence: 148.6] [Reference Citation Analysis (0)] |
| 56. | Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE. ACG Clinical Guideline: Management of Crohn's Disease in Adults. Am J Gastroenterol. 2018;113:481-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 930] [Article Influence: 132.9] [Reference Citation Analysis (0)] |
| 57. | Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am J Gastroenterol. 2019;114:384-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 870] [Cited by in RCA: 1041] [Article Influence: 173.5] [Reference Citation Analysis (0)] |
| 58. | Patel SH, Rachchh MA, Jadav PD. Evaluation of anti-inflammatory effect of anti-platelet agent-clopidogrel in experimentally induced inflammatory bowel disease. Indian J Pharmacol. 2012;44:744-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 59. | Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ; CANTOS Trial Group. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med. 2017;377:1119-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4997] [Cited by in RCA: 6586] [Article Influence: 823.3] [Reference Citation Analysis (0)] |
| 60. | Fumery M, Singh AG, Khera R, Prokop L, Sandborn WJ, Curtis JR, Singh S. Biologic Therapy and Immunodulators are Associated with Decreased Risk of Cardiovascular Events in Patients with Immune-Mediated Inflammatory Diseases: A Systematic Review and Meta-Analysis. Gastroenterology. 2017;152:S77. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 61. | Zanoli L, Ozturk K, Cappello M, Inserra G, Geraci G, Tuttolomondo A, Torres D, Pinto A, Duminuco A, Riguccio G, Aykan MB, Mulé G, Cottone S, Perna AF, Laurent S, Fatuzzo P, Castellino P, Boutouyrie P. Inflammation and Aortic Pulse Wave Velocity: A Multicenter Longitudinal Study in Patients With Inflammatory Bowel Disease. J Am Heart Assoc. 2019;8:e010942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |