Published online Aug 26, 2017. doi: 10.4330/wjc.v9.i8.702
Peer-review started: November 10, 2016
First decision: February 17, 2017
Revised: March 15, 2017
Accepted: June 6, 2017
Article in press: June 8, 2017
Published online: August 26, 2017
Processing time: 286 Days and 23.4 Hours
To investigate the impact of coronary artery disease in a cohort of patients resuscitated from cardiac arrest with non-diagnostic electrocardiogram.
From March 2004 to February 2016, 203 consecutive patients resuscitated from in or out-of-hospital sudden cardiac arrest and non-diagnostic post-resuscitation electrocardiogram (defined as ST segment elevation or pre-sumably new left bundle branch block) who underwent invasive coronary angiogram during hospitalization were included. For purpose of analysis and comparison, patients were classified in two groups: Initial shockable rhythm (ventricular tachycardia or ventricular fibrillation; n = 148, 72.9%) and initial non-shockable rhythm (n = 55, 27.1%). Baseline characteristics, coronary angiogram findings including Syntax Score and long-term survival rates were compared.
Sudden cardiac arrest was witnessed in 95.2% of cases, 66.7% were out-of-hospital patients and 72.4% were male. There were no significant differences in baseline characteristics between groups except for higher mean age (68.1 years vs 61 years, P = 0.001) in the non-shockable rhythm group. Overall 5-year mortality of the resuscitated patients was 37.4%. Patients with non-shockable rhythms had higher mortality (60% vs 29.1%, P < 0.001) and a worst neurological status at hospital discharge based on cerebral performance category score (CPC 1-2: 32.7% vs 53.4%, P = 0.02). Although there were no significant differences in global burden of coronary artery disease defined by Syntax Score (mean Syntax Score: 10.2 vs 10.3, P = 0.96) there was a trend towards a higher incidence of acute coronary lesions in patients with shockable rhythm (29.7% vs 16.4%, P = 0.054). There was also a higher need for ad-hoc percutaneous coronary intervention in this group (21.9% vs 9.1%, P = 0.03).
Initial shockable group of patients had a trend towards higher incidence of acute coronary lesions and higher need of ad-hoc percutaneous intervention vs non-shockable group.
Core tip: Coronary artery disease represents the most common cause of sudden cardiac arrest. Current re-suscitation guidelines recommend emergency coronary angiography in patients with cardiac arrest and ST elevation or new left bundle branch block on post-resuscitation electrocardiogram. However, electrocardiogram findings may be a poor predictor of an acute coronary lesion in this context and nowadays, the benefit of early coronary angiography is still under debate in patients without ST elevation. In this study, we analyzed our single-center data of patients with cardiac arrest and non-diagnostic electrocardiogram to describe the burden of coronary artery disease and their prognosis depending on initial rhythm.
- Citation: Martínez-Losas P, Salinas P, Ferrera C, Nogales-Romo MT, Noriega F, Del Trigo M, Núñez-Gil IJ, Nombela-Franco L, Gonzalo N, Jiménez-Quevedo P, Escaned J, Fernández-Ortiz A, Macaya C, Viana-Tejedor A. Coronary angiography findings in cardiac arrest patients with non-diagnostic post-resuscitation electrocardiogram: A comparison of shockable and non-shockable initial rhythms. World J Cardiol 2017; 9(8): 702-709
- URL: https://www.wjgnet.com/1949-8462/full/v9/i8/702.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i8.702
Sudden cardiac arrest (SCA) is one of the most common causes of death in the developed world, affecting nearly 560000 people annually in the United States. Although a majority of deaths occur during the initial resuscitation, a substantial proportion of cardiac arrest deaths occur in patients who have been initially successfully resuscitated after first medial contact. Despite the important advances in emergency medical services and post cardiac arrest syndrome care over the last decades, survival free from neurological deficit is still low[1].
Coronary artery disease (CAD) represents the most common cause of SCA and current resuscitation guidelines recommend the performance of an emergency coronary angiography (CA) and appropriate percutaneous coronary interventions (PCI) in patients with SCA and ST segment elevation or presumably new left bundle branch block (LBBB) on post-resuscitation electrocardiogram (ECG). In patients without ST elevation after SCA but with suspected or with a high risk of cardiac origin, emergency CA is reasonable in selected situations (for example, electrically or hemodynamically unstable patients)[2,3]. Such “suspicion of cardiac origin” is not well defined and therefore the recommendation remains somewhat ambiguous.
Regarding the likelihood of a cardiac origin of the SCA, the ECG may be a poor predictor of acute coronary occlusion in resuscitated patients[4-7]. Also, a recent meta-analysis showed a high prevalence of significant CAD ranging from 59% to 71% in patients resuscitated from SCA without an obvious non-cardiac etiology[8]. Furthermore, pre-arrest symptoms reported in this setting are unreliable and dependent on the presence of by-standers. In summary, the suspicion of cardiac origin is largely subjective or uncertain for most patients. For these reasons, and without available randomized data, the justification for use of an early invasive strategy in survivors of SCA without an obvious non-cardiac cause of arrest is based on observational data[9-11].
From a single-center registry of patients resuscitated from SCA undergoing CA, we present in this paper the results of a sub-analysis comparing patients with shockable and non-shockable initial rhythms[12]. The aim of this sub-analysis was to investigate the impact of CAD in a cohort of SCA patients with non-diagnostic ECG depending on initial rhythm.
All patients recovered from in or out-of-hospital SCA and admitted to a tertiary care center with 24/7 emergent PCI availability that underwent invasive CA were extracted from a multipurpose database including data from interventional procedures, critical care unit and hospital admission.
From March 2004 to February 2016, 545 consecutive SCA patients were identified. For this study, we focused on patients without emergent indication for CA. Therefore, patients with ST segment elevation or presumably new LBBB on post-resuscitation ECG, or cardiogenic shock at admission were excluded (n = 317). Of the remaining 228 patients, 25 had unavailable or incomplete CA films. Thus, our final study population was 203 patients. For the purpose of this sub-analysis, patients were classified into two groups depending on initial ECG: Shockable [ventricular tachycardia or ventricular fibrillation (n = 148, 72.9%)] and non-shockable rhythm (n = 55, 27.1%) (Figure 1).
Clinical and outcome data were collected from clinical record, patient’s charts or telephone contact with patients or their relatives. Follow-up was completed up to 5-year after index admission.
The indication and timing of CA in our study population was individualized for each patient based on treating physician’s criterion. CA was classified as early when performed < 24 h after hospital admission or late when performed ≥ 24 h after admission. Two interventional cardiologist reviewed all CA blinded to original reports. The percentage diameter stenosis (DS%) was visually estimated for each lesion. Quantitative CA was used if discordances > 10% were found between both investigators. Significant stenosis was defined as ≥ 50 DS%, severe stenosis when DS% was ≥ 70% and non-obstructive CAD when DS% was < 50%. A normal coronary angiogram was defined as 0 DS% in all arteries with no other pathological findings. Culprit lesion was defined as the presence of an acute arterial occlusion (plaque rupture with occlusive thrombus) or an incomplete coronary artery occlusion in presence of complex lesion morphology as previously defined[13]. Chronic total occlusion (CTO) was defined as a Thrombolysis In Myocardial Infarction (TIMI) grade 0 flow for at least 3 mo of estimated duration. Estimation of occlusion duration was based on at least one of the following: Prior history of myocardial infarction in the target vessel territory, comparison with a previous angiogram, or the presence of collateral circulation or bridging collaterals. Critical stenosis was considered when DS% was ≥ 90% but < 100% and there were no CTO features. Acute coronary lesion was defined as critical or culprit lesion for the purpose of this investigation. Ad-hoc PCI was defined if performed at the moment of the index CA at the operator’s discretion. Procedural success was defined as complete restoration of antegrade blood flow (TIMI 3) and < 30% residual diameter stenosis by visual assessment.
Burden of CAD was measured using the Synergy Between Percutaneous Coronary Intervention With Taxus And Cardiac Surgery (SYNTAX) Score and number of vessels with significant and/or severe stenosis. We calculated the Syntax Score for each patient, as previously reported[14,15]. If the patient had previous PCI we used residual Syntax score (rSS) defined as the SYNTAX score remaining after PCI. If the patient had previous coronary artery bypass graft (CABG) surgery we calculated the CABG-SYNTAX score proposed by Farooq et al[16]. Both rSS and CABG-SYNTAX score reflect the current burden of CAD (successfully revascularized segments are equalized to segments with CAD < 50%, thus not incrementing SYNTAX score).
Statistical analysis was performed using SPSS 21 (SPSS Inc, Illinois, Chicago, United States). Continuous variables are presented as mean and standard deviation. Categorical variables are expressed as frequency and percentage. In quantitative variables, the groups were compared using a two-tailed Student’s t-test for independent samples. Categorical variables were compared with the χ2 test. The Kaplan-Meier method was used to estimate the cumulative patient survival rates and log-rank test for comparison. All test were two sided and P < 0.05 was considered significant.
Of 203 consecutive patients resuscitated from SCA with non-diagnostic ECG, 148 had initial shockable rhythm and 55 had non-shockable rhythm. Table 1 shows the baseline characteristics of the study cohort. There were no statistical differences between groups in baseline characteristics except for higher mean age in the initial non-shockable group (68.1 years vs 61 years, P = 0.001).
| All patients (n = 203) | Non-shockable rhythm (n = 55) | Shockable rhythm (n = 148) | P value | |
| Age (mean ± SD) | 62.9 ± 14 | 68.1 ± 13 | 61 ± 13.9 | 0.001 |
| Male sex | 147 (72.4) | 36 (65.5) | 111 (75) | 0.176 |
| Arterial hypertension | 123 (60.6) | 37 (67.3) | 86 (58.1) | 0.235 |
| Diabetes mellitus | 65 (32) | 22 (40) | 43 (29.1) | 0.137 |
| Dyslipidemia | 80 (39.4) | 26 (47.3) | 54 (36.5) | 0.162 |
| Smoking | 103 (50.7) | 27 (49.1) | 76 (51.4) | 0.775 |
| Peripheral vascular disease | 23 (11.3) | 7 (12.7) | 16 (10.8) | 0.702 |
| Cerebrovascular vascular disease | 18 (8.9) | 6 (10.9) | 12 (8.1) | 0.533 |
| Prior MI | 45 (22.2) | 14 (25.5) | 31 (20.9) | 0.780 |
| Prior PCI | 35 (17.2) | 10 (18.2) | 25 (16.9) | 0.829 |
| Prior CABG | 22 (10.8) | 7 (12.7) | 15 (10.1) | 0.597 |
| Out-of-hospital SCA | 124 (66.7) | 30 (58.8) | 94 (69.6) | 0.163 |
| Time to ROSC | 17.8 ± 12.7 | 14.8 ± 11.9 | 19 ± 12.9 | 0.122 |
| Witnessed arrest | 157 (95.2) | 40 (93) | 117 (95.9) | 0.450 |
| Coma status at admission | 148 (84.6) | 40 (88.9) | 108 (83.1) | 0.352 |
| Cardiogenic shock | 48 (23.6) | 18 (32.7) | 30 (20.3) | 0.063 |
| Therapeutic hypothermia | 71 (41.8) | 14 (32.6) | 57 (44.9) | 0.402 |
Early CA was performed in 115 patients (56.9%). The most relevant angiography findings are reproduced in Table 2. Overall, mean value of Syntax Score calculated was 10.30 with no statistical differences between groups (10.33 vs 10.23, P = 0.95). There were also no differences (P = 0.71) in the percentage of vessels with significant stenosis (0, 1, 2 or 3 vessels with ≥ 50 DS%). However, patients with initial shockable rhythm showed a trend towards a higher incidence of acute coronary lesions (29.7% vs 16.4%, P = 0.054) and higher rate of ad-hoc PCI (21.9% vs 9.1%, P = 0.03), mainly for left anterior descending artery lesions (45.9%).
| All patients (n = 203) | Non-shockable rhythm (n = 55) | Shockable rhythm (n = 148) | P value | |
| Normal coronaries | 71 (35) | 20 (36.4) | 51 (34.5) | 0.800 |
| Mean Syntax Score | 10.3 ± 12.4 | 10.2 ± 13.6 | 10.3 ± 11.9 | 0.961 |
| Any vessel with significant stenosis (DS ≥ 50%) | 125 (61.6) | 33 (60) | 92 (62.2) | 0.778 |
| Significant stenosis | ||||
| None | 79 (38.9) | 22 (40) | 57 (38.5) | 0.710 |
| One vessel | 46 (22.7) | 15 (27.3) | 31 (20.9) | |
| Two vessels | 40 (19.7) | 9 (16.4) | 31 (20.9) | |
| Three vessels | 38 (18.7) | 9 (16.4) | 29 (19.6) | |
| Any vessel with severe stenosis (DS ≥ 70%) | 111 (54.7) | 28 (50.9) | 83 (56.1) | 0.480 |
| Any CTO | 60 (29.6) | 14 (25.5) | 46 (31.1) | 0.388 |
| Critical stenosis | 51 (25.1) | 9 (16.4) | 42 (28.4) | 0.079 |
| Culprit lesion | 25 (12.3) | 4 (7.3) | 21 (14.2) | 0.173 |
| Acute lesion | 53 (26.1) | 9 (16.4) | 44 (29.7) | 0.054 |
| Ad hoc PCI | 37 (18.2) | 5 (9.1) | 32 (21.6) | 0.036 |
The prognostic value of acute coronary lesions as defined by this study was assessed through a stratified Kaplan Meier analysis. Figure 2 shows Kaplan Meier curves for all cause 5-year survival depending on the finding of an acute coronary lesion. Patients with shockable rhythm and with acute coronary lesions had a non-significant increased mortality, whereas no significant differences or trends were found in the non-shockable group. Interestingly, in patients with shockable rhythm, those who underwent ad hoc PCI of the acute coronary lesions had a trend towards improved survival compared to patients with untreated acute coronary lesions (mean all-cause survival 41.3 ± 5.4 mo vs 29.7 ± 6.9 mo, P = 0.147). However, in patients with initial non-shockable rhythm, ad hoc PCI did not improve survival rates (P = 0.948).
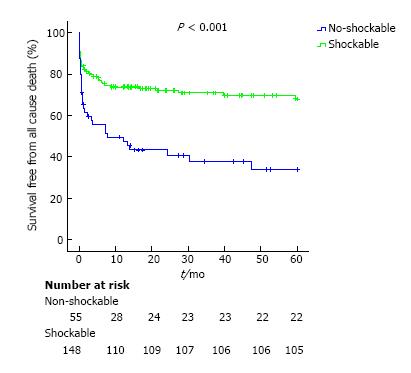
Overall, 151 (74.4%) patients survived until hospital discharge and 97 (64.2%) survived with a favorable neurological outcome based on cerebral performance category score (CPC). Patients with initial shockable rhythm had a better prognosis, with higher survival rates to discharge compared with those with non-shockable rhythm (56.4% vs 81.1%, P < 0.001). Patients with shockable rhythm also had a better neurological status at discharge (CPC 1-2: 32.7% vs 53.4%, P = 0.02). Five-years mortality was 37.4% in the global cohort. Patients with non-shockable rhythm had a higher five-year mortality (60% vs 29.1%, P < 0.001, Figure 3).
This study is a sub-analysis of a large single-center registry of selected SCA patients with CA and non-diagnostic post resuscitation ECG[12]. The present study compares shockable vs non-shockable rhythms and reveals a similar high burden of CAD in both groups. Although these findings are consistent with previous observational studies[8], our study is novel because it is the first to explore differences between shockable and non- shockable rhythms in this setting. Since the publication in 1997 of a seminal study by Spaulding et al[17], many studies with important methodological limitations have reported the possible survival impact of an early invasive approach in this context[9,18-21]. However, other studies did not find any benefit from such an invasive strategy and proposed to restrict it use to highly selected patients[10,11,22]. Besides, in contrast to the usual presentation of acute coronary syndromes, the standard tools to evaluate coronary ischemia in post cardiac arrest patients are less accurate. The sensitivity and specificity of the usual clinical data, ECG or biomarkers to predict an acute coronary artery occlusion are unclear[4-6,23]. For these reasons, there is still an ongoing debate on the use of an early invasive strategy in all survivors of SCA without an obvious non-cardiac cause. We conducted this sub-analysis in order to assess if the initial rhythm after resuscitation could be a predictor of CAD burden and acute coronary lesions.
Given the high probability of CAD (measured as mean Syntax Score), our data supports a low threshold for CA regardless of initial rhythm. According to current resuscitation guidelines, it is reasonable to discuss and consider emergent cardiac catheterization in patients with a high risk of a coronary cause for their cardiac arrest[3]. However, definitive data will come with the results of several ongoing randomized trials designed to determine whether early CA improves outcomes in out-of-hospital cardiac arrest, in patients without ST elevation [one of those (COUPE trial) conducted by our group][24-27].
Some differences in acute coronary lesions were found between the two groups. Those patients with initial shockable rhythm had a higher incidence of acute coronary lesions (29.7% vs 16.4%, P = 0.054) and consequently a greater requirement of ad-hoc PCI (21.9% vs 9.1%, P = 0.03). These acute coronary lesions might also have a potential impact on prognosis (Figure 2). Unfortunately, our study was underpowered to show the effect of revascularization on these lesions, but this should be considered a relevant research target for future studies. These findings are in accordance with the observed trend that reveals that CA and PCI after ventricular tachycardia or ventricular fibrillation has substantially increased over the last years, regardless of the presence of ST elevation[28].
Regarding the prognosis of initial ECG rhythm analysis, SCA patients are usually divided into non-shockable rhythms (pulseless electrical activity and asystole) or shockable rhythms (ventricular tachycardia and ventricular fibrillation). Non-shockable rhythms are the most prevalent first recorder rhythm and survival rates of this group are worst compared with initial shockable rhythm[1]. Studies have shown that increased age, female gender, and prolonged ROSC are associated with a non-shockable rhythm while public location and witnessed arrest are associated with a shockable rhythm[29]. In our study, survival rates were also higher in patients with initial shockable rhythms (60% vs 29.1%, P < 0.001), as previously reported[1]. However, there were no statistical differences in baseline characteristic except for higher mean age (68.1 years vs 61 years, P = 0.001) in the non-shockable rhythm group, probably due to the study design and patients selection.
The present study should be interpreted within the context of several limitations of a single-center observational study and relatively small size of the study population. The cohort included in this study was selected from consecutive patients who survived to in or out-of-hospital SCA and were subsequently selected for CA by clinicians upon admission. Patients with an explicit non-cardiac etiology of SCA would not be selected for CA and the final decision to proceed with CA was based on the clinical judgment of individual physicians. It is likely that CA was selectively more frequently offered to patients with a better likelihood of neurological recovery.
In conclusion, in our cohort of patients with SCA and non-diagnostic ECG, initial shockable rhythm group of patients had a similar burden of CAD compared to those with non-shockable rhythms. Patients with initial shockable rhythm had a trend towards a higher incidence of acute coronary lesions and a higher need of ad-hoc percutaneous coronary intervention. A low threshold for early CA should be considered in this subgroup of resuscitated SCA patients.
The authors thank Philip J Brabyn for English editing services.
Acute coronary syndromes are a common cause of sudden cardiac arrest (SCA). Based on observational studies, current resuscitation guidelines recommend emergency coronary angiography (CA) in patients with SCA and ST segment elevation on post-resuscitation electrocardiogram (Class I, level B). However, because of fewer data available, in patients without ST segment elevation, emergency CA is reasonable in selected patients with suspected cardiac origin (Class II a, level C), regardless of initial rhythm.
Electrocardiogram findings may be a poor predictor of an acute coronary lesion in patients after a SCA. Without randomized data, the benefit of early CA in patients without ST elevation remains controversial.
In patients with SCA and non-diagnostic post-resuscitation electrocardiogram, initial shockable rhythms show a trend towards a higher incidence of acute coronary lesions and higher need of ad-hoc percutaneous coronary intervention.
The results of the study suggest that a low threshold for early CA should be considered in this subgroup of resuscitated SCA patients.
Shockable rhythms include ventricular tachycardia and ventricular fibrillation in opposition to non-shockable rhythm that include asystole and pulseless electrical activity.
