Published online Jul 26, 2017. doi: 10.4330/wjc.v9.i7.629
Peer-review started: November 10, 2016
First decision: March 7, 2017
Revised: April 19, 2017
Accepted: May 3, 2017
Article in press: May 5, 2017
Published online: July 26, 2017
Processing time: 260 Days and 14.1 Hours
Open surgery is the elective treatment for mycotic aneurysms of the aorta. This surgery consists of resection of the aneurysm, debridement and revascularization with an in situ or extra-anatomic bypass. Even when surgery has been successful, the morbi-mortality is raised and the endovascular treatment has become an alternative for specific patients. When mycotic aneurysms involved the visceral arteries, more complex techniques are necessary such as fenestrated endovascular aortic repair or chimmeny endovascular aortic repair and the most frequent complications of this are endoleaks and oclussion the visceral arteries. We present a case of a pacient with a paravisceral abdominal mycotic aneurysms that was result with 2 chimney technique (in the right renal and superior mesenteric arteries) and a single Nellix EVAS (Endologix, Irvine, Calif) of 12 cm long without evidence of endoleaks in the follow-up.
Core tip: The interesting of the case that we present is the resolution of the mycotic aneurysms throw a new techniques calls chimmeny endovascular sealing (Ch-EVAS). This case it would be the first case treated with Ch-EVAS that has been reported since in the bibliographical review that we made we do not find cases of paravisceral abdominal mycotic aneurysms treated with this technology.
- Citation: Rabellino M, Moltini PN, Di Caro VG, Chas JG, Marenchino R, Garcia-Monaco RD. Endovascular treatment of paravisceral mycotic aneurysm: Chimmeny endovascular sealing the end of de road. World J Cardiol 2017; 9(7): 629-633
- URL: https://www.wjgnet.com/1949-8462/full/v9/i7/629.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i7.629
Open surgery is the elective treatment for mycotic aneurysms of the aorta. This surgery consists of resection of the aneurysm, debridement and revascularization with an in situ or extra-anatomic bypass[1]. Even when surgery has been successful, the morbi-mortality is raised and the endovascular treatment has become an alternative for specific patients[2].
The main problem of this kind of pseudoaneurysms is the location. When the mycotic aneurysm is in the descending aorta or infrarenal aorta without compromising the supra-aortic trunks or the visceral arteries, endovascular treatment is possible with a successful outcome[2]. Nevertheless, it has not been well described in the literature this type of procedure for paravisceral abdominal aortic aneurysm.
When mycotic aneurysms involved the visceral arteries, more complex techniques are necessary such as Fenestrated endovascular aortic repair (f-EVAR) or chimmeny endovascular aortic repair (Ch-EVAR) and the most frequent complications of this are endoleaks and oclussion the visceral arteries[3,4].
We present a case of a pacient with a paravisceral abdominal mycotic aneurysms with absolute contraindication for open surgery with two unsuccessful endovascular treatments, that was result with chimney technique and Nellix (Endologix, Irvine, Calif) chimmeny endovascular sealing (Ch-EVAS).
A 72-year-old woman was admitted in the emergency department presented with acute abdomnal pain. She had a medical history of former smoker, multiple coronary by-pass with dehiscence of the chest wound, pulmonary embolism treated with anticoagulants and respiratory failure (SpO2 82%).
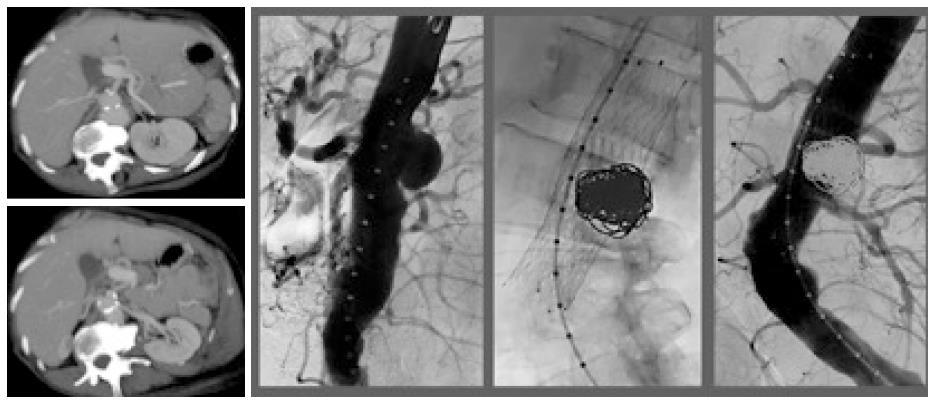
To the physical examination, the patient was presenting an acute abdominal pain with rigidity, guarding and peritoneal irritation so an AngioCT scan was performed and showed gastrointestinal perforation and a 4.9 cm paravisceral abdominal aneurysms with intraluminal thrombus (Figure 1A). Small bowel resection and jejunostomy was done. Anatomopathology showed miliary tuberculosis with intestinal involvement and peritoneal implants.
