Published online Mar 26, 2017. doi: 10.4330/wjc.v9.i3.261
Peer-review started: September 2, 2016
First decision: October 26, 2016
Revised: November 14, 2016
Accepted: December 16, 2016
Article in press: December 19, 2016
Published online: March 26, 2017
Processing time: 207 Days and 15.3 Hours
To investigate the relationship of inferior wall ischemia on myocardial perfusion imaging in patients with non-dominant right coronary artery anatomy.
This was a retrospective observational analysis of consecutive patients who presented to the emergency department with primary complaint of chest pain. Only patients who underwent single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) were included. Patients who showed a reversible defect on SPECT MPI and had coronary angiography during the same hospitalization was analyzed. Patients with prior history of coronary artery disease (CAD) including history of percutaneous coronary intervention and coronary artery bypass graft surgerys were excluded. True positive and false positive results were identified on the basis of hemodynamically significant CAD on coronary angiography, in the same territory as identified on SPECT MPI. Coronary artery dominance was determined on coronary angiography. Patients were divided into group 1 and group 2. Group 1 included patients with non-dominant right coronary artery (RCA) (left dominant and codominant). Group 2 included patients with dominant RCA anatomy. Demographics, baseline characteristics and positive predictive value (PPV) were analyzed for the two groups.
The mean age of the study cohort was 57.6 years. Sixty-one point seven percent of the patients were males. The prevalence of self-reported diabetes mellitus, hypertension and dyslipidemia was 36%, 71.9% and 53.9% respectively. A comparison of baseline characteristics between the two groups showed that patients with a non-dominant RCA were more likely to be men. For inferior wall ischemia on SPECT MPI, patients in study group 2 had a significantly higher PPV, 32/42 (76.1%), compared to patients in group 1, in which only 3 out of the 29 patients (10.3%) had true positive results (P value < 0.001 Z test). The difference remained statistically significant even when only patients with left dominant coronary system (without co-dominant) were compared to patients with right dominant system (32/40, 76.1% in right dominant group, 3/19, 15.8% in left dominant group, P value < 0.001 Z test). There was no significant difference in mean hospital stay, re-hospitalization, and in-hospital mortality between the two groups.
The positive predictive value of SPECT MPI for inferior wall ischemia is affected by coronary artery dominance. More studies are needed to explain this phenomenon.
Core tip: A positive test for ischemia on single photon emission computed tomography (SPECT), myocardial perfusion imaging (MPI) is often followed up with coronary angiography. The aim of our study was to assess the relationship of inferior wall ischemia on SPECT MPI with non-dominant right coronary artery (RCA) anatomy. We found that positive predictive value of inferior wall ischemia on SPECT MPI was significantly lower in patients with non-dominant RCA anatomy. We postulate that in non-dominant RCA anatomy flow tracer may show relatively decreased uptake in the inferior wall that might not be indicative of flow limiting stenosis.
- Citation: Malik AO, Abela O, Devabhaktuni S, Malik AA, Allenback G, Ahsan CH, Malhotra S, Diep J. Significance of inferior wall ischemia in non-dominant right coronary artery anatomy. World J Cardiol 2017; 9(3): 261-267
- URL: https://www.wjgnet.com/1949-8462/full/v9/i3/261.htm
- DOI: https://dx.doi.org/10.4330/wjc.v9.i3.261
Single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is most often used to assess the likelihood of obstructive coronary artery disease (CAD), presence of ischemia in a patient with known CAD, and evaluating the extent of ischemia for prognostic value[1]. In essence SPECT MPI accomplishes this by measuring relative changes in perfusion of myocardial territories before and after augmenting coronary blood flow[1]. SPECT MPI has enjoyed widespread clinical use because of its well documented diagnostic and prognostic utility in CAD[2].
Coronary artery dominance is determined by the artery supplying the posterior portion of interventricular (IV) septum[3]. In a right dominant system, the right coronary artery (RCA) supplies this territory and feeds the posterior descending artery, in contrast to left dominant system in which the left circumflex artery (LCX) accomplishes this role[3]. In a co-dominant system, the supply of posterior IV septum is shared by both RCA and LCX[3]. Right dominant system is the more prevalent variant occurring in approximately 70% of people, followed by left dominant and co-dominant system[4].
The prognostic significance of coronary artery dominance in patients with CAD has been studied. Left dominant system has been shown to be an independent risk factor of morbidity and mortality in patients undergoing both surgical and percutaneous revascularization, especially in patients with ST segment elevated myocardial infarction (STEMI)[4-7].
The effect of coronary anatomy on diagnostic accuracy of cardiac magnetic resonance imaging (CMR) has been studied[8]. However, no study to our knowledge has evaluated the effect of coronary artery dominance on diagnostic accuracy of SPECT (MPI studies). We present the first report showing the effect of coronary artery dominance on positive predictive value of SPECT MPI.
The study was a single center retrospective analysis conducted at a tertiary care center.
All patients who underwent rest and stress SPECT MPI from January 1st 2013 to June 30th 2014, for diagnostic purposes were included in our study. All patients who did not undergo a coronary angiogram during the same hospital stay were excluded. Furthermore, all patients who did not have evidence of reversible ischemia on SPECT MPI were excluded.
These patients presented with chest pain that were deemed to be of intermediate pre-test probability for ischemia. The images were initially read by an experienced radiologist and results verified by the cardiologist.
The study was approved by the Institute Review Board at University Medical Center of Southern Nevada. This study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
All of the patients subsequently underwent a coronary angiogram during the same hospital stay after the SPECT MPI. Patients were divided into two groups on the basis of coronary artery dominance. Group 1 included patients with a non-dominant RCA (left dominant and co-dominant). Group 2 included patients with right dominant coronary artery system.
The coronary angiogram was performed by an experienced interventional cardiologist. It was noted if there was obstructive CAD, in the same distribution as shown by the SPECT MPI the study was deemed to be true positive. Obstructive CAD was defined as maximal coronary artery stenosis of more than 70%.
SPECT MPI was performed using standard protocols approved by the American Society of Nuclear Cardiology[9]. An experienced radiologist initially read the images and the presence of any reversible ischemia was verified by the cardiology team. Figure 1 shows representative images of SPECT MPI, showing inferior wall ischemia and normal scan respectively.
The primary study outcome was determining diagnostic accuracy of the SPECT MPI, with the coronary angiogram as gold standard. The positive predictive value of SPECT MPI was compared in both groups.
Data for each study variable were summarized initially for the whole cohort and then by dominant coronary artery group, using means for continuous variables and frequencies/percentages for categorical variables. Means for the non-dominant RCA and dominant RCA groups were compared using independent-samples t-tests (or Mann Whitney U tests, for variables with non-normally distributed data). Frequencies/percentages were compared using χ2 tests. Positive predictive values for were compared via Z tests of proportions. The significance level (alpha) was set at 0.05, and all analyses were completed via SPSS, version 22 (IBM).
The mean age of the study cohort was 57.6 years. Sixty-one point seven percent of the patients were males. The prevalence of self-reported diabetes mellitus, hypertension and dyslipidemia was 36%, 71.9% and 53.9% respectively. A comparison of baseline characteristics between the two groups showed that patients with a non-dominant RCA were more likely to be men. Table 1 shows comparison of other baseline characteristics.
| Dominant RCA n = 87 | Non- dominant RCA n = 41 | P value (test) | |
| Age | 56.92 yr | 59.24 yr | 0.252 (t test) |
| Male gender | 48/87 (55.17) | 31/41 (75.61) | 0.026 (χ2) |
| BMI | 28.29 | 28.87 | 0.459 (Mann-Whitney) |
| PMH of DM | 33/87 (37.93) | 14/41 (34.15) | 0.679 (χ2) |
| PMH HTN | 64/87 (73.56) | 27/41 (65.85) | 0.369 (χ2) |
| PMH dyslipidemia | 51/87 (58.62) | 18/41 (43.90) | 0.119 (χ2) |
| PMH of a fib | 2/87 (2.30) | 1/41 (2.45) | 1.000 (χ2) |
| PMH of PVD | 17/87 (19.54) | 8/41 (19.51) | 0.997 (χ2) |
| PMH of COPD | 5/87 (5.75) | 7/41 (17.07) | 0.053 (χ2) |
| Current smoker | 27/87 (31.03) | 15/41 (36.59) | 0.533 (χ2) |
| Drug abuse | 10/87 (11.49) | 7/41 (17.07) | 0.386 (χ2) |
| Alcohol use | 23/87 (26.45) | 11/40 (27.50) | 0.900 (χ2) |
| PMH of sleep apnea | 3/87 (3.45) | 1/41 (2.44) | 1.000 (χ2) |
| PMH of CKD | 9/87 (10.34) | 2/41 (4.88) | 0.501 (χ2) |
| ESRD on HD | 4/87 (4.60) | 2/41 (4.88) | 1.000 (χ2) |
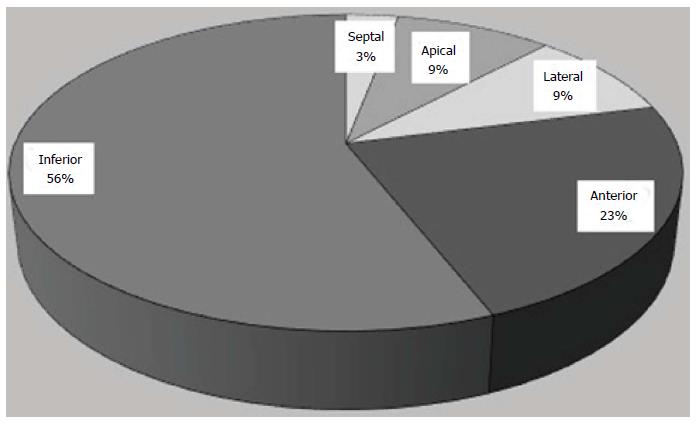
The most common location for the reversible defect was seen the inferior wall (Figure 2).
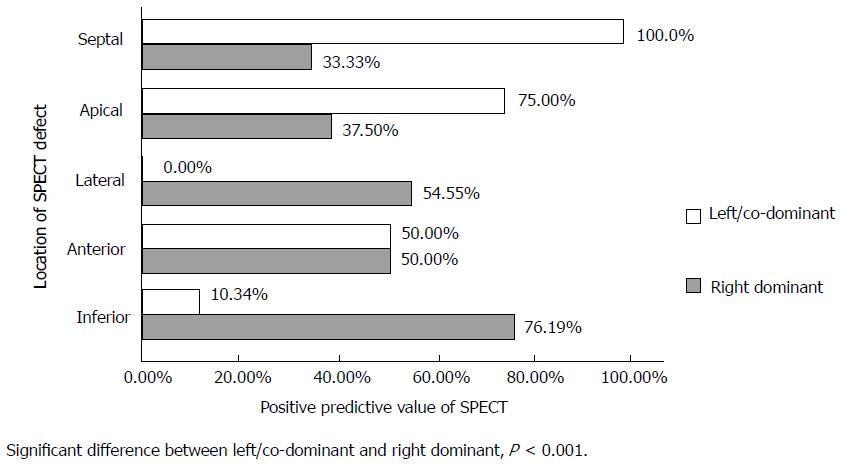
The positive predictive value (PPV) was analyzed and compared between the two study groups. Sub-group analysis showed that for inferior wall ischemia on SPECT MPI, patients in study group 2 had a significantly higher PPV, 32/42 (76.1%), compared to patients in group 1, in which PPV was 10.3% (3/29) (P value < 0.001 Z test) Figure 2 illustrates the results. The difference remained statistically significant even when only patients with left dominant coronary system (without co-dominant) were compared to patients with right dominant system. (32/40, 76.1% in right dominant group, 3/19, 15.8% in left dominant group, P value < 0.001 Z test).