The manuscript is well-written, the statistical analysis is appropriate, and the data support the conclusions. This work will be of interest to the readership, and is potentially impactful regarding acute treatment of initially resuscitated, hospitalized cardiac arrest patients.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: den Uil CA, Mallet RT, Vermeersch P S-Editor: Kong JX L-Editor: A E-Editor: Lu YJ
| 1. | Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2843] [Cited by in RCA: 3822] [Article Influence: 382.2] [Reference Citation Analysis (0)] |
| 2. | Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, Meurer WJ, Peberdy MA, Thompson TM. Part 8: Post-Cardiac Arrest Care: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S465-S482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 965] [Cited by in RCA: 1037] [Article Influence: 103.7] [Reference Citation Analysis (0)] |
| 3. | Nolan JP, Soar J, Cariou A, Cronberg T, Moulaert VR, Deakin CD, Bottiger BW, Friberg H, Sunde K, Sandroni C. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines for Post-resuscitation Care 2015: Section 5 of the European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. 2015;95:202-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 710] [Cited by in RCA: 763] [Article Influence: 84.8] [Reference Citation Analysis (0)] |
| 4. | Zanuttini D, Armellini I, Nucifora G, Grillo MT, Morocutti G, Carchietti E, Trillò G, Spedicato L, Bernardi G, Proclemer A. Predictive value of electrocardiogram in diagnosing acute coronary artery lesions among patients with out-of-hospital-cardiac-arrest. Resuscitation. 2013;84:1250-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 5. | Sideris G, Voicu S, Dillinger JG, Stratiev V, Logeart D, Broche C, Vivien B, Brun PY, Deye N, Capan D. Value of post-resuscitation electrocardiogram in the diagnosis of acute myocardial infarction in out-of-hospital cardiac arrest patients. Resuscitation. 2011;82:1148-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 6. | Müller D, Schnitzer L, Brandt J, Arntz HR. The accuracy of an out-of-hospital 12-lead ECG for the detection of ST-elevation myocardial infarction immediately after resuscitation. Ann Emerg Med. 2008;52:658-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Stær-Jensen H, Nakstad ER, Fossum E, Mangschau A, Eritsland J, Drægni T, Jacobsen D, Sunde K, Andersen GØ. Post-Resuscitation ECG for Selection of Patients for Immediate Coronary Angiography in Out-of-Hospital Cardiac Arrest. Circ Cardiovasc Interv. 2015;8:e002784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 59] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 8. | Larsen JM, Ravkilde J. Acute coronary angiography in patients resuscitated from out-of-hospital cardiac arrest--a systematic review and meta-analysis. Resuscitation. 2012;83:1427-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 129] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 9. | Hollenbeck RD, McPherson JA, Mooney MR, Unger BT, Patel NC, McMullan PW Jr, Hsu CH, Seder DB, Kern KB. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation. 2014;85:88-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 183] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 10. | Bro-Jeppesen J, Kjaergaard J, Wanscher M, Pedersen F, Holmvang L, Lippert FK, Møller JE, Køber L, Hassager C. Emergency coronary angiography in comatose cardiac arrest patients: do real-life experiences support the guidelines? Eur Heart J Acute Cardiovasc Care. 2012;1:291-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 116] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 11. | Dankiewicz J, Nielsen N, Annborn M, Cronberg T, Erlinge D, Gasche Y, Hassager C, Kjaergaard J, Pellis T, Friberg H. Survival in patients without acute ST elevation after cardiac arrest and association with early coronary angiography: a post hoc analysis from the TTM trial. Intensive Care Med. 2015;41:856-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 12. | Nogales-Romo MT, Martinez-Losas P, Salinas P, Ferrera C, Gonzalo N, Nombela L, Jiménez P, Núñez-Gil I, Escaned J, Viana-Tejedor A. SYNTAX score as a prognostic tool in non-STEMI patients resuscitated from sudden cardiac arrest. ESC congress; Rome, Italy; August 27-31. 2016;. |
| 13. | Kerensky RA, Wade M, Deedwania P, Boden WE, Pepine CJ; Veterans Affairs Non-Q-Wave Infarction Stategies in-Hospital (VANQWISH) Trial Investigators. Revisiting the culprit lesion in non-Q-wave myocardial infarction. Results from the VANQWISH trial angiographic core laboratory. J Am Coll Cardiol. 2002;39:1456-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 107] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, Van Dyck N, Russell ME, Mohr FW. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219-227. [PubMed] |