With this result and the presence of the aortic aneurysms we made the diagnosis of tuberculous mycotic aneurysm with compromise of the four visceral branches. Although, the endovascular treatment was decided because of the clinical situation of the patient, the endovascular options have not been simple because of the location of the aneurysms. The options were a f-EVAR, which was impossible for the time confection or a Ch-EVAR with the risk of endoleaks in the pseudoaneurysms that needs 4 chimney.
Another therapeutic option was Ch-EVAS which was not available in our country. Base on the foregoing, and knowing that it was not a definitive treatment, the decision was to perform stent assisted coil embolization technique of the aneurysms.
In the procedure, for a femoral access a Sinus XL stent (OptiMed, Ettlingen, Germany) was placed in the aortic visceral topography and across it embolization of the pseudoaneurysm with coils was performed with a successful initial first result (Figure 1B and D) and without complications. The patient was discharged 48 h later with parenteral nutrition, aspirin 100 mg/d and antibiotics therapy for tuberculosis.
Four month later, an AngioCT scan revealed that the mycotic aneurysm had grown and a for a percutaneous femoral access a balloon-assisted coils and n-butyl 2-cyanoacrylate embolization was performed with good angiographic outcomes (Figure 2). The patient was still undergoing treatment for her infection disease and was discharged 24 h later without complications. Bowel transit and abdominal wall reconstruction was made a month later. Two month after surgery, the patient was admitted with low back pain and the CT angiogram showed an endoleak with aneurysm sac enlargement and extravasation of the embolic agents used previously that indicated rupture, so an endovascular treatment with Ch-EVAS was decided, because it was already available in our country.
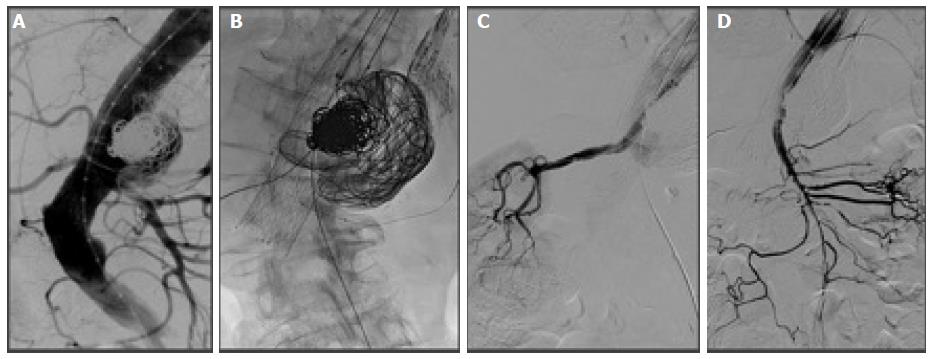
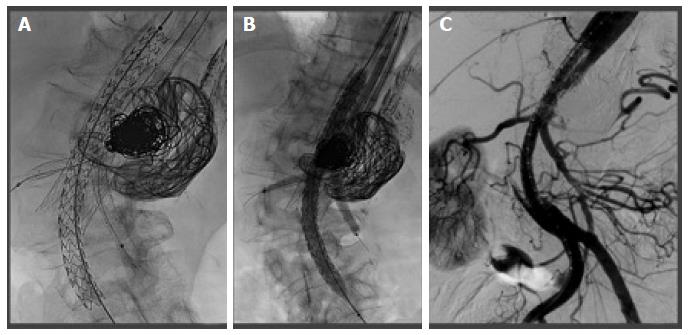
Under general anesthesia a percutaneous femoral access was done for the introduction of a single Nellix EVAS of 12 cm long (the aortic diameter was normal and it was not necessary to spread up to the iliac arteries) and a open left subclavian access to place the chimneys for the right renal and superior mesenteric arteries. Both chimneys were performed with a Viabahn covered stent (Gore and Associates, Flagstaff, AZ) of 7 mm × 100 mm for the right renal artery and 8 mm × 100 mm for the superior mesenteric artery. Inside the chimneys a nitinol self-expanding stent was placed to give them a greater radial force strength and to avoid the chimney collapse by the polymer (Figure 3).
The left renal artery was catheterized but it was not possible to advance a catheter across the strut of the Sinus stent, so an angioplasty with a 6-mm low-profile coronary balloon was performed. Despite these, it was not possible to introduce a 4 Fr diagnostic catheter so it was decided to abandon the left renal artery. It was decided not to be catheterized the celtrunk for the idea that it would be compensated for the superior mesenteric artery, as it happened.
The final angiographic control showed the exclusion of the mycotic aneurysms with permeability of the right renal artery and superior mesenteric artery which supply the celiac trunk and its branches (Figure 4). After the procedure, the patient was discharged 5 d later without complications, normal renal function, clopidogrel 75 mg, aspirin 100 mg a day and antibiotic therapy. AngioCT scan follow-up at 3 mo, showed absence of endoleaks and permeability of the right renal artery, superior mesenteric artery and the celiac trunk.
Open surgery is the elective treatment for mycotic aneurysms of the aorta, however in patient with absolute contraindication for surgery, the endovascular treatment become an important alternative for this patients that have been well described in the multicentric European study which concluded that endovascular treatment it is a feasible and lasting option in most patients[2]. Nevertheless, in this study of all treated aneurysms only in the 7% of them it was used f-EVAR techniques, not having specific comments about the follow-up in these patients. Another endovscular option for the treatment of paravisceral abdominal mycotic aneurysms is the Ch-EVAR. However, the rate of endoleaks with this technique in a review by Patel et al[4] was estimated at 5% to 37.5%.
In a recent review by Li et al[5] the rate of endoleaks type IA was11.8% with a permeability of the branches of 96.6% at 6 mo. Because of these, in our case we this alternative was scorned in view of the high percentage of endoleaks (4 or 3 chimneys were necessary) and the consequent risk of rupture. In this location, the f-EVAR is a good choice to treat this aneurysm. The only problem is the time of confection that limits the use in pseudoaneurysms that need an early resolution. In the last 2 years, it has been reported some cases of paravisceral aneurysms treated with Ch-EVAS technique that show promising result[6-8]. Torella et al[7] presented 2 cases of juxtarenal aortic aneurysms treated with Ch-EVAS with 2 chimneys in each case and without evidence of endoleaks type IA. Youssef et al[6] published recently a series of 7 patients treated with Ch-EVAS with four chimneys for patient in which they reported no early endoleaks with a permeability of 96% of the branches to 6 mo of follow-up.
The Ch-EVAS turns out to be a interesting concept since the polymer realizes a copy of the aortic anatomy occupying the space of the gutters that they originate with the conventional Ch-EVAR technique reducing the risk of endoleaks. The case that we presented it would be the first case treated with Ch-EVAS that has been reported since in the bibliographical review that we made we do not find cases of paravisceral abdominal mycotic aneurysms treated with this technology. While so far, the reports on Ch-EVAS are only clinical case reports, they represent encouraging results as a future alternative of first choice for the treatment of paravisceral aortic aneurysms.
A 72-year-old woman with a medical history of military tuberculosis with abdominal involment that was treated in two opportunities for a mycotic aortic aneurysm with compromise of the four visceral branches with endovascular technique was admitted at the emergency department with low back pain two months after the second treatment.
Computed tomography angiogram showed an endoleak with mycotic aneurysm enlargement.
Endovascular treatment performed with Chimney endovascular aneurysm sealing (Ch-EVAS) with good result with exclution and absent of endoleaks in the final angiography control. In the follow up the patient continuos asintomatyc with no evidence of endoleaks or another complication.
A mycotic aneurysm of the aorta with involvement of the visceral arteries is a dreadful condition and repair it can be quite challenging. The endovascular treatment has become an important alternative. The Ch-EVAS turns out to be a interesting concept because it solves the endoleaks problems with the conventional chimney endovascular aneurysm repair). In the authors’ bibliographical review, the authors did not find cases of paravisceral abdominal mycotic aneurysms treated with this technology.
This is an interesting case report about the endovascular treatment of paravisceral mycotic aneurysm.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Argentina
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Schoenhagen P, Teragawa H, Ueda H S- Editor: Ji FF L- Editor: Logan S E- Editor: Wu HL
| 1. | Hsu RB, Chen RJ, Wang SS, Chu SH. Infected aortic aneurysms: clinical outcome and risk factor analysis. J Vasc Surg. 2004;40:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Sörelius K, Mani K, Björck M, Sedivy P, Wahlgren CM, Taylor P, Clough RE, Lyons O, Thompson M, Brownrigg J. Endovascular treatment of mycotic aortic aneurysms: a European multicenter study. Circulation. 2014;130:2136-2142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Donas KP, Torsello G, Bisdas T, Osada N, Schönefeld E, Pitoulias GA. Early outcomes for fenestrated and chimney endografts in the treatment of pararenal aortic pathologies are not significantly different: a systematic review with pooled data analysis. J Endovasc Ther. 2012;19:723-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | Patel RP, Katsargyris A, Verhoeven EL, Adam DJ, Hardman JA. Endovascular aortic aneurysm repair with chimney and snorkel grafts: indications, techniques and results. Cardiovasc Intervent Radiol. 2013;36:1443-1451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Li Y, Zhang T, Guo W, Duan C, Wei R, Ge Y, Jia X, Liu X. Endovascular chimney technique for juxtarenal abdominal aortic aneurysm: a systematic review using pooled analysis and meta-analysis. Ann Vasc Surg. 2015;29:1141-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Youssef M, Dünschede F, El Beyrouti H, Salem O, Vahl CF, Dorweiler B. Endovascular Repair of Paravisceral Aortic Aneurysms Combining Chimney Grafts and the Nellix Endovascular Aneurysm Sealing Technology (Four-Vessel ChEVAS). Thorac Cardiovasc Surg. 2017;65:112-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Torella F, Chan TY, Shaikh U, England A, Fisher RK, McWilliams RG. ChEVAS: Combining Suprarenal EVAS with Chimney Technique. Cardiovasc Intervent Radiol. 2015;38:1294-1298. [PubMed] |
| 8. | Malkawi AH, de Bruin JL, Loftus IM, Thompson MM. Treatment of a juxtarenal aneurysm with the Nellix endovascular aneurysm sealing system and chimney stent. J Endovasc Ther. 2014;21:538-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |