Copyright
©2010 Baishideng Publishing Group Co.
World J Radiol. Jun 28, 2010; 2(6): 203-214
Published online Jun 28, 2010. doi: 10.4329/wjr.v2.i6.203
Published online Jun 28, 2010. doi: 10.4329/wjr.v2.i6.203
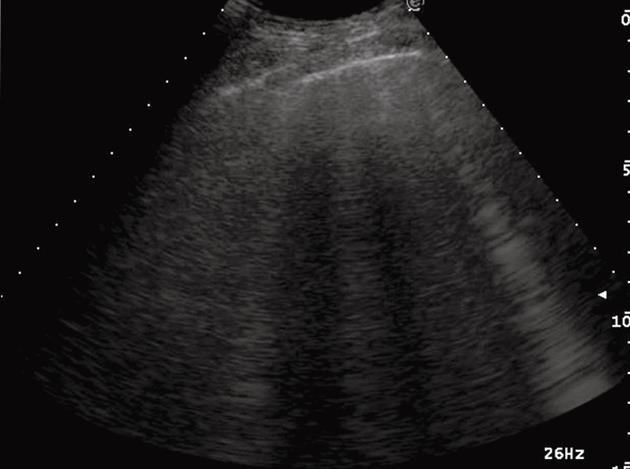
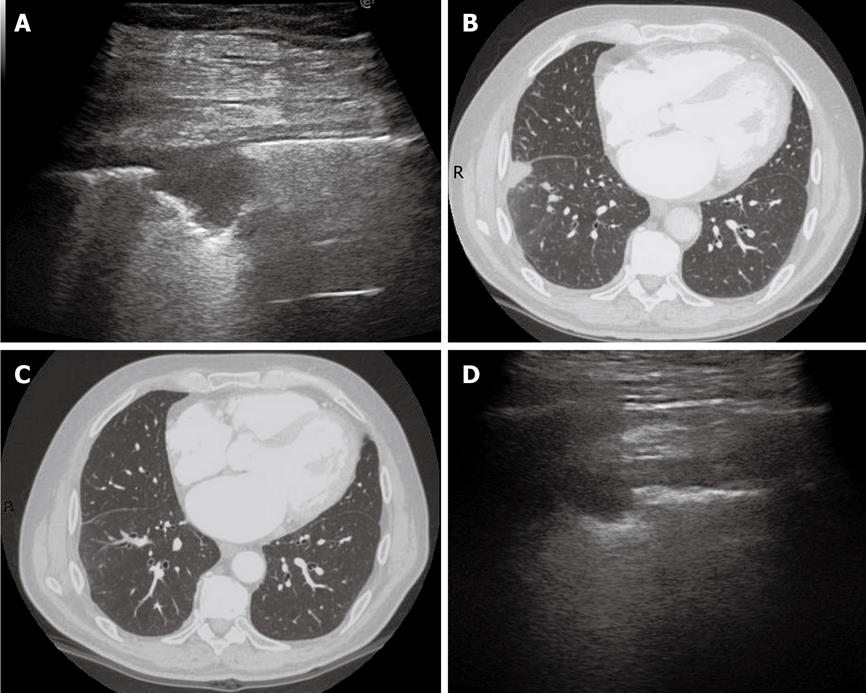
Figure 1 Ring-down artifacts, characterized by a series of hyperechoic, narrow-based bands spreading from the pleural line into the lung.
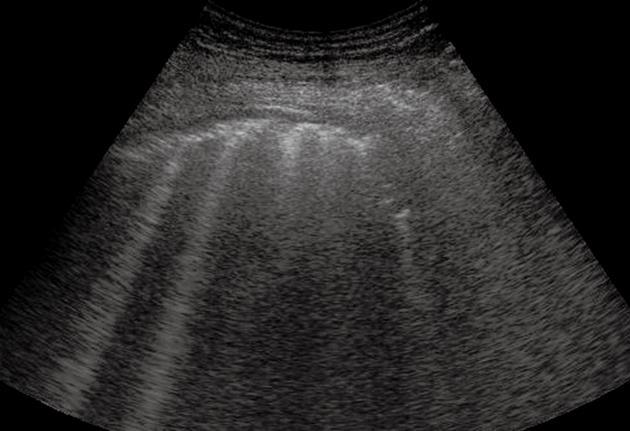
Figure 2 Pulmonary fibrosis.
Multiple comet-tail artifacts departing from a thickened and irregular pleural line.
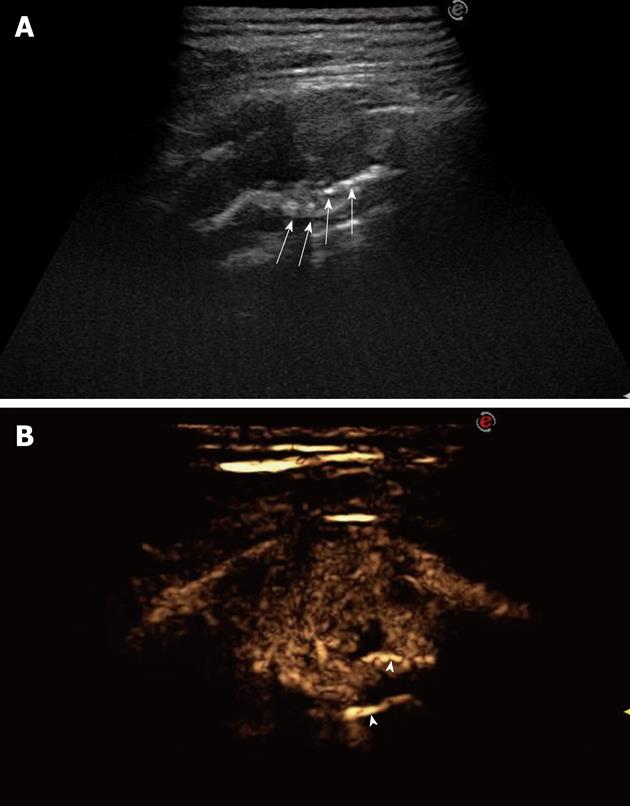
Figure 3 Pneumonia.
Posterior intercostal scan shows a hypoechoic consolidated area that contains multiple echogenic lines that represent an air bronchogram (arrows).
Figure 4 Post-stenotic pneumonia.
Posterior intercostal scan shows a hypoechoic consolidated area that contains anechoic, branched tubular structures in the bronchial tree (fluid bronchogram) (arrows).
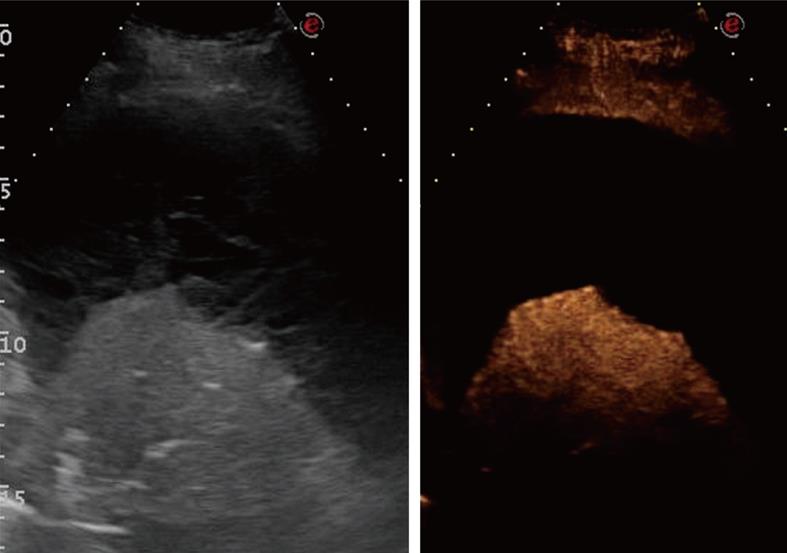
Figure 5 Contrast-enhanced ultrasonography of pneumonia.
A: Baseline scan shows a hypoechoic consolidated area; B: Seven seconds after iv bolus of contrast agent, the lesion shows marked and homogeneous enhancement; C: The lesion remains substantially unmodified after 90 s.
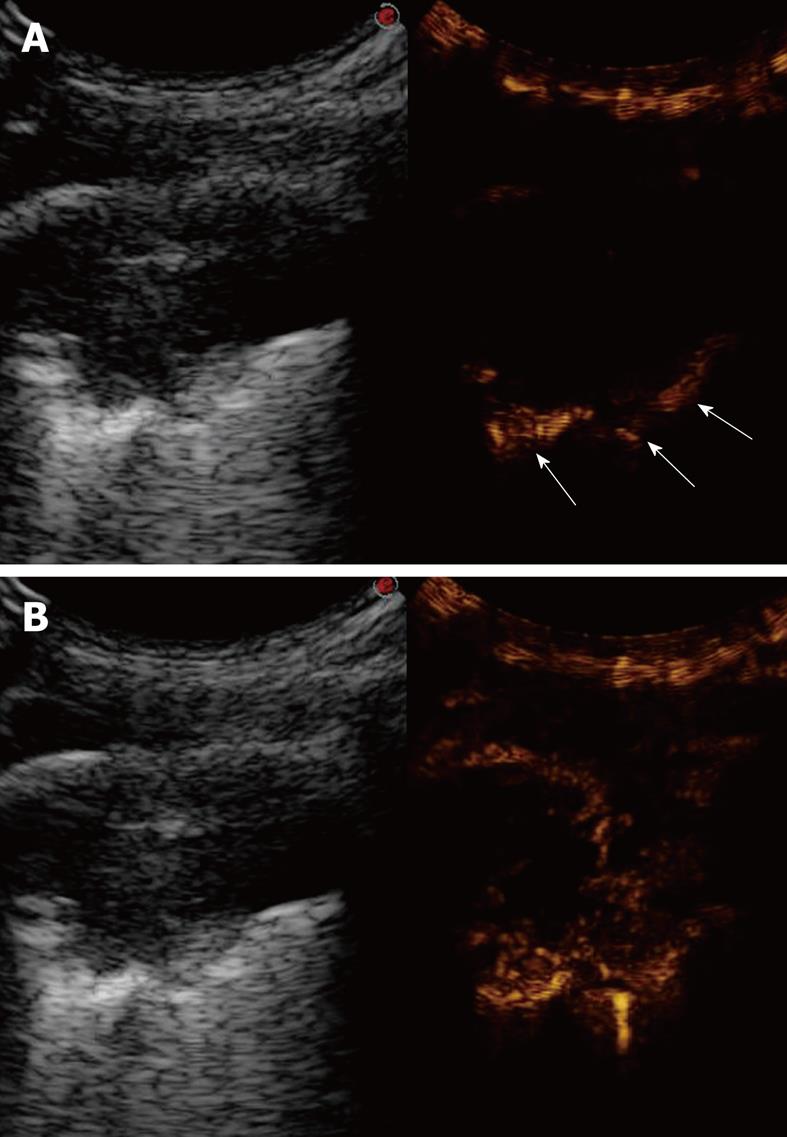
Figure 6 Contrast-enhanced ultrasonography evaluation of pneumonia with pleural effusion.
Baseline scan shows parenchymal consolidation with air bronchogram (arrows) and subtle surrounding effusion (arrowheads) (left side of the split-screen). After iv bolus of contrast agent, the consolidation is enhanced and better demarcated from the effusion (right side of the split-screen).
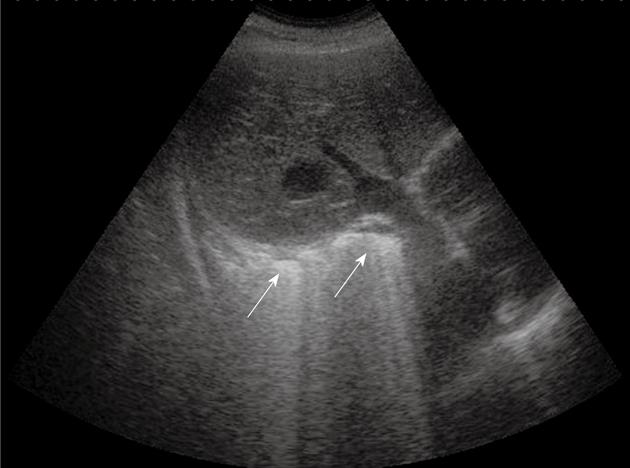
Figure 7 Pneumonia complicated by abscesses.
Multiple small collections of fluid are irregularly settled in a consolidated liver-like infiltrate. Loc: Loculation; Microloc: Microloculation.
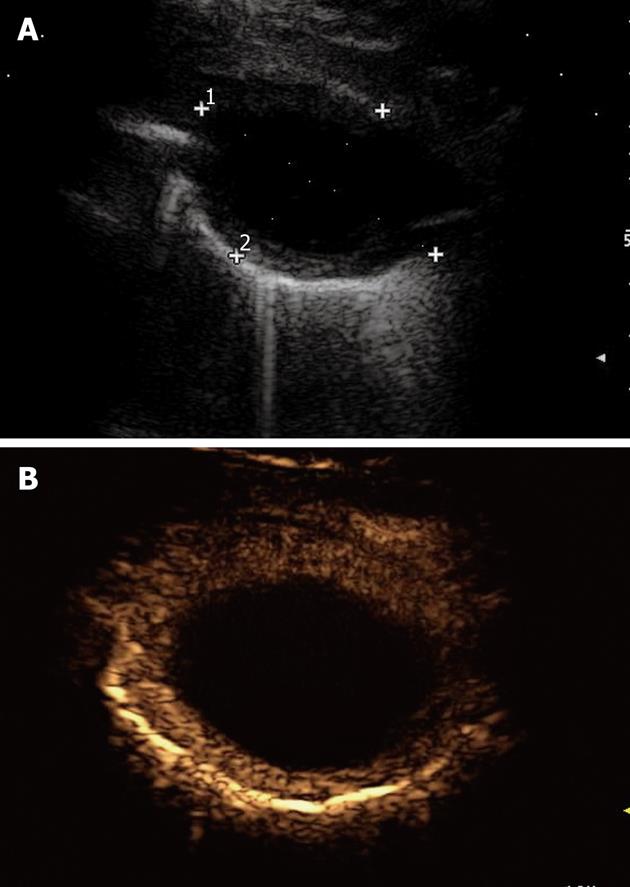
Figure 8 Lung abscess.
A: An anechoic oval lesion is surrounded by an echodense capsule; B: After iv bolus of contrast agent, the lesion shows no contrast agent uptake, whereas the capsule is strongly enhanced.
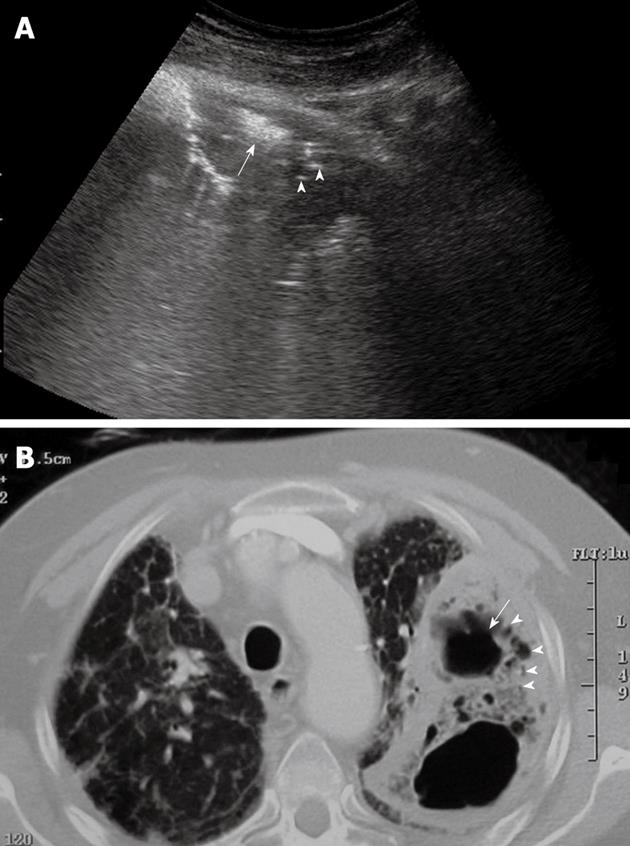
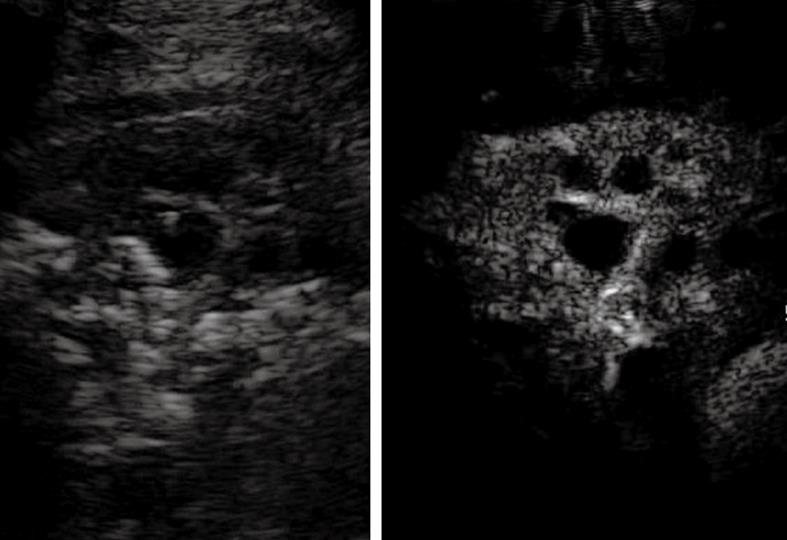
Figure 9 Lung abscess with air inside the lesion.
A: High amplitude echoes are clearly visible (arrow), as well as multiple echogenic small air inclusions (arrowheads); B: Corresponding computed tomography scan shows the same findings.
Figure 10 Pulmonary infarction.
Posterior intercostal scan shows a triangular-shaped hypoechoic lesion with central hyperechoic structures that indicate the presence of air occupying the affected bronchiole (arrows).
Figure 11 Dynamic course of pulmonary infarction.
A: Lateral intercostal scan of the right lung shows a typical triangular-shaped peripheral lesion; B: Likewise, computed tomography scan of the lateral segment of the lower right lobe shows a triangular pleural-based lesion with the vertex towards the hilum; C: After 40 d, the lesion is no longer visible by computed tomography scan; D: The lesion appears reduced in size at transthoracic ultrasonography examination.
Figure 12 Contrast-enhanced ultrasonography of pulmonary infarction.
After iv bolus of contrast agent, the lesion (the same one as in Figure 11A) shows no contrast agent uptake in the arterial phase, which suggests the absence of blood supply.
Figure 13 Compression atelectasis.
Posterior intercostal scan shows a liver-like consolidation with the typical shape of a jelly bag cap surrounded by pleural effusion.
Figure 14 Contrast-enhanced ultrasonography evaluation of compression atelectasis.
Baseline scan shows a liver-like consolidation surrounded by multiloculated pleural effusion (left side of the split-screen). Twelve seconds after iv bolus of contrast agent, the consolidation shows marked and homogeneous enhancement, whereas pleural effusion shows no enhancement.
Figure 15 Adult respiratory distress syndrome.
Oblique subcostal scan through the right lobe of the liver shows the typical transthoracic ultrasonography pattern of intense retro-phrenic hyperechogenicity due to complete reverberation of the US beam (arrows).
Figure 16 Peripheral bronchial carcinoma.
Posterior intercostal scan shows a hypoechoic consolidation with relatively well-delineated borders. The air bronchogram is absent.
Figure 17 Contrast-enhanced ultrasonography evaluation of bronchial carcinoma.
Baseline scan shows consolidation with inhomogeneous echotexture (left side of the split-screen). Twenty seconds after iv bolus of contrast agent, necrotic areas can be depicted as anechoic regions inside the enhanced viable tumor (right side of the split-screen).
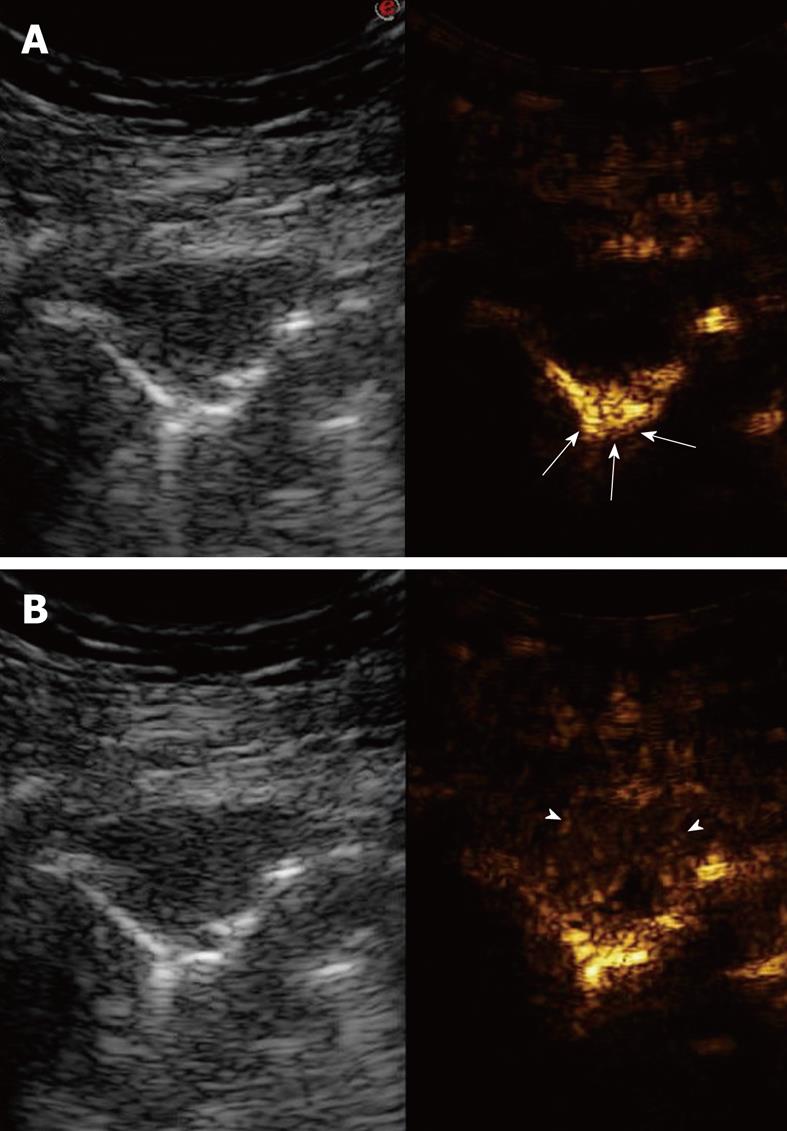
Figure 18 Bronchial carcinoma infiltrating the pleural wall.
A: Posterior intercostal scan shows a hypoechoic lesion accompanied by rib destruction (arrows); B: Twenty-four seconds after iv bolus of contrast agent, the lesion appears inhomogeneously enhanced; the disrupted rib appears more echogenic than the tumor (arrowheads), as a consequence of the incomplete tissue suppression due to the strong echogenicity of bone tissue.
Figure 19 Contrast-enhanced ultrasonography of bronchial carcinoma.
A: Baseline scan shows a hypoechoic lesion with irregular borders (left side of the split-screen). Ten seconds after iv bolus of contrast agent, the pulmonary parenchyma near the lesion is already enhanced (arrows), whereas the lesions is still unenhanced (right side of the split-screen); B: Twenty seconds later, the lesion shows delayed inhomogeneous enhancement, which indicates a preferential bronchial arterial supply (right side of the split-screen).
Figure 20 Pulmonary metastasis.
Posterior intercostal scan shows a round-shaped, clear-bordered lesion.
Figure 21 Contrast-enhanced ultrasonography of pulmonary metastasis.
A: Baseline scan shows a small hypoechoic lesion (left side of the split-screen). Ten seconds after iv bolus of contrast agent, the lesion appears unenhanced with respect to the early enhancement of the pulmonary parenchyma (arrows) (right side of the split-screen); B: Fifty seconds later, the lesion shows inhomogeneous enhancement with reduced contrast agent extent (arrowhead) with respect to the pulmonary parenchyma (right side of the split-screen).
- Citation: Sartori S, Tombesi P. Emerging roles for transthoracic ultrasonography in pulmonary diseases. World J Radiol 2010; 2(6): 203-214
- URL: https://www.wjgnet.com/1949-8470/full/v2/i6/203.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i6.203