Published online Sep 26, 2017. doi: 10.4330/wjc.v9.i9.757
Peer-review started: February 14, 2017
First decision: April 19, 2017
Revised: July 8, 2017
Accepted: July 21, 2017
Article in press: July 24, 2017
Published online: September 26, 2017
Processing time: 222 Days and 19.1 Hours
To apply real time three-dimensional transesophageal echocardiography (RT3D TEE) for quantitative and qualitative assessment of the mitral valve annulus (MVA) and tricuspid valve annulus (TVA) in the same patient.
Our retrospective cohort study examined the MVA and TVA in 49 patients by RT3D TEE. MVA and TVA shape were examined by TEE. The MVA and TVA volume data set images were acquired in the mid esophageal 4-chamber view. The MVA and TVA were acquired separately, with optimization of each for the highest frame rate and image quality. The 3D shape of the annuli was reconstructed using the Philips® Q lab, MVQ ver. 6.0 MVA model software. The end-systolic frame was used. The parameters measured and compared were annular area, circumference, high-low distances (height), anterolateral-posterolateral (ALPM), and anteroposterior (AP) axes.
A total of 49 patients (mean age 61 ± 14 years, 45% males) were studied. The ALPM and the AP axes of the MVA and TVA are not significantly different. The ALPM axis of the MVA was 37.9 ± 6.4 mm and 38.0 ± 5.6 mm for the TVA (P = 0.70). The AP axis of the MVA was 34.8 ± 5.7 mm and 34.9 ± 6.2 mm for the TVA (P = 0.90). The MVA and the TVA had similar circumference and area. The circumference of the MVA was 127.9 ± 16.8 mm and 125.92 ± 16.12 mm for the TVA (P = 0.23). The area of the MVA was 1103.7 ± 307.8 mm2 and 1131.7 ± 302.0 mm2 for the TVA (P = 0.41). The MVA and TVA are similar oval structures, but with significantly different heights. The ALPM/AP ratio for the MVA was 1.08 ± 0.33 and 1.09 ± 0.28 for the TVA (P < 0.001). The height for the MVA and TVA was 9.23 ± 2.11 mm and 4.37 ± 1.48 mm, respectively (P < 0.0001).
RT3D TEE plays an unprecedented role in the management of valvular heart disease. The specific and exclusive shape of the MVA and TVA was revealed in our study of patients studied. Moreover, the intricate codependence of the MVA and the TVA depends on their distinctive shapes. This realization seen from our study will allow us to better understand the role valvular disease plays in disease states such as hypertrophic cardiomyopathy and pulmonary hypertension.
Core tip: Three dimensional (3D) imaging of the heart has allowed for improved understanding and delineation of cardiac structure and function. Real time three-dimensional transesophageal echocardiography (RT3D TEE) has been on the forefront of allowing this 3D imaging to be used in mainstream cardiac practice for many years. The mitral valve annulus (MVA) and the tricuspid valve annulus (TVA) are multi-component complex structures and 3D imaging has allowed better understanding of their structure. Our study aims to apply RT3D TEE for quantitative and qualitative assessment and comparison of the MVA and TVA in the same patient. Gaining an understanding of the similarities and differences between these two valves will provide a better understanding of cardiac physiology and pathophysiology and thereby hopefully lead to improvements in clinical practice.
- Citation: Makaryus AN, Ismail H, Makaryus JN, Fan D. Geometric comparison of the mitral and tricuspid valve annulus: Insights from three dimensional transesophageal echocardiography. World J Cardiol 2017; 9(9): 757-760
- URL: https://www.wjgnet.com/1949-8462/full/v9/i9/757.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i9.757
The mitral valve annulus (MVA) and the tricuspid valve annulus (TVA) are multi-component complex structures[1]. The anatomy and geometry of the MVA has been previously described in many studies that utilized advanced imaging techniques[2-5]. This allowed for a better comprehension of valve dysfunction and provided significant implications for surgical repair[5]. Similarly, the geometry of the TVA has been previously assessed in numerous studies utilizing real time three-dimensional transesophageal echocardiography (RT3D TEE) to allow for complete visualization of the cusps of this complex structure[1]. Furthermore, RT3D TEE can visualize atrio-ventricular valves from both the atrial and ventricular side in great detail[1]. Measurements of the MVA and TVA, both researched and documented in the literature, have not been routinely measured and compared in the same person. This study aimed to apply RT3D TEE for quantitative and qualitative assessment and comparison of the MVA and TVA in the same patients. Gaining an understanding of the similarities and differences between these two valves will likely provide a better understanding of cardiac physiology and pathophysiology and lead to improvements in clinical practice.
In this retrospective cohort study, the MVA and TVA were examined in forty-nine patients by RT3D TEE after institutional review board approval was obtained. The study population included all patients that were referred to the North Shore University Hospital Echocardiography lab for standard TEE during a three month period. The TEE performing physician was capable of performing RT3D TEE. All patients had sinus rhythm, no prosthetic rings, no mechanical/bioprosthetic valves, no > 2+ MR or > 2+ TR, no more than moderate MS/AS, no more than moderate chamber dilation, and no regional wall abnormalities. Only patients with optimal studies were included.
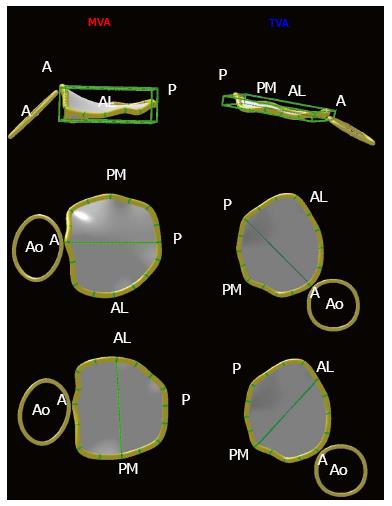
MVA and TVA shape were examined by TEE. The MVA and TVA volume data set images were acquired in the mid esophageal 4-chamber view. The MVA and TVA were acquired separately, with optimization of each for the highest frame rate and image quality. The MVA and TVA were never acquired in the same image because the frame rate was too low. The 3D shape of the annuli was reconstructed using the MVA model software (Figure 1, Philips® Q lab, MVQ ver. 6.0). The end-systolic frame was used. The parameters measured and compared were annular area, circumference, high-low distances (height), anterolateral-posterolateral (ALPM), and anteroposterior (AP) axes.
A total of 49 patients (mean age 61 ± 14 years, 45% males) were studied. Among the 49 patients 59% had hypertension, 18% had diabetes mellitus, 31% had coronary artery disease, and 57% had dyslipidemia. Furthermore, 51% were on a beta blocker, 24% were on a calcium channel blocker, 39% were on an angiotensin converting enzyme inhibitor or angiotensin receptor blocker, and 57% were on a statin. The ALPM and the AP axes of the MVA and TVA are not significantly different. The ALPM axis of the MVA was 37.9 ± 6.4 mm and 38.0 ± 5.6 mm for the TVA (P = 0.70). The AP axis of the MVA was 34.8 ± 5.7 mm and 34.9 ± 6.2 mm for the TVA (P = 0.90). Similarly, the MVA and the TVA had similar circumference and area. The circumference of the MVA was 127.9 ± 16.8 mm and 125.92 ± 16.12 mm for the TVA (P = 0.23). The area of the MVA was 1103.7 ± 307.8 mm2 and 1131.7 ± 302.0 mm2 for the TVA (P = 0.41). The MVA and TVA are similar oval structures, but with significantly different heights. The ALPM/AP ratio for the MVA was 1.08 ± 0.33 and 1.09 ± 0.28 for the TVA (P < 0.001). The height for the MVA and TVA was 9.23 ± 2.11 mm and 4.37 ± 1.48 mm, respectively (P < 0.0001; Table 1).
| Dimension | MV (mean ± SD) | TV (mean ± SD) | P-value |
| Circumference | 127.9 ± 16.8 mm | 125.9 ± 16.1 mm | 0.23 |
| Area | 1103.7 ± 307.8 mm2 | 1131.7 ± 302.0 mm2 | 0.41 |
| Height | 9.23 ± 2.11 mm | 4.37 ± 1.48 mm | < 0.0001 |
| ALPM axis | 37.9 ± 6.4 mm | 38.0 ± 5.6 mm | 0.7 |
| AP axis | 34.8 ± 5.7 mm | 34.9 ± 6.2 mm | 0.9 |
| ALPM/AP ratio | 1.08 ± 0.33 | 1.09 ± 0.28 | < 0.0001 |
Two-dimensional echocardiography (2DE) has been utilized in previous studies and proved to be a valuable imaging modality for the functional assessment of the MVA and TVA[3-7]. However, 2DE did not provide detailed anatomical information of the MVA or TVA. Previous case studies exploited the advanced imaging technique of RT3D TEE in visualizing the MVA and TVA in different patients[1]. This present study demonstrates that RT3D TEE allows for the comprehensive analysis and exact characterization of the anatomy of the MVA and TVA in the same patient.
One of the salient findings in our study was that, although the MVA and TVA had similar annular areas, circumference, ALPM axes, and AP axes, they both have a bimodal pattern with significantly different heights. The MVA is more elevated, circular and saddle shaped. This property allows for a secure anchoring of the leaflets that may minimize leaflet stress[8,9]. This unique shape of the MVA may also be due to the common location of the anterior mitral leaflet and the right coronary aortic leaflet which are united by a fibrous region. On the other hand, the posterior part of the MVA appears to be more flexible from the muscular fiber received from the proximal aspect of the posterior leaflet[8]. These unique assets contribute to the dynamic nature of the MVA for its proper functioning. RT3D TEE allows us to understand the anatomy which is necessary for reconstructive surgery of the MVA in mitral valve (MV) disease. The aim is such to restore the normal MVA shape and dynamics to enhance repair durability.
The MVA has more of an elliptical-saddle shape that is planar and ovoid. The shape of the TVA stems from its bicuspid embryology[9,10]. The TVA has two high points and two low points oriented to the right atrium and the right ventricular apex, respectively. The elliptical shape contributes to the competency of the tricuspid valve (TV) throughout the cardiac cycle. The preservation of the unique shape of the TVA also depends on the normal and unique shape of the MVA during the cardiac cycle. RT3D TEE demonstrates that anatomically the TVA and MVA form a figure eight across the ventricular septum. The shape of the TVA is requisite during ventricular systole when the high pressure of the left ventricle bends the interventricular septum and mitral annulus towards the right ventricle. RT3D TEE allows for better dynamic imaging to help in surgical planning in TV stenosis and regurgitation[8-10].
RT3D TEE plays an unprecedented role in the management of valvular heart disease. It allows for superior characterization of specific components of the valvular apparatus. Several studies have utilized RT3D TEE to evaluate the MVA and TVA in different patients. The aim of this study was to evaluate the native MVA and TVA using RT3D TEE in the same patients. The specific and exclusive shape of the MVA and TVA was revealed in the patients studied. Moreover, the intricate codependence of the MVA and the TVA depends on their distinctive shapes. This realization seen from our study will allow us to better understand the role valvular disease plays in disease states such as hypertrophic cardiomyopathy and pulmonary hypertension.
Three dimensional (3D) imaging of the heart has allowed for improved understanding and delineation of cardiac structure and function. Real time three-dimensional transesophageal echocardiography (RT3D TEE) has been on the forefront of allowing this 3D imaging to be used in mainstream cardiac practice for many years. The mitral valve annulus (MVA) and the tricuspid valve annulus (TVA) are multi-component complex structures and 3D imaging has allowed better understanding of their structure.
