Copyright
©The Author(s) 2016.
World J Radiol. Oct 28, 2016; 8(10): 819-828
Published online Oct 28, 2016. doi: 10.4329/wjr.v8.i10.819
Published online Oct 28, 2016. doi: 10.4329/wjr.v8.i10.819
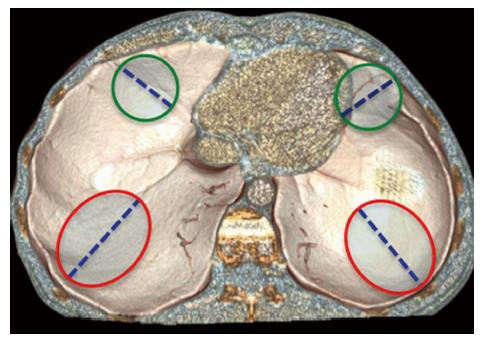
Figure 1 Physiological weakness points of the diaphragm.
This volume-rendering reconstruction shows the most common sites of diaphragm rupture, which are located in the postero-lateral area (red circles) and in the antero-medial area (green circles) of each hemidiaphragm. Blunt diaphragmatic lesions usually show radial course (dotted lines).
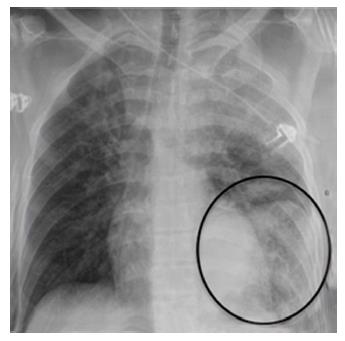
Figure 2 Chest X-ray findings in blunt diaphragmatic lesions.
This antero-posterior chest X-ray shows viscera herniation in the thoracic cavity (circle) in association with costophrenic sulcus obliteration and distorted diaphragmatic profile.
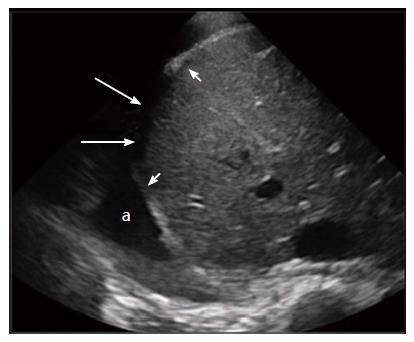
Figure 3 Sonographic findings in blunt diaphragmatic lesions.
This transversal ultrasound scan directly shows the ruptured right hemidiaphragm (arrows) surrounded by thickened diaphragm edges (arrowheads). A good acoustic window is present due to a large pleural effusion (a).
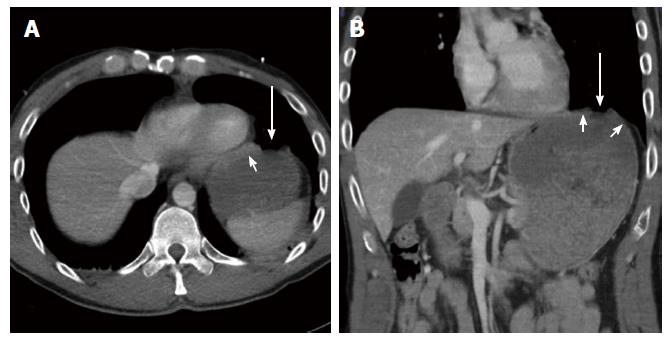
Figure 4 Computed tomography findings in blunt diaphragmatic lesions - segmental defect.
These 3 mm thick axial (A) and coronal (B) multiplanar reconstructions show a segmental diaphragmatic defect (arrows) surrounded by diaphragmatic thickening that indicates muscle retraction (arrowheads).
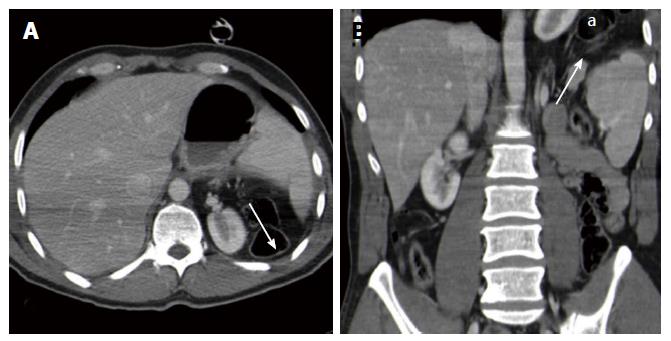
Figure 5 Computed tomography findings in blunt diaphragmatic lesions - diaphragm non-visualization.
These 3 mm thick axial (A) and coronal (B) multiplanar reconstructions show a lack of diaphragm visualization, without the clear demonstration of a tear (arrows), associated with intra-thoracic viscera herniation (a).
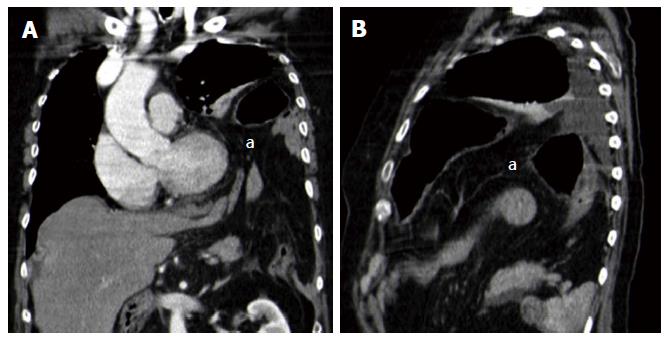
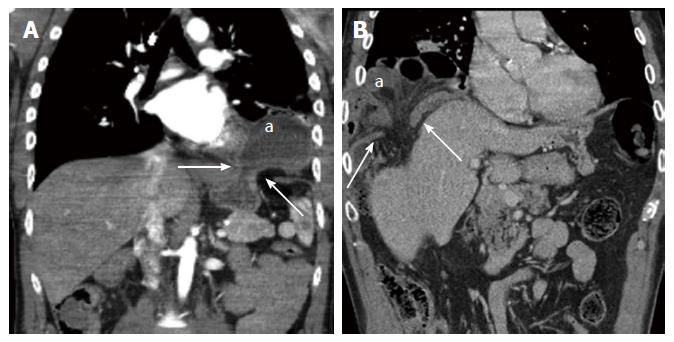
Figure 6 Computed tomography findings in blunt diaphragmatic lesions - intrathoracic viscera herniation.
These 3 mm thick coronal (A) and sagittal (B) multiplanar reconstructions show intrathoracic herniation of abdominal organs and fat (a). This finding is often associated with diaphragm non-visualization or with large diaphragmatic defects.
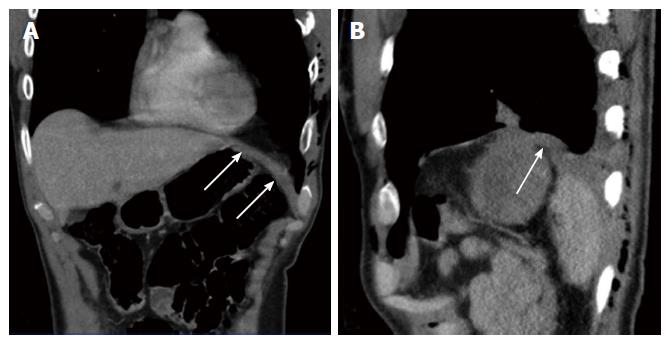
Figure 7 Computed tomography findings in blunt diaphragmatic lesions - diaphragm thickening.
These 3 mm thick coronal (A) and sagittal (B) multiplanar reconstructions show an abnormally thickened left hemidiaphragm (arrows), highly suspicious for blunt diaphragmatic lesions in a patients with multiple ribs fractures and pneumothorax.
Figure 8 Computed tomography findings in blunt diaphragmatic lesions - dangling diaphragm sign.
This 3 mm thick multiplanar axial reconstruction shows the free edges of a torn diaphragm as “comma-shaped” structures (arrows) which curl inward, toward the center of the abdomen. This alteration represents the so-called “dangling diaphragm sign”.
Figure 9 Computed tomography findings in blunt diaphragmatic lesions - dependent viscera sign.
These 3 mm thick multiplanar axial (A) and coronal (B) reconstructions show the spleen (arrows) and the stomach (a) lying on the posterior chest wall, without lung parenchyma interposition. This alteration represents the so-called “dependent viscera sign”.
Figure 10 Computed tomography findings in blunt diaphragmatic lesions - collar sign.
These 3 mm thick multiplanar coronal reconstructions (2 different patients, A and B) show intrathoracic herniation of the stomach (A, “a”) and of the right colic flexure (B, “a”). In both cases the herniated material shows a hourglass shape as a consequence of the compression exerted on it by the ruptured diaphragm edges (arrows).
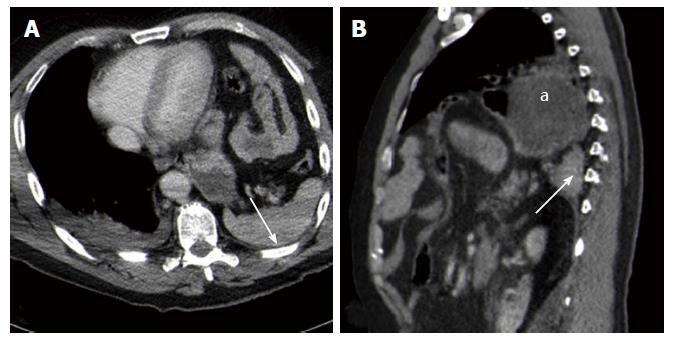
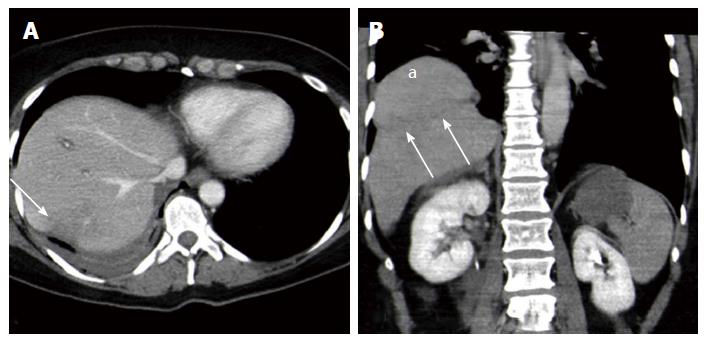
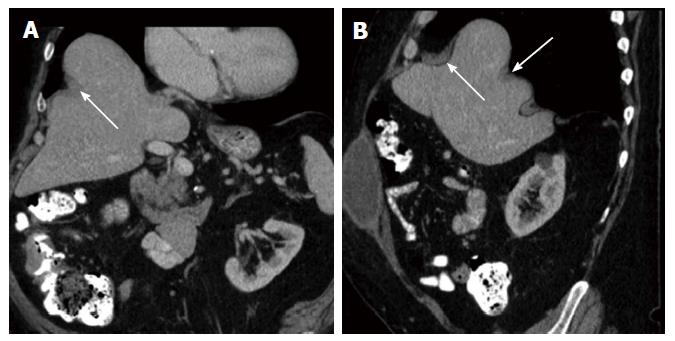
Figure 11 Computed tomography findings in blunt diaphragmatic lesions - hump and band sign.
These 3 mm thick multiplanar axial (A) and coronal (B) reconstructions show a hypodense band that crosses the liver parenchyma in the site where it crosses the ruptured diaphragm (arrows), whereas the liver dome expands above it. This alteration represents the so-called “hump and band sign” (a).
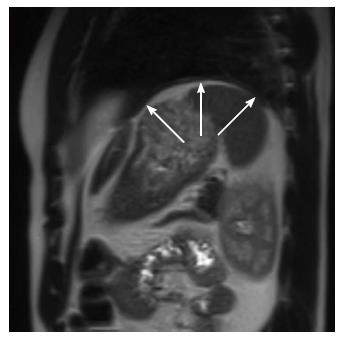
Figure 12 Magnetic resonance imaging apperarance of the diaphragm.
This TSE T2-weighted sagittal image shows the left hemidiaphragm as an uniformly thin intermediate signal intensity band (arrows) between lung parenchyma and intra-abdominal fat.
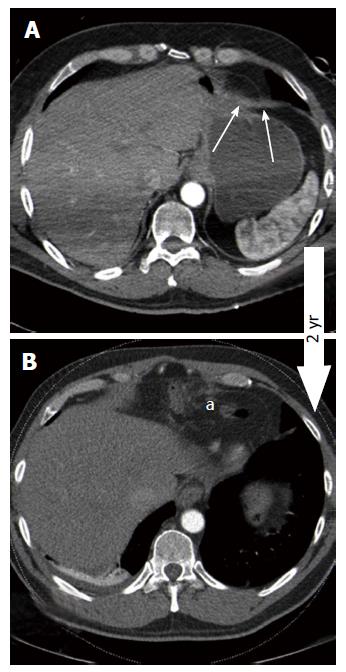
Figure 13 False negative case of blunt diaphragmatic lesions.
Three millimeters thick axial CT images of the same patient, acquired after a precipitation trauma (A) and two years later (B). Thickening of the antero-medial part of the left hemidiaphragm (A, arrows) was overlooked at the first CT scan, performed after a precipitation trauma. Two years later, a CT scan performed because of epigastric pain showed intra-thoracic viscera herniation (B, “a”) as a consequence of diaphragmatic rupture. CT: Computed tomography.
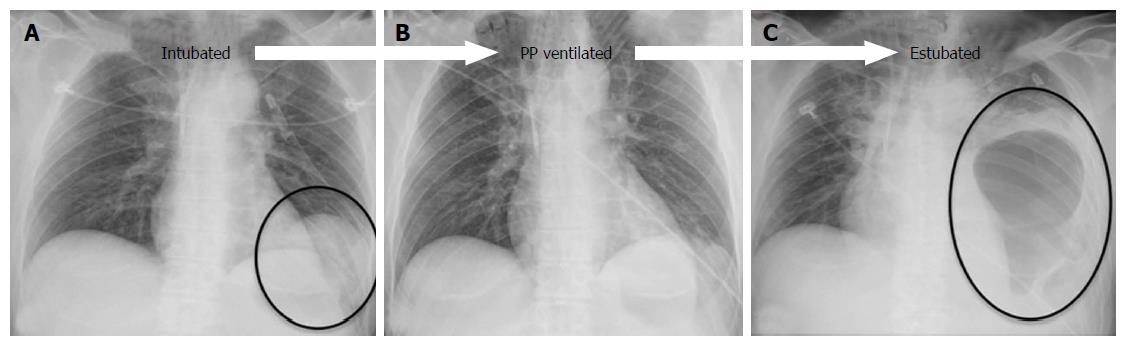
Figure 14 Effects of mechanical ventilation on blunt diaphragmatic lesions.
The antero-posterior chest X-ray, performed immediately after intubation and left pneumothorax drainage (A) in a patient admitted to the ED because of severe motorbike accident, showed a double left diaphragmatic profile (circle), suspicious for BDI. The finding was not confirmed at the subsequent CT, performed after the beginning of positive-pressure ventilation, and also the CXR performed 2 d later, after pleural drainage removal (B) did not show any diaphragm alteration. Three days later, after estubation, the patient suffered respiratory insufficiency and left pleural drainage was replaced in the suspicion of relapsing pneumothorax; subsequent CXR (C) clearly demonstrated the presence of BDI with intra-thoracic gastric herniation (circle). BDI: Blunt diaphragmatic lesions; CXR: Chest X-ray; CT: Computed tomography; ED: Emergency Department.
Figure 15 Diaphragm eventration.
A and B: Eventration may mimick blunt diaphragmatic lesions. In case of eventration diaphragm continuity (arrows) must always be recongnizable and no abrupt thickness changes should be observed.
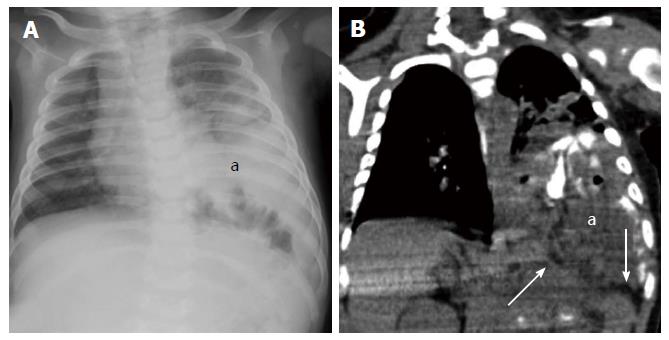
Figure 16 Congenital diaphragmatic hernia.
CXR (A) and CT scan (B) of a 3-mo-old patient with congenital left diaphragmatic hernia (a). The diaphragmatic edges are not thickened (arrows). CXR: Chest X-ray; CT: Computed tomography.
- Citation: Bonatti M, Lombardo F, Vezzali N, Zamboni GA, Bonatti G. Blunt diaphragmatic lesions: Imaging findings and pitfalls. World J Radiol 2016; 8(10): 819-828
- URL: https://www.wjgnet.com/1949-8470/full/v8/i10/819.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i10.819