Copyright
©The Author(s) 2020.
World J Radiol. Apr 28, 2020; 12(4): 29-47
Published online Apr 28, 2020. doi: 10.4329/wjr.v12.i4.29
Published online Apr 28, 2020. doi: 10.4329/wjr.v12.i4.29
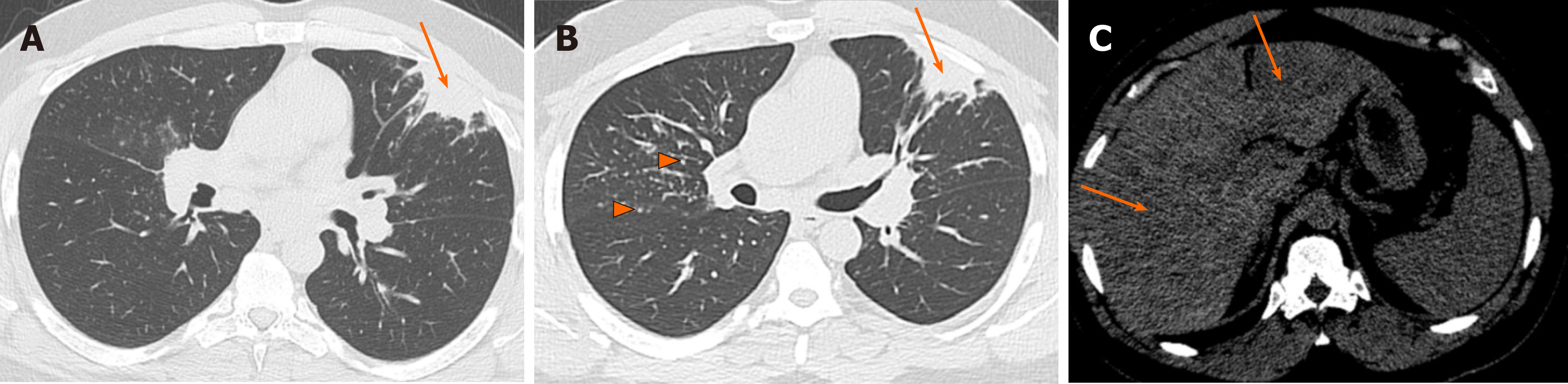
Figure 1 Alveolar sarcoidosis.
A and B: Non-contrast computed tomography of the chest, lung window at baseline (A) and after 5 mo (B) in a 46-year-old man with cough and biopsy-proven sarcoidosis. Pleural-based consolidative opacity remained unchanged (arrows). Typical sarcoidosis findings of peribronchovascular and perilymphatic nodularity can be well-seen in the follow-up image (arrowhead in B); C: The liver was also involved with subtle hypodense lesions in the right and left hepatic lobes (arrows).
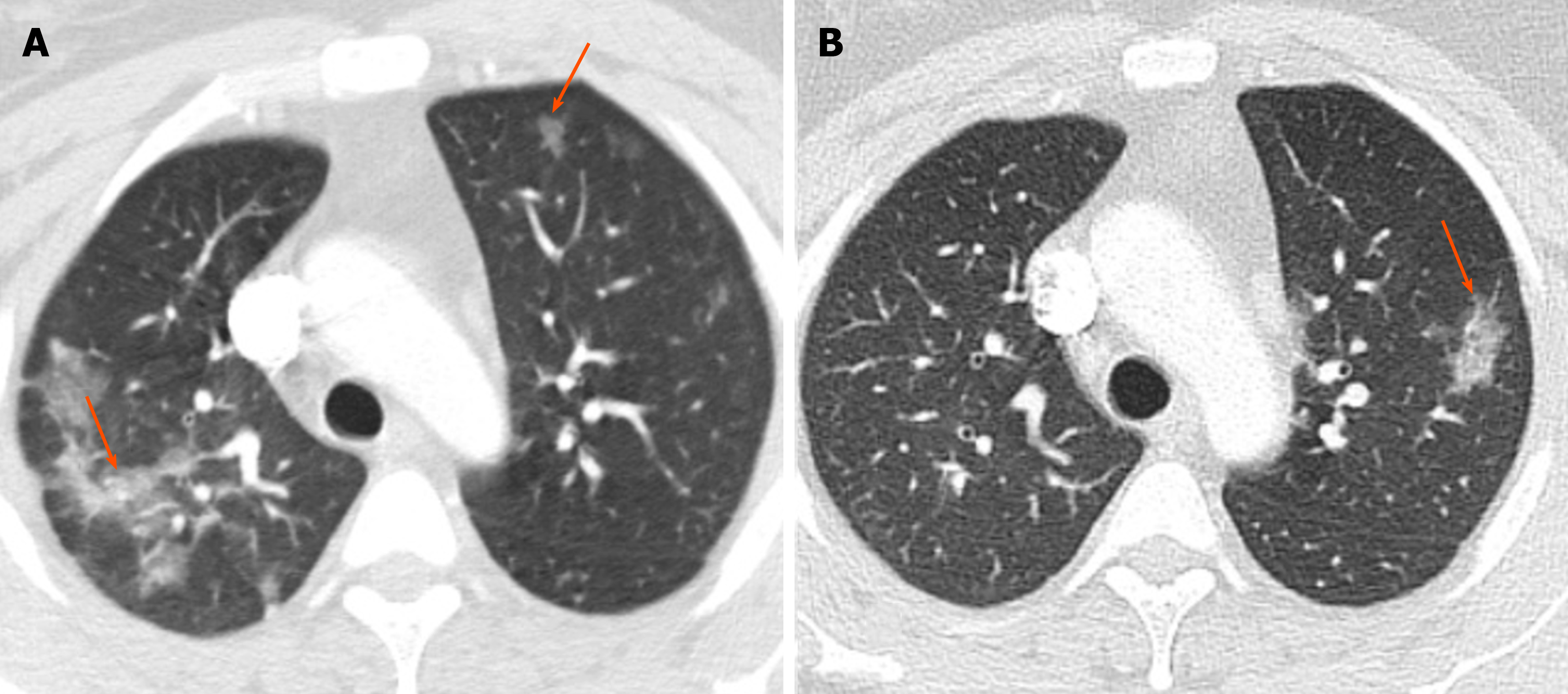
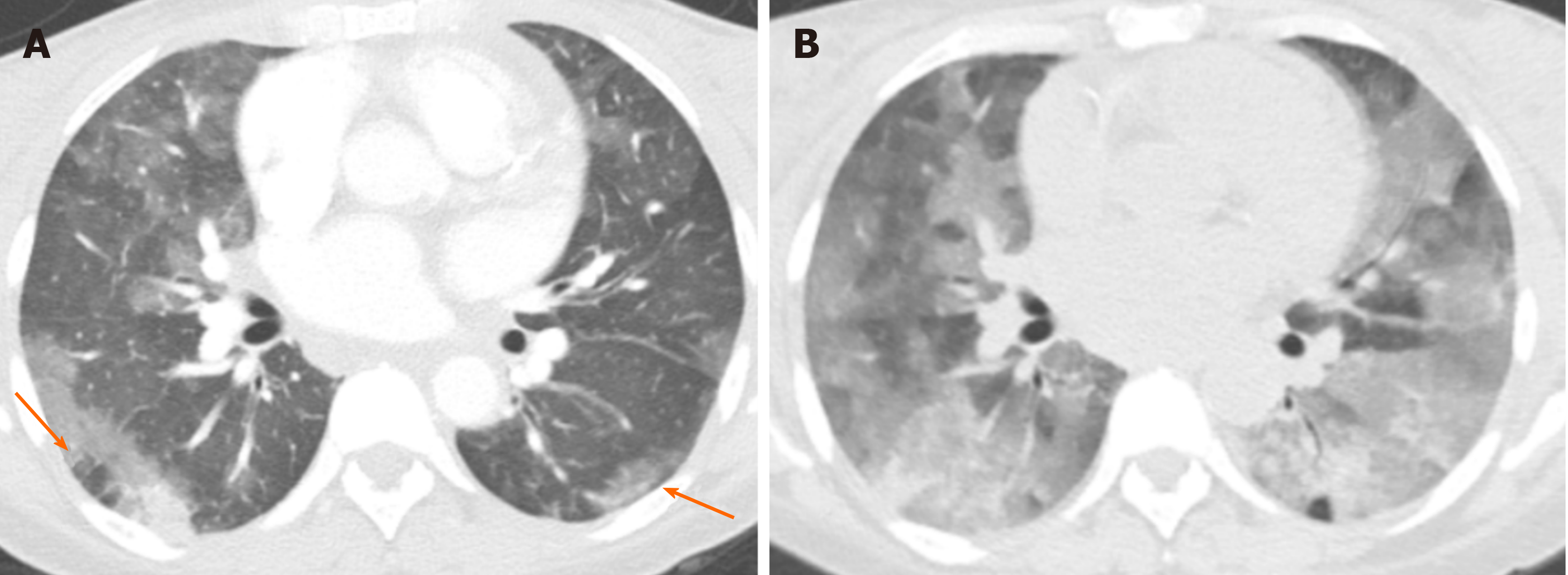
Figure 2 Chronic eosinophilic pneumonia.
A: Baseline non-contrast chest computed tomography in a 38-year-old woman with history of asthma, eosinophilia and eosinophilic pneumonia, who presented with shortness of breath, showed bilateral patchy airspace opacities in both upper lobes (arrows); B: Follow-up chest computed tomography after 8 mo showed resolution of the previous opacities with interval development of an area of patchy consolidation in the left upper lobe (arrow).
Figure 3 Organizing pneumonia.
A: Contrast-enhanced computed tomography (CT) of the chest in lung window in a 52-year-old woman with rheumatoid arthritis presenting with chest pain and shortness of breath. CT was negative for pulmonary embolism but showed pleural-based patchy opacities and consolidations (arrows); B: Follow-up chest CT after 3 mo showed persistent pleural-based opacities in the lungs (arrows). Suture material is seen in the right lobe opacity (arrowhead), in keeping with post-biopsy changes, which confirmed organizing pneumonia; C: Axial CT image more superiorly demonstrated development of a new area of ground glass opacity with a rim of more solid consolidation (reverse halo sign) as well as secondary to organizing pneumonia (arrow).
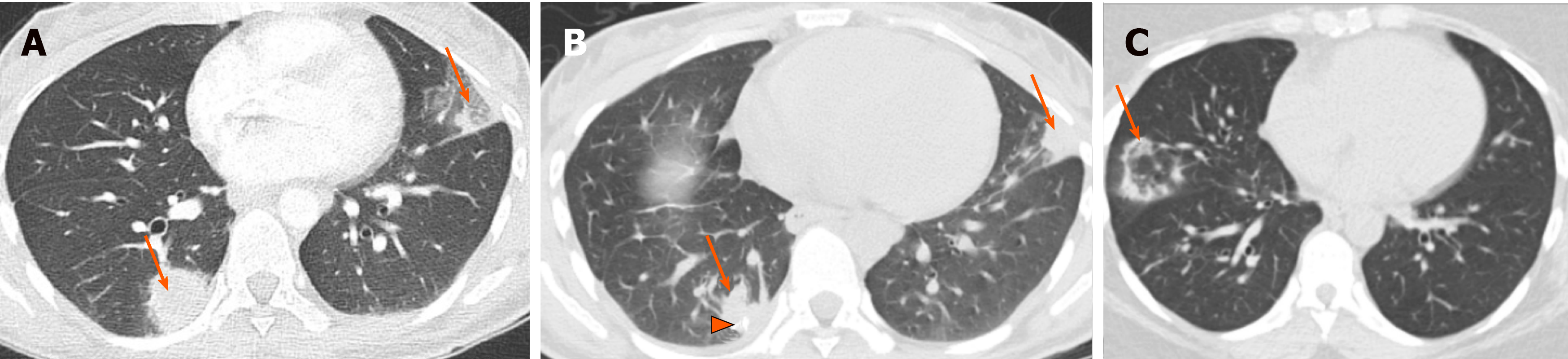
Figure 4 Eosinophilic granulomatosis with polyangiitis.
A 53-year-old female with history of asthma presented with shortness of breath. A: Computed tomography of the chest at baseline shows poorly defined, randomly distributed areas of airspace ground glass opacity (arrows); B: Follow-up computed tomography after 4 mo demonstrated persistent but improved areas of ground glass opacity in a slightly different distribution than in the baseline image (arrows).
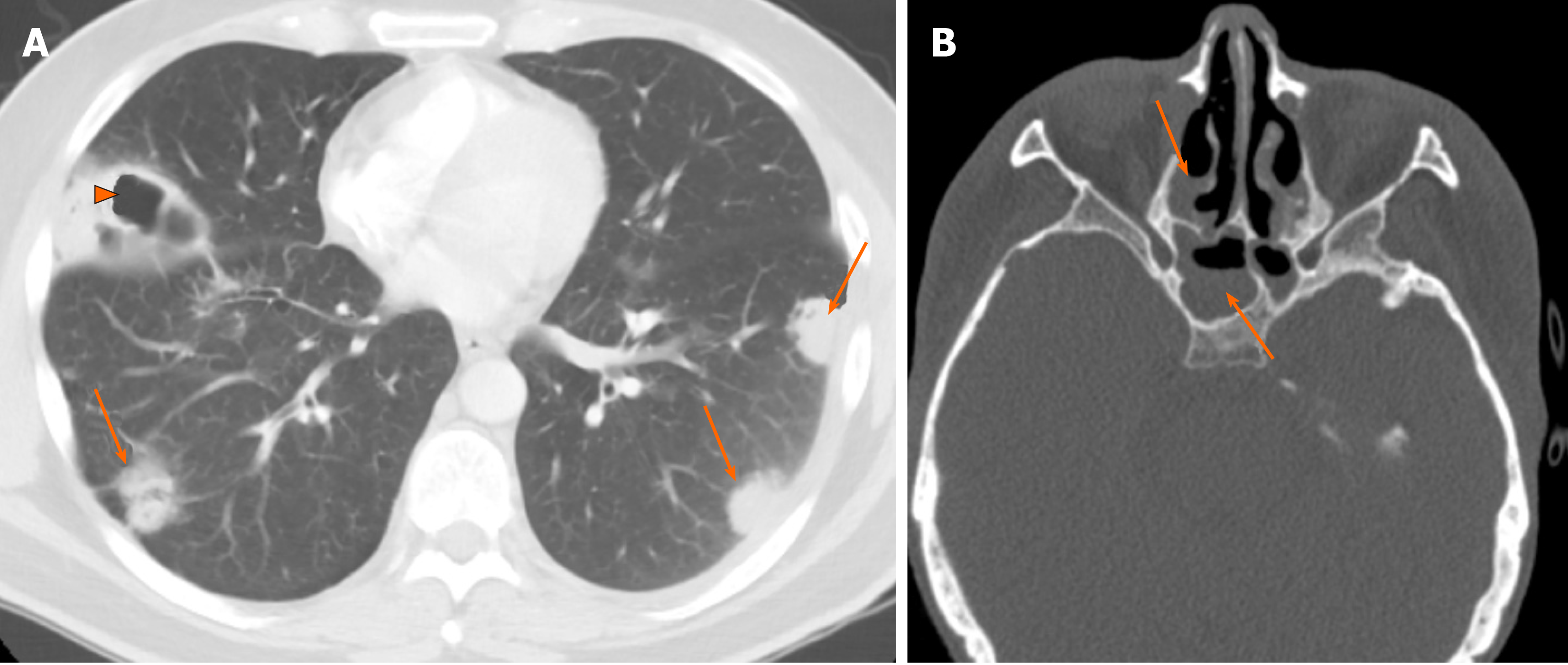
Figure 5 Granulomatosis with polyangiitis.
A 38-year-old male with hemoptysis and shortness of breath. A: Non-contrast enhanced computed tomography of the chest (A) showed multiple randomly distributed nodules/masses and round consolidative opacities in both lungs (arrows), with areas of cavitation (arrowheads); B: Head computed tomography showed involvement of bilateral sphenoid sinuses and ethmoidal air cells (arrows) in keeping with pan-sinusitis.
Figure 6 Pembrolizumab-induced pneumonitis.
A 75-year-old woman with mesothelioma on pembrolizumab presented with shortness of breath. A: Non-contrast chest computed tomography in lung window showed multifocal consolidative opacities in both lungs (arrows), raising concern for pneumonitis. Treatment with pembrolizumab was discontinued; B: Follow-up chest computed tomography after 2 mo showed interval resolution/improvement of some of the consolidative opacities, while new consolidations have developed (arrows).
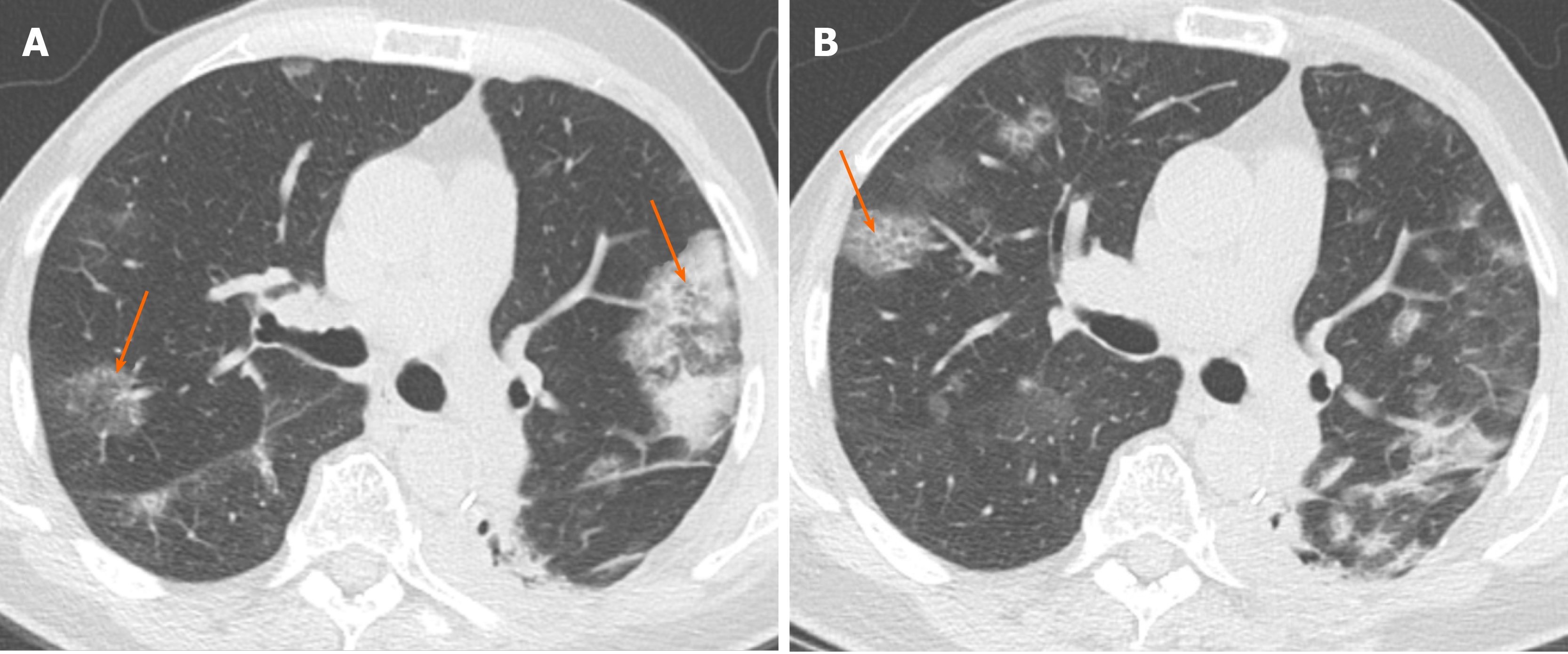
Figure 7 Angio-invasive aspergillosis.
A 35-year-old woman with history of acute myeloid leukemia and severe neutropenia presented with cough and pleuritic chest pain. A: Computed tomography of the chest at the time of presentation showed a wedge-shaped pleural-based opacity (*) and consolidation with peripheral ground glass opacity (arrow) consistent with a halo sign, highly concerning for angio-invasive aspergillosis given the history; B: Despite appropriate therapy, the opacity persisted on 6 wk follow-up chest computed tomography (arrow).
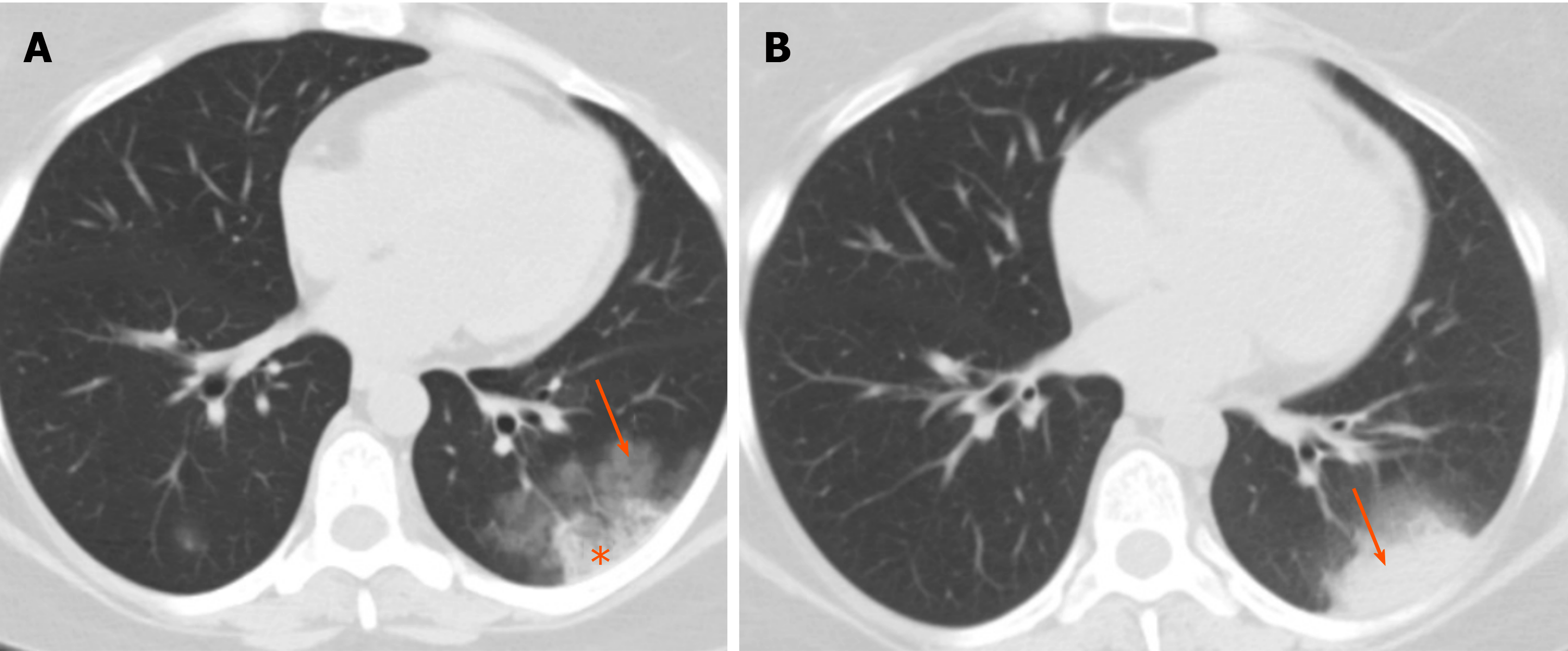
Figure 8 Mycobacterial tuberculosis.
A 49-year-old man with cough and hemoptysis. A: Large area of consolidation was present in the right upper lobe, with small areas of cavitation (arrows); B: There was a significant amount of airspace opacity in the ipsilateral lung involving all three lobes, with areas of tree-in-bud nodularity (arrows) keeping with an endobronchial spread of infection.
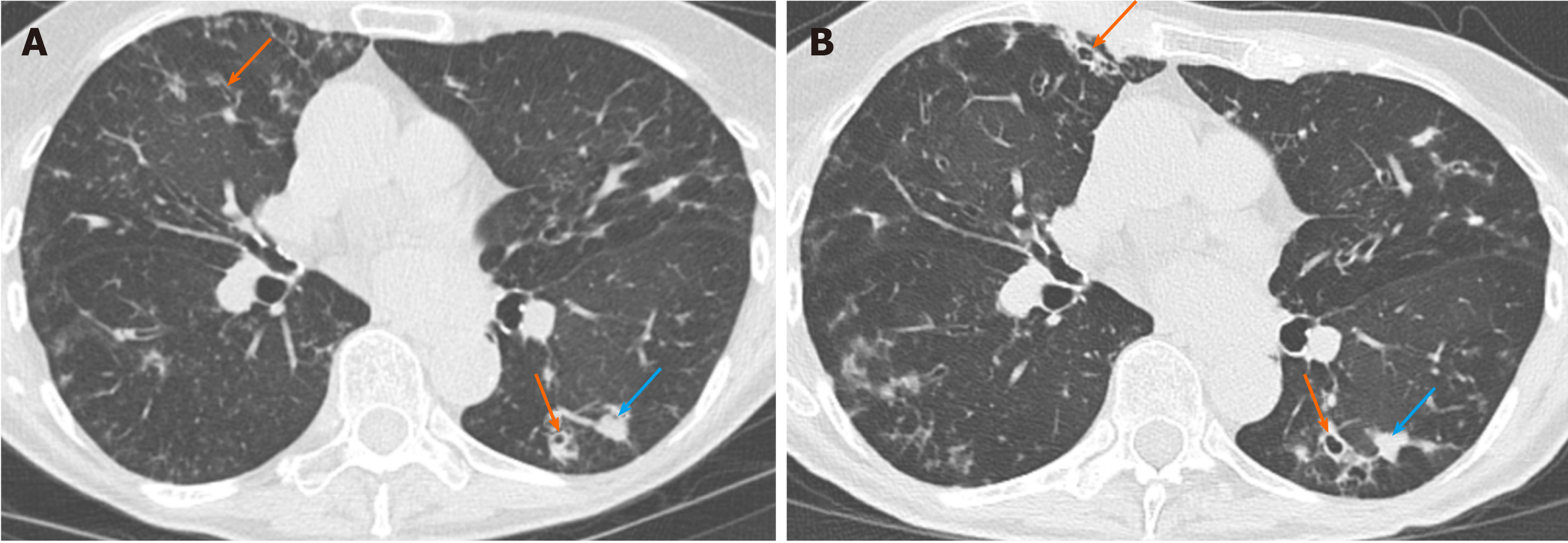
Figure 9 Mycobacterium avium complex infection.
A 79-year-old woman with cough. A and B: Baseline (A) and follow-up chest computed tomography after 11 mo (B) showed no significant change in areas of bronchiectasis and bronchial wall thickening (orange arrows) as well as areas of more focal consolidation (blue arrows).
Figure 10 Pneumocystis jirovecii infection.
A 43-year-old man with human immunodeficiency virus infection who presented with shortness of breath and fever. A: Contrast-enhanced computed tomography of the chest in lung window at presentation showed extensive ground glass opacity in both lungs, with a more focal consolidative opacity in the left lung (arrow); B: Follow-up computed tomography 3 mo after treatment showed improvement in ground glass opacity, with residual interlobular septal thickening and the ground glass opacity causing crazy paving appearance (arrows).
Figure 11 Adenocarcinoma in situ.
A: A 77-year-old woman with a right upper lobe ground glass nodule (arrow), with a small internal solid nodule component (arrowhead) keeping with the fried-egg sign; B: Fluorodeoxyglucose-positron emission tomography showed mild increased metabolic activity (arrow, SUV 2.2). Adenocarcinoma was confirmed after wedge resection.
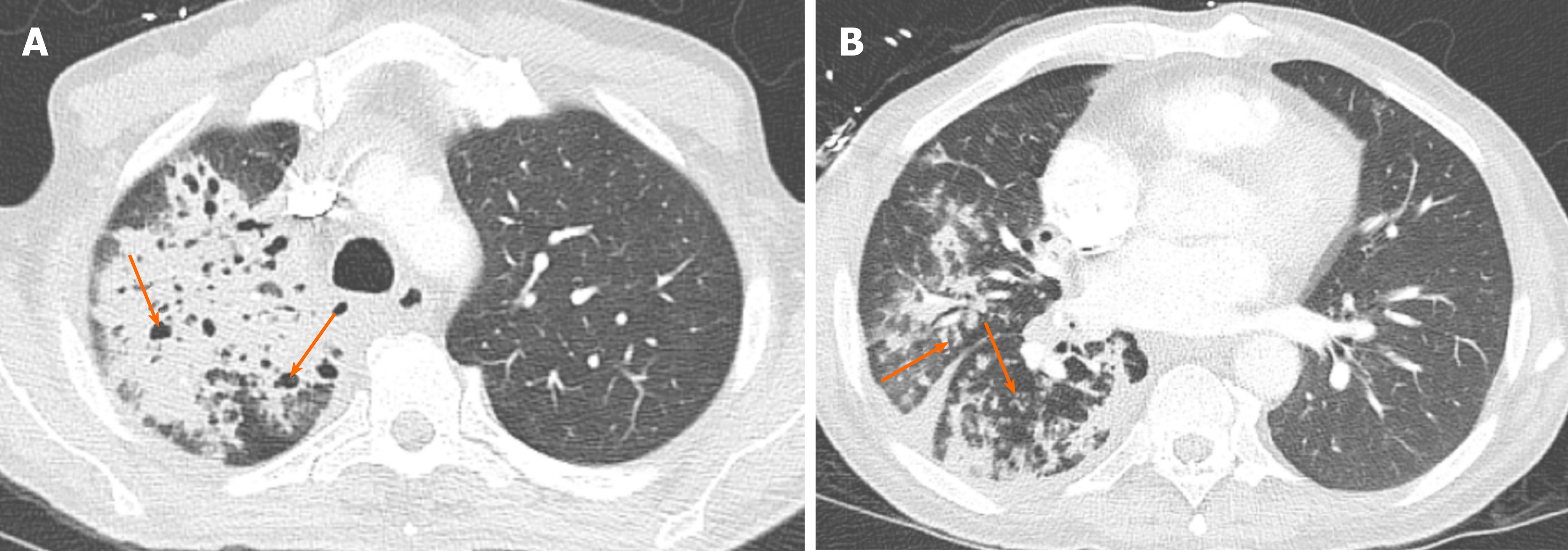
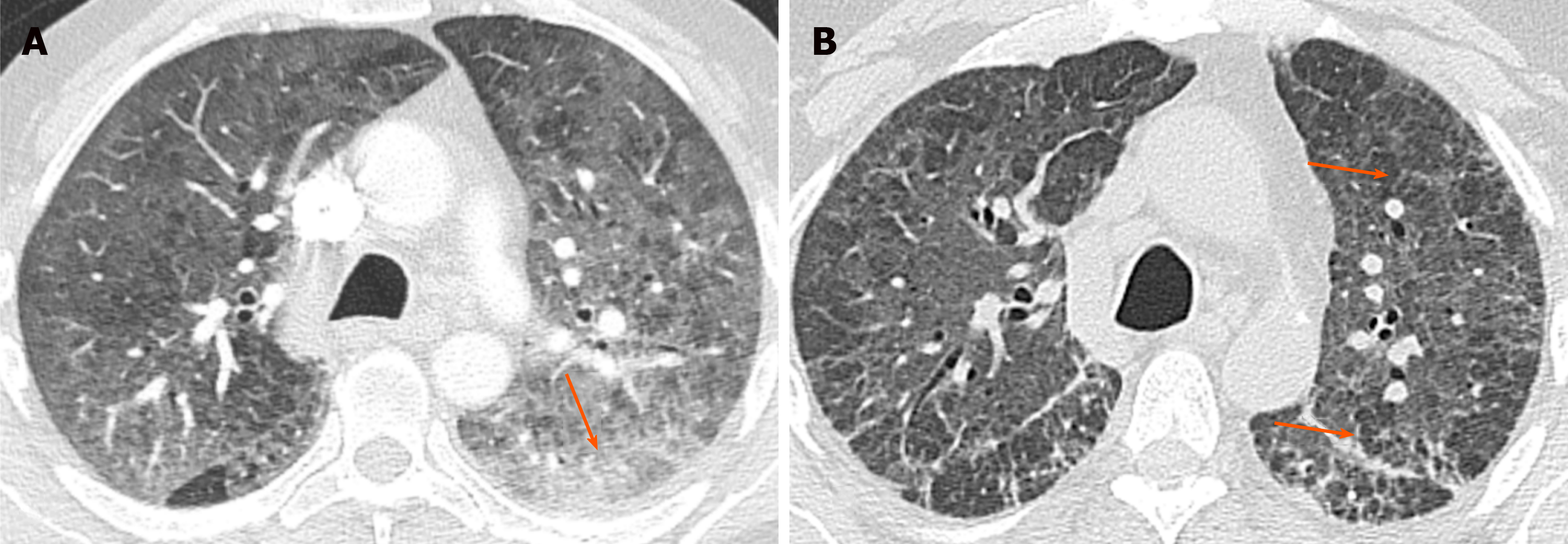
Figure 12 Invasive adenocarcinoma.
A and B: An 81-year-old man with multiple areas of patchy and confluent airspace opacity in both lower lobes (A, arrows), which increased in size and extent at 6 mo follow-up chest computed tomography (B, arrows). Biopsy confirmed the multifocal invasive mucinous adenocarcinoma.
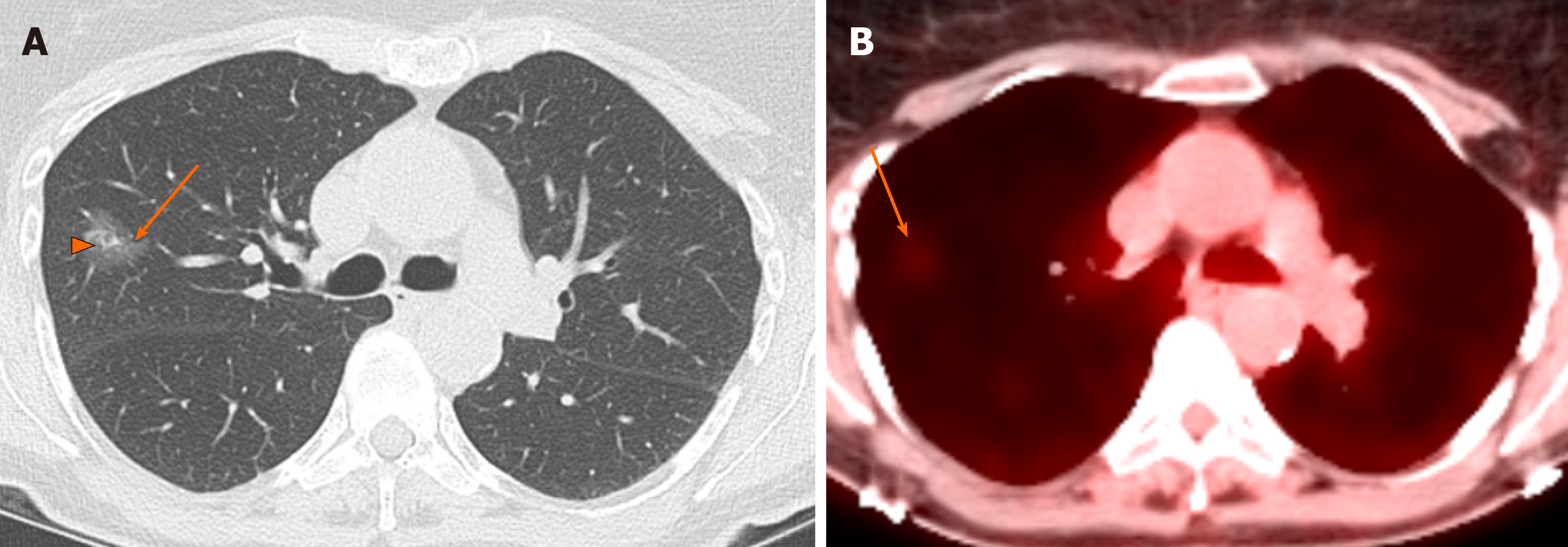
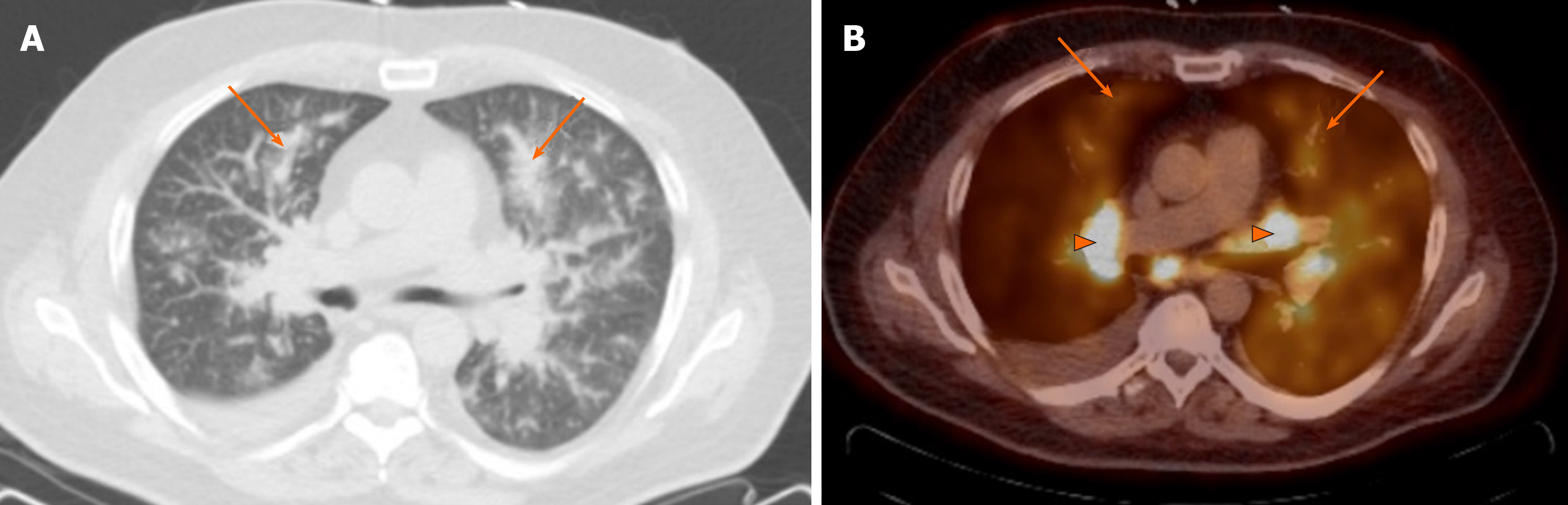
Figure 13 Pulmonary lymphoma.
A 64-year-old man with biopsy proven B cell lymphoma based on biopsy of a hepatic lesion. Chest CT in lung window (A) shows extensive patchy ground glass and consolidative opacities (arrows). PET-CT (B) shows increased FDG uptake in the peri-hilar opacities (arrows) as well as in the enlarged lymph nodes (arrow heads).
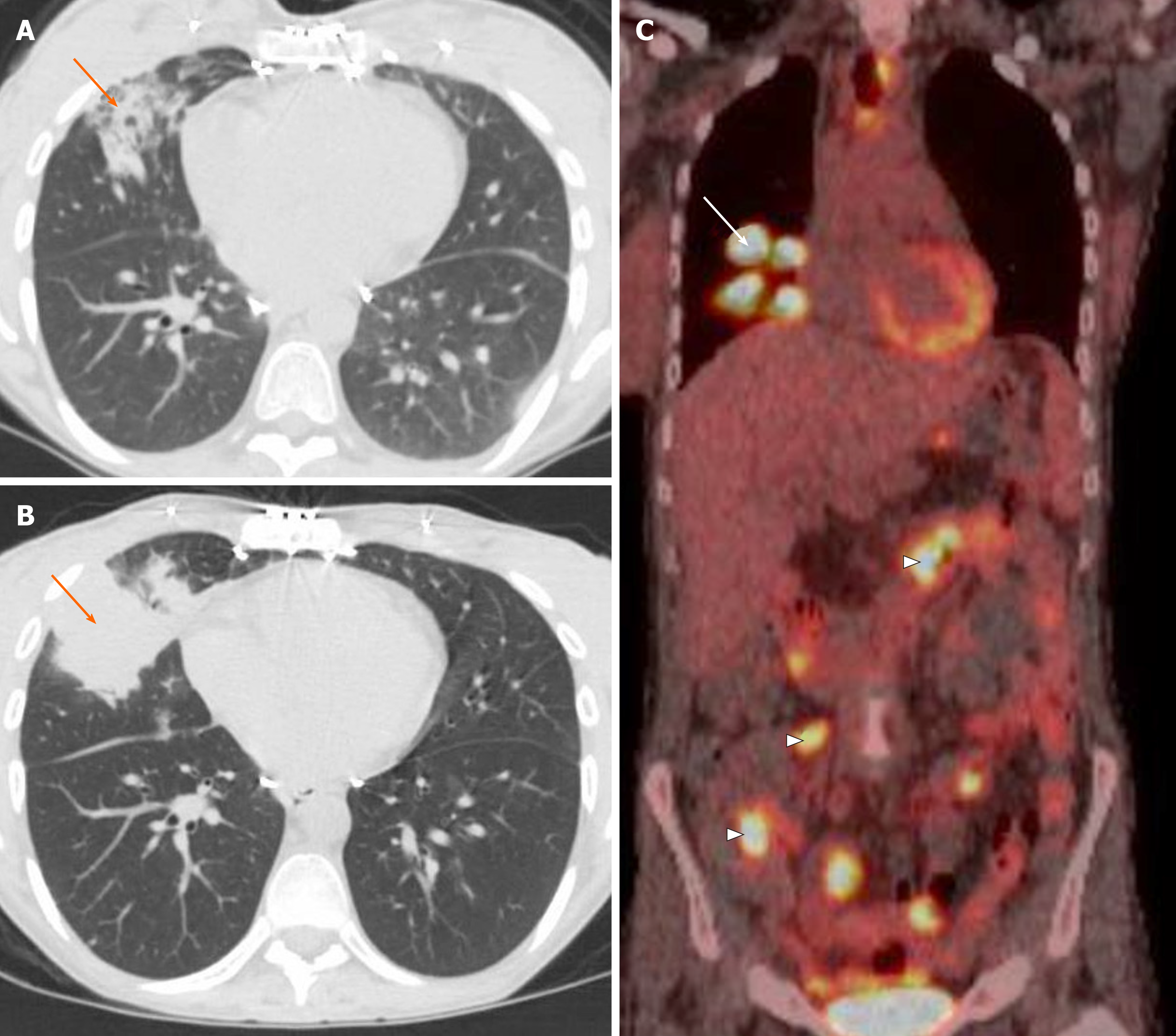
Figure 14 Post-transplant lymphoproliferative disease.
A: A 31-year-old woman with history of cystic fibrosis and double lung transplant presented with cough and computed tomography of the chest demonstrated consolidation in right middle lobe; B: Despite treatment, follow-up computed tomography after 2 mo demonstrated worsening right middle lobe consolidation (arrow); C: Fluorodeoxyglucose-positron emission tomography confirmed intense metabolic activity in the lung opacity (arrow) as well as areas of increased metabolic activity in the bowel (arrowheads). Biopsy confirmed the post-transplant lymphoproliferative disease.
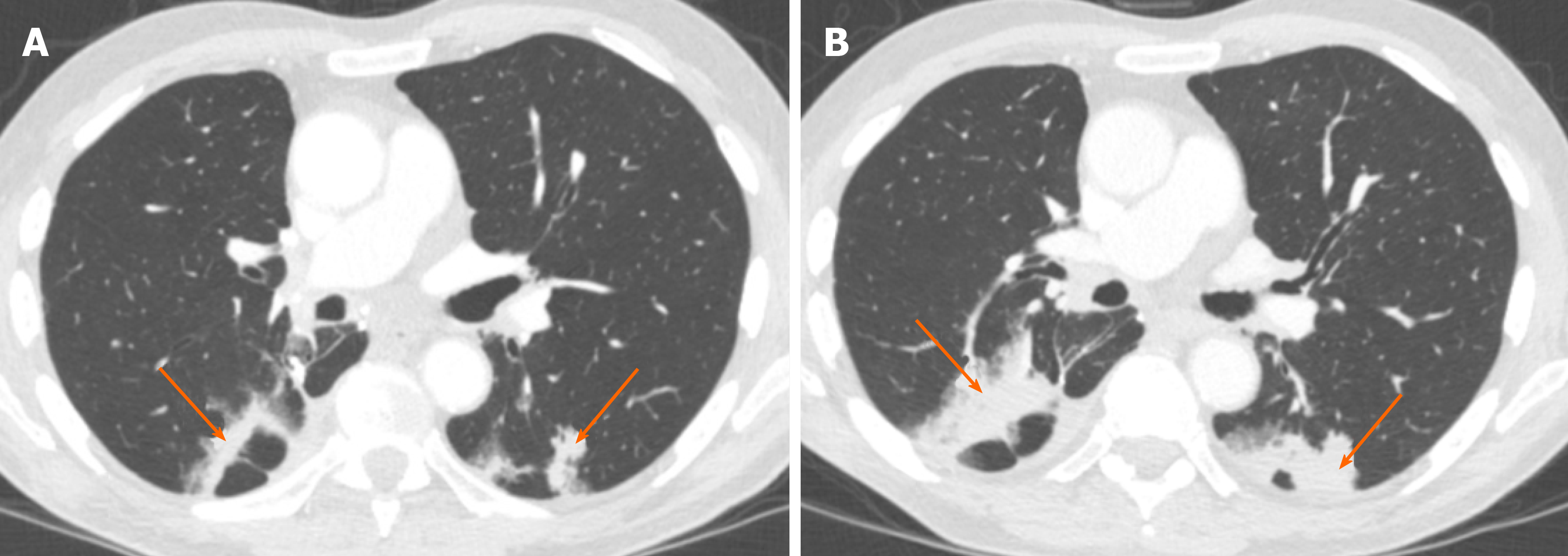
Figure 15 Metastatic adenocarcinoma of the pancreas.
A 54-year-old female presented with increasing shortness of breath. A and B: Contrast-enhanced computed tomography of the chest in lung window showed multiple areas of patchy and confluent airspace opacity, more in both lower lobes (A, arrows), and with no significant change at 3 mo follow-up (B, arrows).
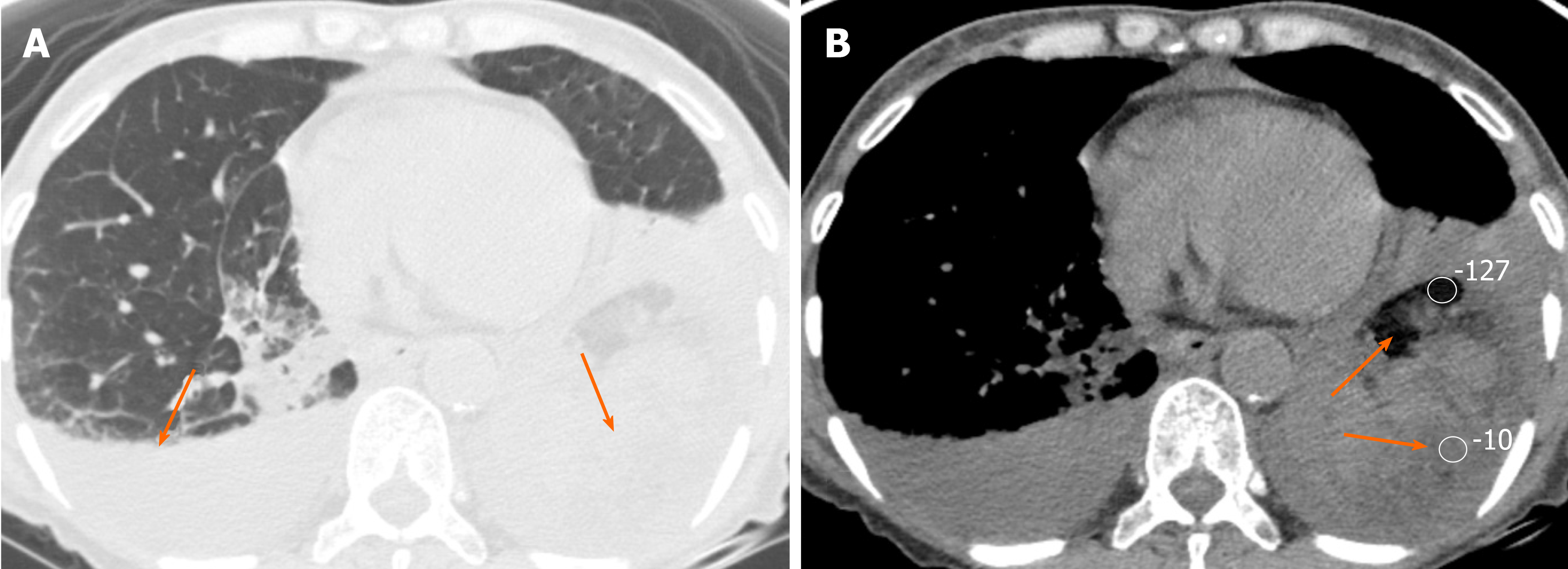
Figure 16 Lipoid pneumonia.
A 68-year-old female presented with long-standing chronic constipation and shortness of breath. A: Chest computed tomography in lung window showed areas of consolidation in both lungs (arrows); B: Some areas of consolidation showed fat density (HU of -127 and -10) (arrows), confirming the diagnosis of lipoid pneumonia. There was also bilateral pleural effusion.
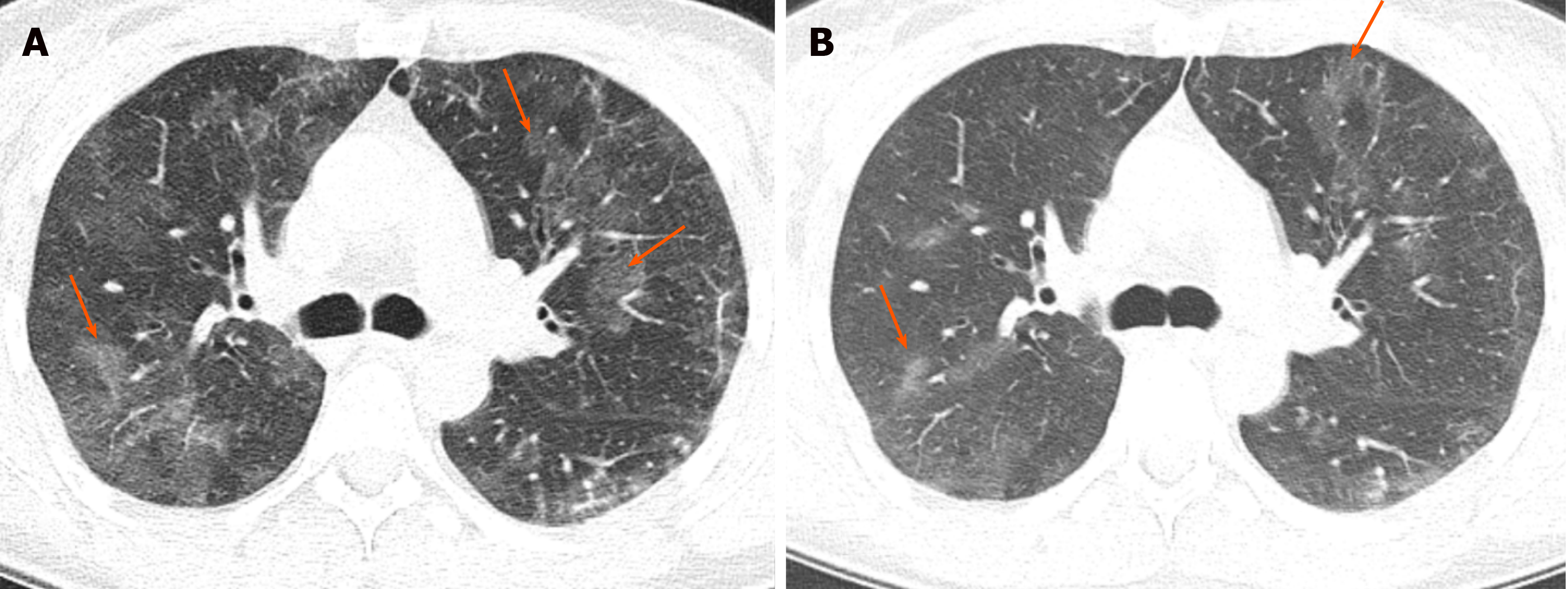
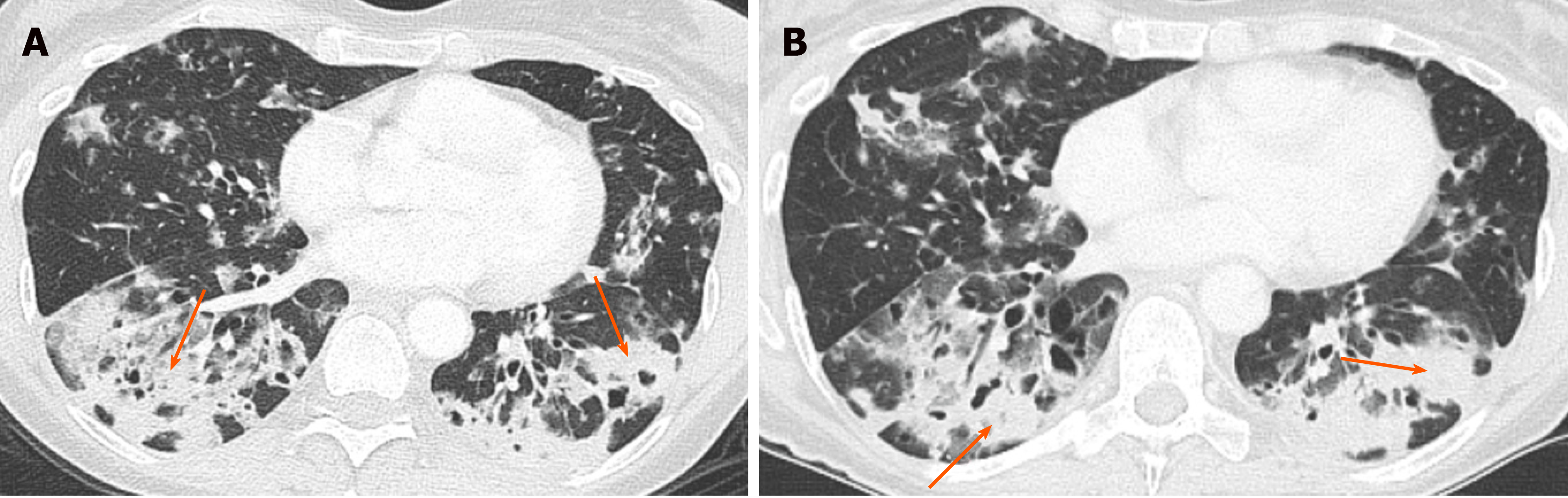
Figure 17 Pulmonary hemorrhage.
A 48-year-old woman with antiphospholipid antibody syndrome presented with shortness of breath. A: Computed tomography showed patchy, predominantly ground glass opacities in both lungs, with areas of subpleural sparing (arrows) that were confirmed to be due to alveolar hemorrhage; B: At 6 mo later, the patient presented with worsening dyspnea and hemoptysis and computed tomography demonstrated significant interval worsening of ground glass opacities with new involvement of a majority of the lung parenchyma.
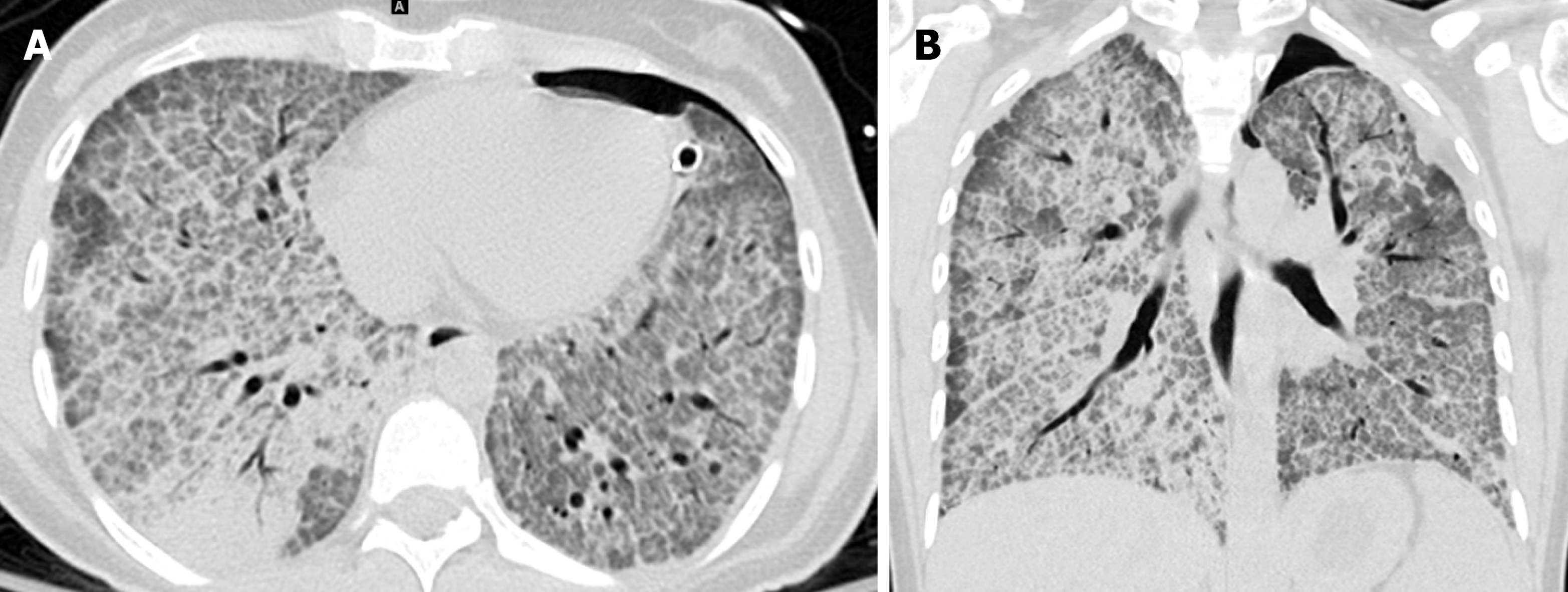
Figure 18 Pulmonary alveolar proteinosis.
A 35-year-old man who was an active smoker presented with shortness of breath and cough. A and B: Axial (A) and coronal (B) computed tomography of the chest showed smooth thickening of the interlobular and intralobular septal lines, and ground glass opacities, causing crazy paving pattern. Bronchoalveolar lavage confirmed the pulmonary alveolar proteinosis. The patient also had left-sided pneumothorax, with a chest tube in place. Courtesy of Lila Pourzand, MD.
- Citation: Ansari-Gilani K, Chalian H, Rassouli N, Bedayat A, Kalisz K. Chronic airspace disease: Review of the causes and key computed tomography findings. World J Radiol 2020; 12(4): 29-47
- URL: https://www.wjgnet.com/1949-8470/full/v12/i4/29.htm
- DOI: https://dx.doi.org/10.4329/wjr.v12.i4.29