There was no significant difference in mean hospital stay, re-hospitalization, and in-hospital mortality between the two groups as shown in Table 2.
| Dominant RCA n = 87 | Non-dominant RCA n = 41 | P value (test) | |
| Mean hospital stay (d) | 4.33 | 4.29 | 0.713 (Mann-Whitney) |
| In-hospital mortality | 0/87 | 0/41 | - |
| 30-d re-hospitalization for chest pain | 10/87 (11.49%) | 2/41 (4.88%) | 0.231 (χ2) |
Around 15 million patients seek medical attention for symptoms concerning for CAD[10]. In stable patients, not having acute coronary syndrome non-invasive testing like SPECT MPI, act as gatekeepers to coronary angiography because of risks and costs associated with coronary angiography[11,12]. Despite the use of conventional non-invasive testing such as SPECT MPI an analysis of almost 400000 coronary angiograms in patients with no prior history of CAD disease revealed no obstructive disease in more than 60% of the cases, resulting in unnecessary risks and costs[13,14]. Hence, from a public health standpoint, it is imperative that we study the reasons for false positive diagnoses associated with non-invasive tests such as SPECT MPI.
SPECT MPI is widely used for diagnostic purposes in patients presenting with chest pain when acute coronary syndrome (ACS) has been ruled out[2]. A recent study showed that SPECT MPI is widely used for diagnostic and risk stratification purposes in the United States and patient’s socio-economic status did not significantly affect the use of SPECT MPI by physicians[15]. In the developing world several studies have shown the widespread use of SPECT MPI by physicians to aid in diagnosis in management[16,17]. One such report from Iran regarding SPECT MPI referral practices showed that 72.5% (211/291) of the referrals found to be appropriate per ASNC recommendations[16].
The utilization of SPECT MPI is often on the physician’s assessment of pre-test probability. The American College of Physicians pre-test probability assessment and Duke chest pain score are two common objective tools used for this assessment[18]. In our retrospective analysis, SPECT MPI was done, on the physician’s assessment of the patient’s pre-test probability.
Our study shows that SPECT MPI in patients with non-dominant RCA has significantly high false positive results for inferior wall ischemia. In a study using positron emission tomography measuring absolute myocardial blood flow (MBF) in low risk normal patients’ authors found baseline MBF in the inferior region was significantly (P < 0.0001) lower than either the anterior or lateral regions[19]. However, coronary anatomy was not available in this study population. Nonetheless this finding may contribute to our observation as well. One study using stress CMR also showed a statistically significant difference in false positive rate correlating with dominance[8]. They also showed a correlation with the vessel size, postulating that the smaller vessel size that usually comes with non-dominant vessels was the factor leading to false positive readings[8].
Gender differences in vessel caliber and coronary artery dominance could also play a role. As shown in our results patients with non-dominant RCA were more likely to be men. This is consistent with the report by Gebhard et al[5] in which patients with left dominant coronary artery anatomy were more likely to be males. In contrast in a cohort of patients with STEMI, lower percentage of patients with left dominant circulation were men compared to patients with right dominant circulation[7]. This was not statistically significant. Vessel caliber was not available in either of these studies. Whether gender differences affect coronary artery, dominance is not clear at this time.
Regardless our study finding has important consequences. First, it has been shown that patients with left dominant system are at high risk in terms of cardiovascular events[6]; hence, it is important that significant CAD is promptly addressed in these patients. If the diagnostic accuracy of SPECT MPI is particularly low in this sub group of patients, then it is important that more studies are done to evaluate the negative predictive value (NPV) in this subset to reach a better understanding about role of SPECT MPI in excluding significant CAD in these patients. In our retrospective analysis patients with negative SPECT MPI imaging did not have a coronary angiogram, hence analysis of NPV was not possible.
Second, if the diagnostic accuracy of inferior wall ischemia on SPECT MPI is affected by coronary artery dominance and it has a significantly lower PPV in patients with non-dominant RCA, it would mean that many patients in this sub-group are exposed to unnecessary invasive procedures. This is in addition to utilizing the resources when it will not help the patient.
In conclusion, based on our findings we hypothesize that the flow tracer in a non-dominant RCA may show relatively decreased uptake in the inferior wall that might not be indicative of flow limiting stenosis. More multi-center studies to explore the relationship of coronary artery dominance on SPECT MPI are needed to reach a better understanding regarding positive or negative results in patients in the context of non-dominant RCA anatomy.
This study was done only at a single center and the SPECT MPI results were only read by one group of physicians. Prone imaging was not done. Also some patients could have could have had inferior wall abnormality and coronary computed tomography angiogram was not utilized. Coronary angiograms were not done on patients with normal SPECT MPI results. Hence we could not analyze the effect of coronary dominance on NPV. We did not strictly use objective validated models to quantify SPECT MPI defect so some measurement bias may be present.
Single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) is most often used to assess the likelihood of obstructive coronary artery disease (CAD), presence of ischemia in a patient with known CAD, and evaluating the ex-tent of ischemia for prognostic value. SPECT MPI has enjoyed widespread clinical use be-cause of its well documented diagnostic and prognostic utility in CAD. The authors’ study aims to understand the effect of coronary artery dominance on the positive predictive value (PPV) of SPECT MPI.
The effect of coronary anatomy on diagnostic accuracy of cardiac magnetic resonance imaging (CMR) has been studied. However, no study to our knowledge has evaluated the effect of coronary artery dominance on diagnostic accuracy of SPECT MPI studies. The authors’ present the first report showing the effect of coronary artery dominance on PPV of SPECT MPI.
They studied the effect of coronary artery dominance on the PPV of SPECT MPI. The effect of coronary anatomy on diagnostic accuracy of cardiac magnetic resonance imaging (CMR) has been studied. In a study using positron emission tomography measuring absolute myocardial blood flow (MBF) in low risk normal patients’ authors found baseline MBF in the inferior region was significantly lower than either the anterior or lateral regions. However, coronary anatomy was not available in this study population. They studied the effect of coronary artery dominance on the PPV of SPECT MPI.
In stable patients, not having acute coronary syndrome non-invasive testing like SPECT MPI, act as gatekeepers to coronary angiography because of risks and costs as-sociated with coronary angiography. Despite the use of conventional non-invasive testing such as SPECT MPI an analysis of almost 400000 coronary angiograms in pa-tients with no prior history of CAD disease revealed no obstructive disease in more than 60% of the cases, resulting in unnecessary risks and costs. Hence, from a public health standpoint, it is imperative that the study the reasons for false positive diagnoses associated with non-invasive tests such as SPECT MPI. They show in the study that the PPV of SPECT MPI for inferior wall ischemia in stable patients no having ACS, is affected by coronary artery dominance. Although more studies are needed to explain this phenomenon, maybe this subset of patients should undergo further non-invasive testing before proceeding to invasive coronary angiography.
SPECT MPI: SPECT MPI is most often used to assess the likelihood of obstructive CAD, presence of ischemia in a patient with known CAD, and evaluating the ex-tent of ischemia for prognostic value. In essence SPECT MPI accomplishes this by measuring relative changes in perfusion of myocardial territories before and after aug-menting coronary blood flow; coronary artery dominance: Coronary artery dominance is determined by the artery supplying the posterior portion of interventricular (IV) septum. In a right dominant system, the right coronary artery (RCA) supplies this territory and feeds the posterior descending artery, in contrast to left dominant system in which the left circumflex artery (LCX) accomplishes this role. In a co-dominant system, the supply of posterior IV septum is shared by both RCA and LCX.
This is an interesting manuscript about the association of a positive test for inferior wall ischemia on MPI with non-dominant RCA anatomy.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Kettering K, Najafi M, Rauch B, Ueda H S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Beller GA, Heede RC. SPECT imaging for detecting coronary artery disease and determining prognosis by noninvasive assessment of myocardial perfusion and myocardial viability. J Cardiovasc Transl Res. 2011;4:416-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Garcia EV. Physical attributes, limitations, and future potential for PET and SPECT. J Nucl Cardiol. 2012;19 Suppl 1:S19-S29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Parikh NI, Honeycutt EF, Roe MT, Neely M, Rosenthal EJ, Mittleman MA, Carrozza JP, Ho KK. Left and codominant coronary artery circulations are associated with higher in-hospital mortality among patients undergoing percutaneous coronary intervention for acute coronary syndromes: report From the National Cardiovascular Database Cath Percutaneous Coronary Intervention (CathPCI) Registry. Circ Cardiovasc Qual Outcomes. 2012;5:775-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Omerbasic E, Hasanovic A, Omerbasic A, Pandur S. Prognostic value of anatomical dominance of coronary circulation in patients with surgical myocardial revascularization. Med Arch. 2015;69:6-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Gebhard C, Fuchs TA, Stehli J, Gransar H, Berman DS, Budoff MJ, Achenbach S, Al-Mallah M, Andreini D, Cademartiri F. Coronary dominance and prognosis in patients undergoing coronary computed tomographic angiography: results from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) registry. Eur Heart J Cardiovasc Imaging. 2015;16:853-862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Lam MK, Tandjung K, Sen H, Basalus MW, van Houwelingen KG, Stoel MG, Louwerenburg JW, Linssen GC, Saïd SA, Nienhuis MB. Coronary artery dominance and the risk of adverse clinical events following percutaneous coronary intervention: insights from the prospective, randomised TWENTE trial. EuroIntervention. 2015;11:180-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Veltman CE, van der Hoeven BL, Hoogslag GE, Boden H, Kharbanda RK, de Graaf MA, Delgado V, van Zwet EW, Schalij MJ, Bax JJ. Influence of coronary vessel dominance on short- and long-term outcome in patients after ST-segment elevation myocardial infarction. Eur Heart J. 2015;36:1023-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Pilz G, Heer T, Graw M, Ali E, Klos M, Scheck R, Zeymer U, Höfling B. Influence of small caliber coronary arteries on the diagnostic accuracy of adenosine stress cardiac magnetic resonance imaging. Clin Res Cardiol. 2011;100:201-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Dorbala S, Di Carli MF, Delbeke D, Abbara S, DePuey EG, Dilsizian V, Forrester J, Janowitz W, Kaufmann PA, Mahmarian J. SNMMI/ASNC/SCCT guideline for cardiac SPECT/CT and PET/CT 1.0. J Nucl Med. 2013;54:1485-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 165] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 10. | Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, de Ferranti S, Després JP, Fullerton HJ, Howard VJ. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3462] [Cited by in RCA: 4535] [Article Influence: 412.3] [Reference Citation Analysis (1)] |
| 11. | Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A, Bugiardini R, Crea F, Cuisset T, Di Mario C. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J. 2013;34:2949-3003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2772] [Cited by in RCA: 2994] [Article Influence: 249.5] [Reference Citation Analysis (0)] |
| 12. | Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126:3097-3137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 289] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 13. | Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV, Brindis RG, Douglas PS. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010;362:886-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1067] [Cited by in RCA: 1230] [Article Influence: 82.0] [Reference Citation Analysis (0)] |
| 14. | Patel MR, Dai D, Hernandez AF, Douglas PS, Messenger J, Garratt KN, Maddox TM, Peterson ED, Roe MT. Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am Heart J. 2014;167:846-852.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 206] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 15. | Doukky R, Hayes K, Frogge N, Nazir NT, Collado FM, Williams KA. Impact of insurance carrier, prior authorization, and socioeconomic status on appropriate use of SPECT myocardial perfusion imaging in private community-based office practice. Clin Cardiol. 2015;38:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Gholamrezanezhad A, Shirafkan A, Mirpour S, Rayatnavaz M, Alborzi A, Mogharrabi M, Hassanpour S, Ramezani M. Appropriateness of referrals for single-photon emission computed tomography myocardial perfusion imaging (SPECT-MPI) in a developing community: a comparison between 2005 and 2009 versions of ACCF/ASNC appropriateness criteria. J Nucl Cardiol. 2011;18:1044-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Dos Santos MA, Santos MS, Tura BR, Félix R, Brito AS, De Lorenzo A. Budget impact of applying appropriateness criteria for myocardial perfusion scintigraphy: The perspective of a developing country. J Nucl Cardiol. 2016;23:1160-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Bom MJ, van der Zee PM, Cornel JH, van der Zant FM, Knol RJ. Diagnostic and Therapeutic Usefulness of Coronary Computed Tomography Angiography in Out-Clinic Patients Referred for Chest Pain. Am J Cardiol. 2015;116:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Chareonthaitawee P, Kaufmann PA, Rimoldi O, Camici PG. Heterogeneity of resting and hyperemic myocardial blood flow in healthy humans. Cardiovasc Res. 2001;50:151-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 260] [Article Influence: 10.8] [Reference Citation Analysis (0)] |