Copyright
©The Author(s) 2018.
World J Radiol. Nov 28, 2018; 10(11): 172-183
Published online Nov 28, 2018. doi: 10.4329/wjr.v10.i11.172
Published online Nov 28, 2018. doi: 10.4329/wjr.v10.i11.172
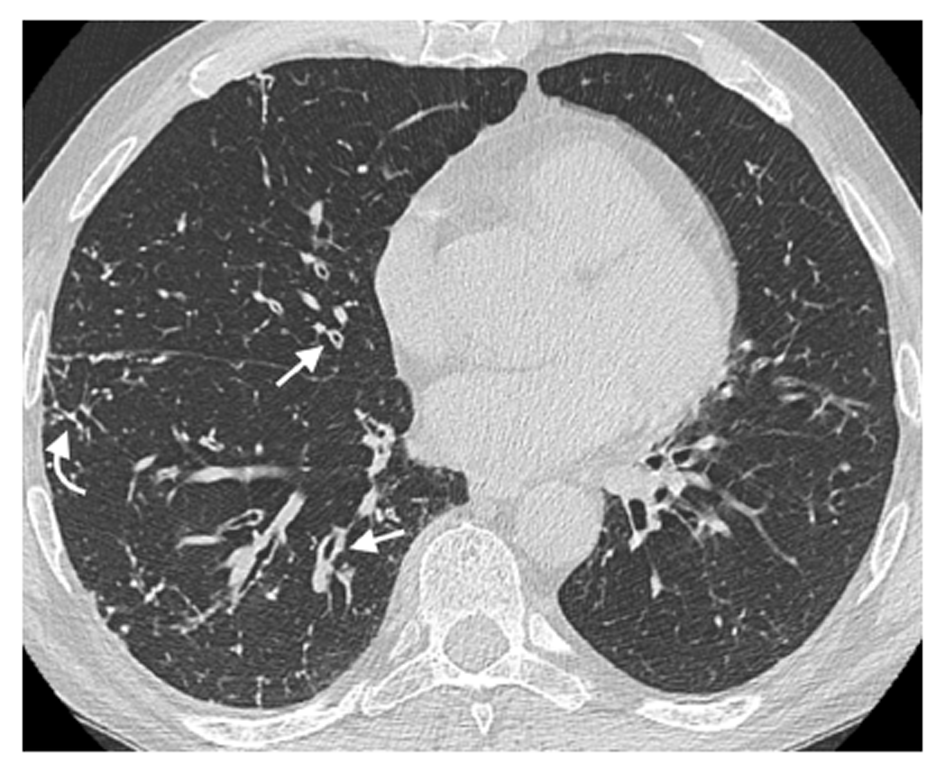
Figure 1 Airway wall thickening.
A 65-year-old male patient with common variable immunodeficiency disorder. High-resolution computed tomography shows diffuse airway wall thickening in the right middle and lower lobes (straight arrows); centrilobular and tree-in-bud nodules in the right lung are also detected (curved arrow).
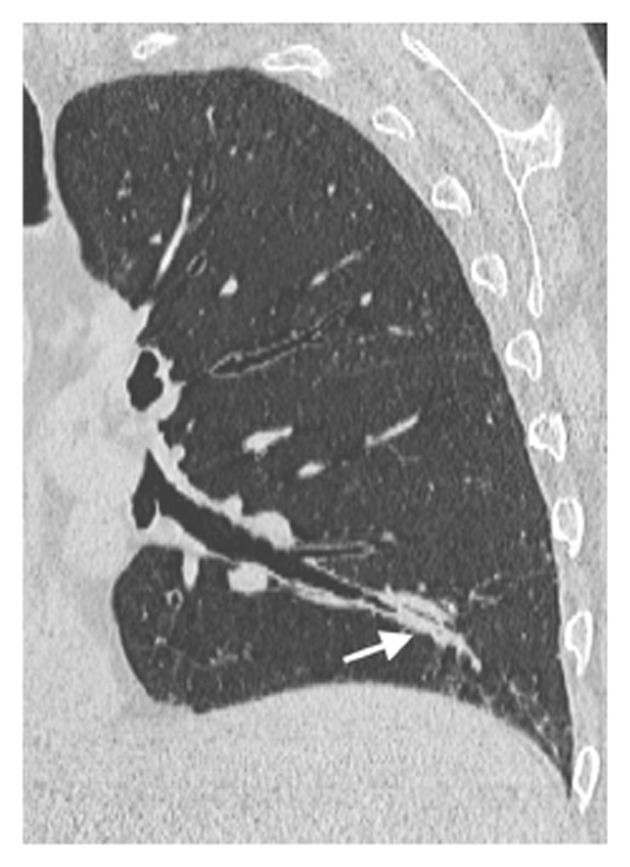
Figure 2 Nodules.
A 64-year-old female patient with common variable immunodeficiency disorder. High-resolution computed tomography shows multiple, small nodules with peribronchial and perifissural location in the upper and lower lobes of both lungs (arrows). A diagnosis of granulomatous and lymphocytic interstitial lung disease was subsequently made.
Figure 3 Mucus plugging.
A 65-year-old male patient with common variable immunodeficiency disorder. Para-coronal 2-mm minimum intensity projection high-resolution computed tomography image shows mild bronchiectasis with extensive mucus plugging in the left lower lobe (arrow).
Figure 4 Tree-in-bud.
A 40-year-old female patient with isolated IgG2 subclass deficiency. High-resolution computed tomography shows centrilobular and tree-in-bud nodules in the right upper lobe (straight arrows); small mucus plugging in the left lower lobe is also detected (curved arrow).
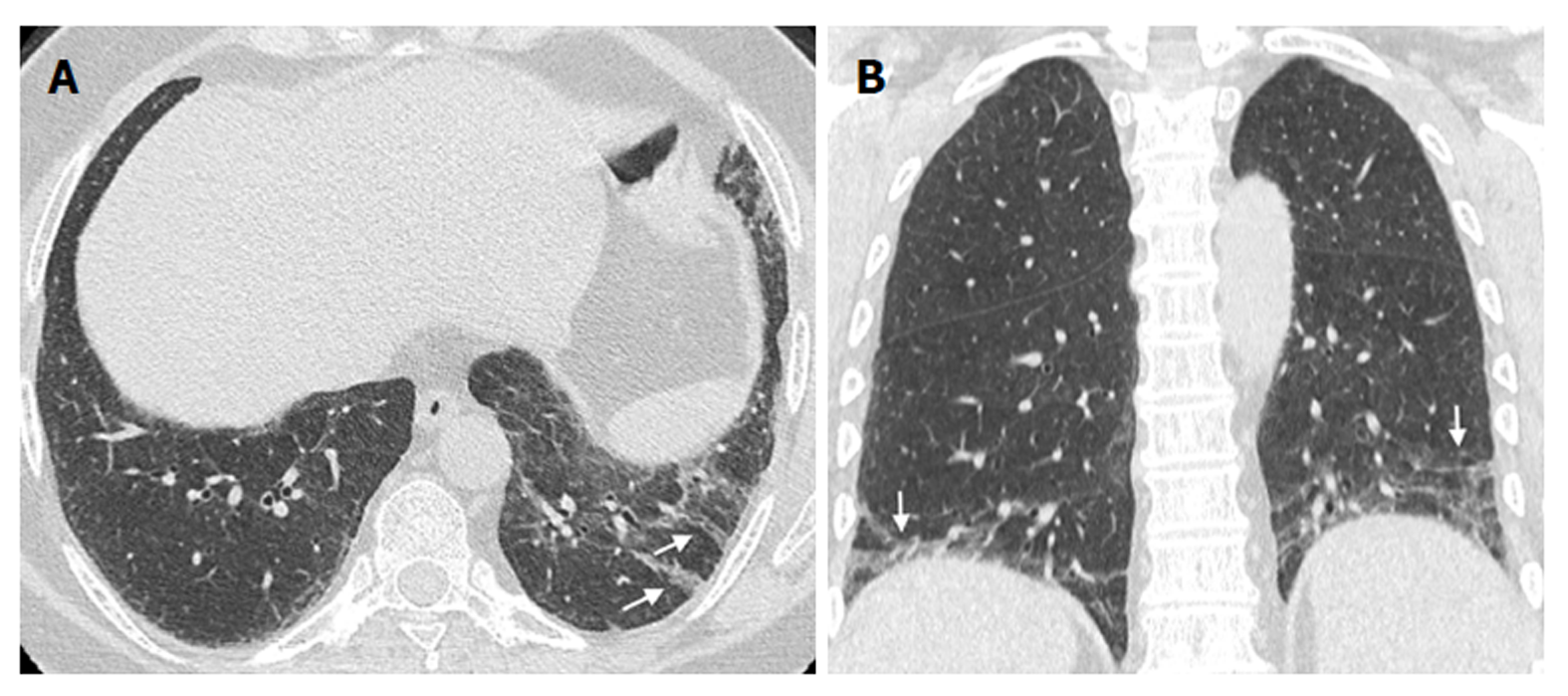
Figure 5 Linear and/or irregular opacities.
A 66-year-old female patient with common variable immunodeficiency disorder. A: High-resolution computed tomography shows patchy areas of ground-glass opacity, along with reticulation and linear and/or irregular opacities (arrows) in both lower lobes; B: Coronal reformatted image shows the peripheral and basal-predominant distribution of the findings (arrows).
- Citation: Cereser L, De Carli M, d’Angelo P, Zanelli E, Zuiani C, Girometti R. High-resolution computed tomography findings in humoral primary immunodeficiencies and correlation with pulmonary function tests. World J Radiol 2018; 10(11): 172-183
- URL: https://www.wjgnet.com/1949-8470/full/v10/i11/172.htm
- DOI: https://dx.doi.org/10.4329/wjr.v10.i11.172