Measurements of the MVA and TVA, both researched and documented in the literature, have not been routinely measured and compared in the same person.
The study aims to apply RT3D TEE for quantitative and qualitative assessment and comparison of the MVA and TVA in the same patient. Measurements in the same patient with comparison of the MVA and TVA have not been routinely performed and documented. The authors used an innovative comparison of these two valve areas in the same patient.
Gaining an understanding of the similarities and differences between these two valves will provide a better understanding of cardiac physiology and pathophysiology and thereby hopefully lead to improvements in clinical practice.
MVA: This is the fibrous ring that comprises the structural skeleton of the two mitral valve leaflets. The mitral annulus is generally saddle-shaped and its shape is dynamic throughout the cardiac cycle; TVA: This is the fibrous ring that comprises the structural skeleton of the three tricuspid valve leaflets. The tricuspid annulus is generally saddle-shaped and its shape is dynamic throughout the cardiac cycle; RT3D TEE: Three-dimensional visual tool employing echocardiography to achieve a better understanding and assessment of normal and pathological cardiac function and anatomy and the spatial relationships of the structures identified.
This is an interesting manuscript.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kettering K, Okumura K S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Mor-Avi V, Sugeng L, Lang RM. Three-dimensional adult echocardiography: where the hidden dimension helps. Curr Cardiol Rep. 2008;10:218-225. [PubMed] |
| 2. | Silbiger JJ, Bazaz R. Contemporary insights into the functional anatomy of the mitral valve. Am Heart J. 2009;158:887-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Jungwirth B, Mackensen GB. Real-time 3-dimensional echocardiography in the operating room. Semin Cardiothorac Vasc Anesth. 2008;12:248-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Badano LP, Agricola E, Perez de Isla L, Gianfagna P, Zamorano JL. Evaluation of the tricuspid valve morphology and function by transthoracic real-time three-dimensional echocardiography. Eur J Echocardiogr. 2009;10:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Valocik G, Kamp O, Visser CA. Three-dimensional echocardiography in mitral valve disease. Eur J Echocardiogr. 2005;6:443-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Anwar AM, Soliman OI, Nemes A, van Geuns RJ, Geleijnse ML, Ten Cate FJ. Value of assessment of tricuspid annulus: real-time three-dimensional echocardiography and magnetic resonance imaging. Int J Cardiovasc Imaging. 2007;23:701-705. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Dreyfus J, Durand-Viel G, Raffoul R, Alkhoder S, Hvass U, Radu C, Al-Attar N, Ghodbhane W, Attias D, Nataf P. Comparison of 2-Dimensional, 3-Dimensional, and Surgical Measurements of the Tricuspid Annulus Size: Clinical Implications. Circ Cardiovasc Imaging. 2015;8:e003241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Ring L, Rana BS, Kydd A, Boyd J, Parker K, Rusk RA. Dynamics of the tricuspid valve annulus in normal and dilated right hearts: a three-dimensional transoesophageal echocardiography study. Eur Heart J Cardiovasc Imaging. 2012;13:756-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Kwan J, Kim GC, Jeon MJ, Kim DH, Shiota T, Thomas JD, Park KS, Lee WH. 3D geometry of a normal tricuspid annulus during systole: a comparison study with the mitral annulus using real-time 3D echocardiography. Eur J Echocardiogr. 2007;8:375-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Fukuda S, Saracino G, Matsumura Y, Daimon M, Tran H, Greenberg NL, Hozumi T, Yoshikawa J, Thomas JD, Shiota T. Three-dimensional geometry of the tricuspid annulus in healthy subjects and in patients with functional tricuspid regurgitation: a real-time, 3-dimensional echocardiographic study. Circulation. 2006;114:I492-I498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 194] [Article Influence: 10.2] [Reference Citation Analysis (0)] |