| 15. | Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50-56. [PubMed] |
| 16. | Farooq V, Girasis C, Magro M, Onuma Y, Morel MA, Heo JH, Garcia-Garcia H, Kappetein AP, van den Brand M, Holmes DR. The CABG SYNTAX Score - an angiographic tool to grade the complexity of coronary disease following coronary artery bypass graft surgery: from the SYNTAX Left Main Angiographic (SYNTAX-LE MANS) substudy. EuroIntervention. 2013;8:1277-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 17. | Spaulding CM, Joly LM, Rosenberg A, Monchi M, Weber SN, Dhainaut JF, Carli P. Immediate coronary angiography in survivors of out-of-hospital cardiac arrest. N Engl J Med. 1997;336:1629-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 733] [Cited by in RCA: 702] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 18. | Weiser C, Testori C, Sterz F, Schober A, Stöckl M, Stratil P, Wallmüller C, Hörburger D, Spiel A, Kürkciyan I. The effect of percutaneous coronary intervention in patients suffering from ST-segment elevation myocardial infarction complicated by out-of-hospital cardiac arrest on 30 days survival. Resuscitation. 2013;84:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Lettieri C, Savonitto S, De Servi S, Guagliumi G, Belli G, Repetto A, Piccaluga E, Politi A, Ettori F, Castiglioni B. Emergency percutaneous coronary intervention in patients with ST-elevation myocardial infarction complicated by out-of-hospital cardiac arrest: early and medium-term outcome. Am Heart J. 2009;157:569-575.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 20. | Geri G, Dumas F, Bougouin W, Varenne O, Daviaud F, Pène F, Lamhaut L, Chiche JD, Spaulding C, Mira JP. Immediate Percutaneous Coronary Intervention Is Associated With Improved Short- and Long-Term Survival After Out-of-Hospital Cardiac Arrest. Circ Cardiovasc Interv. 2015;8:e002303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 21. | Dumas F, Cariou A, Manzo-Silberman S, Grimaldi D, Vivien B, Rosencher J, Empana JP, Carli P, Mira JP, Jouven X. Immediate percutaneous coronary intervention is associated with better survival after out-of-hospital cardiac arrest: insights from the PROCAT (Parisian Region Out of hospital Cardiac ArresT) registry. Circ Cardiovasc Interv. 2010;3:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 565] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 22. | Anyfantakis ZA, Baron G, Aubry P, Himbert D, Feldman LJ, Juliard JM, Ricard-Hibon A, Burnod A, Cokkinos DV, Steg PG. Acute coronary angiographic findings in survivors of out-of-hospital cardiac arrest. Am Heart J. 2009;157:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 149] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 23. | Dumas F, Manzo-Silberman S, Fichet J, Mami Z, Zuber B, Vivien B, Chenevier-Gobeaux C, Varenne O, Empana JP, Pène F. Can early cardiac troponin I measurement help to predict recent coronary occlusion in out-of-hospital cardiac arrest survivors? Crit Care Med. 2012;40:1777-1784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 24. | Uppsala University. Direct or Subacute Coronary Angiography for Out-of-hospital Cardiac Arrest (DISCO). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Available from: https://clinicaltrials.gov/ct2/show/NCT02309151 NLM Identifier: NCT02309151. |
| 25. | University of Arizona. Early Coronary Angiography Versus Delayed Coronary Angiography (PEARL). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Available from: https://clinicaltrials.gov/ct2/show/NCT02387398 NLM Identifier: NCT02387398. |
| 26. | Hospital San Carlos, Madrid. Coronary in out of hospital cardiac arrest (COUPE). In: ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). Available from: https://clinicaltrials.gov/ct2/show/NCT02641626 ClinicalTrials.gov Identifier: NCT02641626. |
| 27. | Lemkes JS, Janssens GN, Straaten HM, Elbers PW, van der Hoeven NW, Tijssen JG, Otterspoor LC, Voskuil M, van der Heijden JJ, Meuwissen M. Coronary angiography after cardiac arrest: Rationale and design of the COACT trial. Am Heart J. 2016;180:39-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Patel N, Patel NJ, Macon CJ, Thakkar B, Desai M, Rengifo-Moreno P, Alfonso CE, Myerburg RJ, Bhatt DL, Cohen MG. Trends and Outcomes of Coronary Angiography and Percutaneous Coronary Intervention After Out-of-Hospital Cardiac Arrest Associated With Ventricular Fibrillation or Pulseless Ventricular Tachycardia. JAMA Cardiol. 2016;1:890-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 29. | Granfeldt A, Wissenberg M, Hansen SM, Lippert FK, Lang-Jensen T, Hendriksen OM, Torp-Pedersen C, Christensen EF, Christiansen CF. Clinical predictors of shockable versus non-shockable rhythms in patients with out-of-hospital cardiac arrest. Resuscitation. 2016;108:40-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |