Published online Sep 26, 2014. doi: 10.4330/wjc.v6.i9.916
Revised: April 2, 2014
Accepted: July 15, 2014
Published online: September 26, 2014
Processing time: 241 Days and 13.8 Hours
Apical hypertrophic cardiomyopathy (AHCM) is a relatively rare morphologic variant of HCM in which the hypertrophy of myocardium is localized to the left ventricular apex. Symptoms of AHCM might vary from none to others mimic coronary artery disease including acute coronary syndrome, thus resulting in inappropriate hospitalization. Transthoracic echocardiography is the first-line imaging technique for the diagnosis of hypertrophic cardiomyopathies. However, when the hypertrophy of the myocardium is localized in the ventricular apex might results in missed diagnosis. Aim of this paper is to review the different imaging techniques used for the diagnosis of AHCM and their role in the detection and comprehension of this uncommon disease.
Core tip: Apical hypertrophic cardiomyopathy (AHCM) is a relatively rare morphologic variant of HCM in which the hypertrophy of myocardium is localized to the left ventricular apex. Aim of this paper is to review the different imaging techniques used for the diagnosis of AHCM and their role in the detection and comprehension of this uncommon disease.
- Citation: Parisi R, Mirabella F, Secco GG, Fattori R. Multimodality imaging in apical hypertrophic cardiomyopathy. World J Cardiol 2014; 6(9): 916-923
- URL: https://www.wjgnet.com/1949-8462/full/v6/i9/916.htm
- DOI: https://dx.doi.org/10.4330/wjc.v6.i9.916
Hypertrophic cardiomyopathy (HCM) is a genetic disorder caused by mutations in one or more of the genes encoding protein components of the cardiac sarcomere and transmitted with an autosomal dominant trait and variable penetrance[1,2]. The variability of these mutations leads to different morphological features of the pathology and influences patient prognosis[3,4].
Apical HCM (AHCM) is a relatively rare morphologic variant of HCM in which the hypertrophy of the myocardium is mainly localized to the left ventricular (LV) apex without the typical septal predominance, which characterize hypertrophic obstructive cardiomyopathy. A sarcomere protein gene defects have been found to be present from 13% to 30% of these patients[5]. It was first described in Japanese patients with precordial deep T wave inversions (referred to as giant T wave inversions) in 1976[6,7]. This condition is frequent in Asian population accounting for almost 25% of Japanese patients with HCM while its prevalence dramatically decrease in Caucasian patients to 1%-3%[8-10]. Male gender is the most frequently affected in the Japanese population but this gender difference has not been as relevant outside Japan[11]. Differences between the “pure” Japanese form of AHCM (hypertrophy of only the apical segments) and the non-Japanese form are reported. AHCM in Caucasian patients presents hypertrophy extended to the middle left ventricle’s segment segments (“mixed form”), with a worsened prognosis. These findings suggest a variability in the phenotypic expression of AHCM between countries and races with a possible additional role of environmental factors[12,13].
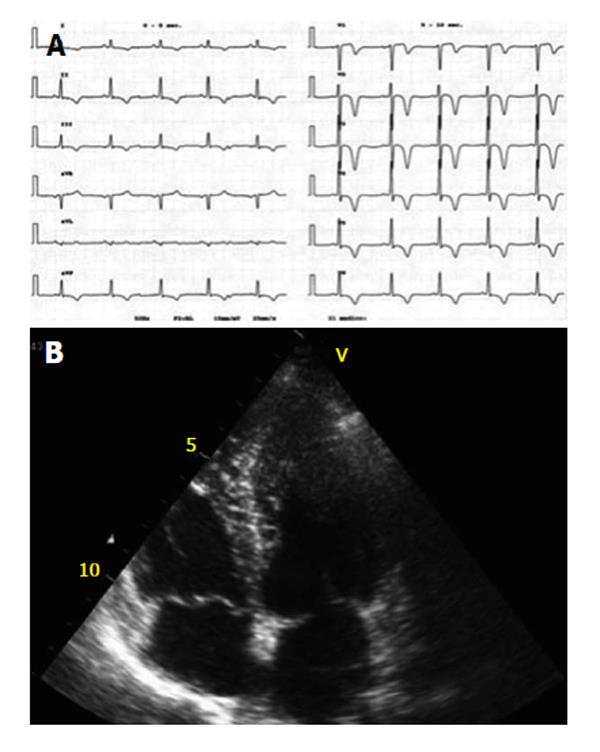
AHCM has a relatively benign prognosis in terms of cardiovascular mortality ranging around 0.1% in “pure” forms. However, one-third of the patients may experience unfavourable clinical events and life treating complications: diastolic dysfunction, myocardial infarction, left atrial enlargement with subsequent atrial fibrillation, apical aneurysm and thrombi with ventricular arrhythmias[10,12]. Moreover, progression into apical aneurysm or mid-ventricular obstruction is a variant and unfavourable feature of the disease. Symptoms might vary from none to others including chest pain in absence of angiographically proven coronary stenosis, palpitations, dyspnea, fatigue or syncope[14]. ECG pattern found in up to 90% of cases, include giant negative T waves at rest with transient normalization on exertion. Transthoracic echocardiography is currently the standard diagnostic tool for hypertrophic cardiomyopathies, however its diagnostic accuracy for identification of hypertrophy confined to the LV apex is limited.
Aim of this paper is to briefly review the different imaging techniques in the diagnosis of AHCM and their potential role in expanding our knowledge of this uncommon disease (Table 1).
| Echocardiography | SPECT | Angiography | MDCT | CMR | |
| LV morfology (dimensions, wall thickness) | ++ | - | + | ++ | +++ |
| Global and regional LV function | ++ | + | + | ++ | +++ |
| LV filling pressure | ++ | + | +++ | + | ++ |
| Radiation | - | + | + | + | - |
| Ischemia/CAD | + | ++ | +++ | ++ | ++ |
| Tissue characterisation | + | - | - | - | +++ |
| Cost | - | +++ | +++ | ++ | ++ |
Transthoracic echocardiography (TTE) is the first line imaging exam in patient with suspected AHCM because of its widespread availability and low-cost. On TTE, AHCM is defined as an absolute apical thickness of more than 15 mm with a ratio of apical to basal LV wall thickness of more than 1.3 (Figure 1). According to patterns of hypertrophy, two morphologically distinct phenotypes have been described: pure AHCM where the hypertrophy is limited to the apical segments and mixed AHCM with hypertrophy extending to the mid-ventricular level, sparing the basal segments[15]. Morphological subtypes have been found to be predictors of different prognosis and clinical manifestations[16]. Tissue Doppler technique enables to document a lowered coronary flow reserve capacity of penetrating intramyocardial coronary arteries[17]. However, because of technical artefacts and variability of imaging quality, TTE might results in poor detection of endocardial border thus resulting in misleading diagnosis[18]. Patients with AHCM might develop apical aneurysms and clots mimicking other conditions such as cardiac tumor, isolated ventricular non-compaction, endomiocardial fibrosis, etc. The use of microbubbles contrast agent may improve diagnostic sensitivity[19-23].
Newer Doppler-based techniques have been successfully applied in the diagnosis of AHCM. Reddy et al[24] described paradoxical apical longitudinal strain (systolic lengthening) in two patients with AHCM despite an apparently normal apical wall motion on conventional TTE. Abecasis et al[25] using velocity vector imaging tissue characterization study found abnormal regional velocities and deformation parameters, particularly concerning base to apex longitudinal strain gradient, that could be related to the abnormal tissue hypertrophy extending beyond the more evident apical hypertrophic segments.
Multiplane transoesophageal echocardiography enables a correct visualization and sizing of ventricular segments and has been successfully applied in the diagnosis of AHCM[26].
Radionuclide scanning has also been used in diagnosis of AHCM. Reports of stress myocardial perfusion images in patients with AHCM have ranged from normal perfusion to reversible and fixed apical perfusion defects, often in the presence of normal epicardial coronary arteries[27]. The unbalanced wall thickness-to-vascular supply ratio leads to a relative apical ischemia[28,29]. Myocardial ischemic chest pain in the absence of coronary artery disease (CAD) has been related to limited coronary flow reserve in patients with asymmetric septal an apical hypertrophy[29-32]. Morishita et al[33] have also described increased uptake of Tc-99 m tetrofosmin in the apical segment on resting Single Photon Emission Computed Tomography (SPECT) polar maps in a subgroup of patients with AHCM. AHCM increased apical tracer uptake on resting Tl-201 planar and SPECT imaging has been previously reported[34]. Ward et al[35] showed a newly ‘‘Solar Polar’’ map pattern at rest. This “Solar Polar” map pattern on resting Tl-201 volume-weighted polar maps, sees an intensely bright spot of counts in the apical segment surrounded by a circumferential ring of decreasing counts. This study is the first describing the typical findings on dual-isotope rest and stress SPECT perfusion images and volume-weighted polar maps in non-Japanese patients with AHCM. Three different patterns characteristic of AHCM were identified[36]: an increased apical tracer uptake, a spade-like configuration of the LV chamber and the ‘‘Solar map’’ in 75% of patients; however no difference in apical thickness and magnitude of T-wave negativity between patients with normal SPECT and typical pattern were observed. Interstitial fibrosis that prevented the increased apical tracer uptake is the possible explanation for a normal SPECT study in patients with AHCM.
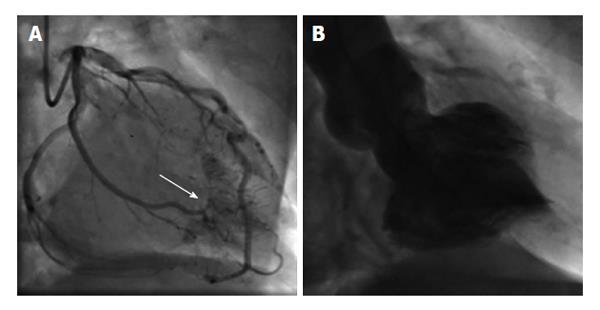
ECG changes and symptoms associated with AHCM often mimic acute coronary syndromes. Moreover elevated troponine serum levels reported in patients with AHCM and chest pain usually encourage physicians to perform invasive testing. Coronary angiography allows to exclude significant epicardial coronary lesions and enables detection of the associated congenital coronary artery anomalies, myocardial bridge or multiple coronary-LV fistulae[37]. Evaluation of the LV cavity can show the characteristic spade-like configuration of the left ventricle in end-diastole, with obliteration of the apical cavity in end-systole due to the vigour contraction of the hypertrophied myocardium[7] (Figure 2). Caucasian patients tend to have less localized involvement of the distal apex resulting in a lower frequency of the pathognomonic sign of “ace-of-spade” on the left ventriculography[13].
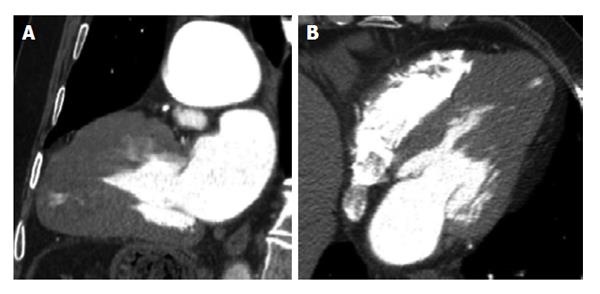
Coronary multidetector computed tomography (MDCT) is an high sensitive (91%-99%) and specific (74%-96%) technique in detecting significant coronary stenosis[38-40]. Major international guidelines currently indicate coronary MDCT for patients at a low to intermediate risk of CAD[41] and his adoption in the emergency room might facilitate early triage of patients presenting chest pain[42-44].
MDCT has also emerged as a novel technique for evaluating cardiac morphology and function. Initial concern with MDCT examination with radiation exposure have been overcome by novel technologies using dose-saving strategies[45,46]. Due to its high spatial resolution, MDCT can offer cardiac anatomical and functional information and a high quality non-invasive coronary evaluation[47-50]. It also enables accurate delineation of the apical endocardial border and dynamic evaluations of myocardial thickness, global and regional LV functions[51]. Multiplanar reconstructions along major cardiac axis allow to measure myocardial thickness on short-axis view in the end-diastolic phase while the apex can be evaluated in long axis planes (Figure 3). Knickelbine et al[52] have found nonatherosclerotic-related cardiovascular abnormalities judged to be of potential clinical relevance in 4.4% of 4543 patients with suspected atherosclerotic CAD undergoing to 64-slice MDCT. In 50 of these patients (1.1%) the abnormality was previously unrecognized. The most common abnormalities were: congenital coronary artery anomalies (38%), ascending aortic aneurysms > 45 mm (22%), hypertrophic cardiomyopathy with apical LV wall thickening (14%), valvular heart diseases (8%), congenital heart diseases including ventricular septal defect (6%), pulmonary embolus (6%), LV noncompaction, left atrial myxoma, and LV apical aneurysm (2%). Chen et al[53] have performed MDCT in 14 patients with known diagnosis of AHCM. Left ventricle shapes reconstructions of MDCT were similar to angiography, with “ace-of-spades” configurations, apical sequestrations and apical aneurysm. Furthermore, MDCT was able to detect two cases of significant coronary stenosis and 7 patients with myocardial bridges.
In the last few years cardiovascular magnetic resonance (CMR) has emerged as a useful and accurate imaging technique for diagnosis of HCM. Both European and American Cardiology Society indicated CMR as first choice exam or at least equivalent to other diagnostic methods in the approach of several cardiomyopathies, including HCM[54,55].
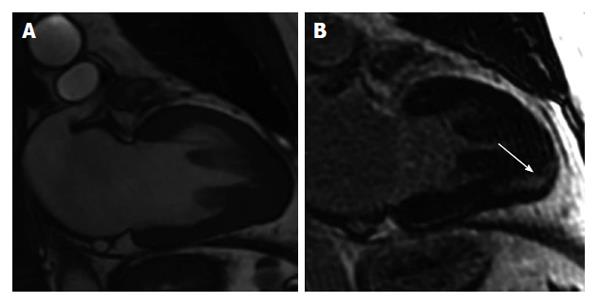
The excellence of CMR in analyse anatomy and function has increased the sensitivity and specificity of the diagnosis of HCM[56]. A comparative study of TTE and CMR among HCM subjects demonstrated the greater accuracy of CMR identifying different patterns of hypertrophy. Among subjects with confined hypertrophy in anterolateral wall, echocardiography underestimates wall thickness and poorly evaluates the apical segments in up to 40%[57-59]. AHCM may mimic other pathological conditions such as coronary artery disease, myocardial tumor, ventricular aneurysm, ventricular non-compaction or endomyocardial fibrosis and CMR can be useful in differential diagnosis. CMR provides a more accurate assessment of LV apical hypertrophy allowing detection of HCM related complications and wall motion abnormalities (Figure 4). Tsukamoto et al[60] using CMR-tagging showed systolic outward motion of the LV apical wall in AHCM patients. LV apical aneurysms have been reported in up to 2% of all patients with HCM, with a rate of related adverse events of 10.5% per year, considerably higher with respect to HCM without aneurysm[61]. Notably, a higher incidence of apical aneurysms, ranging from 10% to 20%[62,63], has been reported in AHCM. In a case series, Fattori et al[64] showed that TTE was able to detect only 1 of the 4 cases of AHCM related apical aneurysms, suggesting the use of CMR in all patients affected by AHCM in order to confirm the diagnosis and to ascertain the presence of aneurysms. Indeed, the presence of an apical aneurysm, especially if associated with the detection of ventricular tachyarrhythmias, could support the decision to implant a cardioverter-defibrillator.
CMR appears to be more sensitive than other imaging techniques in detecting infarct areas and ischemia, identifying even subendocardial infarction with late gadolinium-enhanced (LGE)[65,66]. LGE-CMR has been used to visualize myocardial interstitial abnormalities in patients with different forms of cardiomyopathies, including non-ischemic forms[67,68]. LGE has been found to be present in a high proportion of patients with HCM and has been associated with a higher incidence of ventricular tachycarrythmias and risk of sudden death[69,70]. In patients with apical hypertrophic cardiomyopathy, the incidence of LGE seems to be less common with respect to other form of HCMP, but it is similarly associated to a worse prognosis. In the largest available series of AHCM patients imaged with magnetic resonance imaging, LGE was reported only in 40% of cases and limited to the hypertrophic apical segments[71]. However, others studies showed that LGE was not limited to the hypertrophic apical segments but also present in the midventricular and basal segments of interventricular septum, potential expression of myocardial damage preceding the abnormal hypertrophy. LGE-CMR should be applied for longitudinal follow-up studies to detect development and progression of AHCM related fibrotic tissue formations highlighting the subsets of patients associated with worse prognosis[72].
The correct diagnosis of AHCM is of major importance. Multimodality imaging is essential in increasing the detection of AHCM, yielding larger study populations. In particular, CMR showed an excellent accuracy in identifying the abnormal LV hypertrophy. With late gadolinium enhancement, CMR is able to in vivo detect abnormal myocardial structure allowing a more accurate risk stratification.
P- Reviewer: Driscoll D S- Editor: Wen LL L- Editor: A E- Editor: Liu SQ
| 1. | Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113:1807-1816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2284] [Cited by in RCA: 2243] [Article Influence: 118.1] [Reference Citation Analysis (0)] |
| 2. | Arad M, Penas-Lado M, Monserrat L, Maron BJ, Sherrid M, Ho CY, Barr S, Karim A, Olson TM, Kamisago M. Gene mutations in apical hypertrophic cardiomyopathy. Circulation. 2005;112:2805-2811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 145] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Spirito P, Seidman CE, McKenna WJ, Maron BJ. The management of hypertrophic cardiomyopathy. N Engl J Med. 1997;336:775-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 683] [Cited by in RCA: 612] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 4. | Wigle ED, Sasson Z, Henderson MA, Ruddy TD, Fulop J, Rakowski H, Williams WG. Hypertrophic cardiomyopathy. The importance of the site and the extent of hypertrophy. A review. Prog Cardiovasc Dis. 1985;28:1-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 600] [Cited by in RCA: 545] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 5. | Gruner C, Care M, Siminovitch K, Moravsky G, Wigle ED, Woo A, Rakowski H. Sarcomere protein gene mutations in patients with apical hypertrophic cardiomyopathy. Circ Cardiovasc Genet. 2011;4:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Sakamoto T, Tei C, Murayama M, Ichiyasu H, Hada Y. Giant T wave inversion as a manifestation of asymmetrical apical hypertrophy (AAH) of the left ventricle. Echocardiographic and ultrasono-cardiotomographic study. Jpn Heart J. 1976;17:611-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 230] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Yamaguchi H, Ishimura T, Nishiyama S, Nagasaki F, Nakanishi S, Takatsu F, Nishijo T, Umeda T, Machii K. Hypertrophic nonobstructive cardiomyopathy with giant negative T waves (apical hypertrophy): ventriculographic and echocardiographic features in 30 patients. Am J Cardiol. 1979;44:401-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 334] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 8. | Chikamori T, Doi YL, Akizawa M, Yonezawa Y, Ozawa T, McKenna WJ. Comparison of clinical, morphological, and prognostic features in hypertrophic cardiomyopathy between Japanese and western patients. Clin Cardiol. 1992;15:833-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Maron BJ. Hypertrophic cardiomyopathy: a systematic review. JAMA. 2002;287:1308-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1394] [Cited by in RCA: 1423] [Article Influence: 61.9] [Reference Citation Analysis (0)] |
| 10. | Kitaoka H, Doi Y, Casey SA, Hitomi N, Furuno T, Maron BJ. Comparison of prevalence of apical hypertrophic cardiomyopathy in Japan and the United States. Am J Cardiol. 2003;92:1183-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 140] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 11. | Abinader EG, Rauchfleisch S, Naschitz J. Hypertrophic apical cardiomyopathy: a subtype of hypertrophic cardiomyopathy. Isr J Med Sci. 1982;18:1005-1009. [PubMed] |
| 12. | Matsumori A, Ohashi N, Sasayama S. Hepatitis C virus infection and hypertrophic cardiomyopathy. Ann Intern Med. 1998;129:749-750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Louie EK, Maron BJ. Apical hypertrophic cardiomyopathy: clinical and two-dimensional echocardiographic assessment. Ann Intern Med. 1987;106:663-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 71] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Sakamoto T. Apical hypertrophic cardiomyopathy (apical hypertrophy): an overview. J Cardiol. 2001;37 Suppl 1:161-178. [PubMed] |
| 15. | Eriksson MJ, Sonnenberg B, Woo A, Rakowski P, Parker TG, Wigle ED, Rakowski H. Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;39:638-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 306] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 16. | Choi EY, Rim SJ, Ha JW, Kim YJ, Lee SC, Kang DH, Park SW, Song JK, Sohn DW, Chung N. Phenotypic spectrum and clinical characteristics of apical hypertrophic cardiomyopathy: multicenter echo-Doppler study. Cardiology. 2008;110:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Youn HJ, Lee JM, Park CS, Ihm SH, Cho EJ, Jung HO, Jeon HK, Oh YS, Chung WS, Kim JH. The impaired flow reserve capacity of penetrating intramyocardial coronary arteries in apical hypertrophic cardiomyopathy. J Am Soc Echocardiogr. 2005;18:128-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Prasad K, Atherton J, Smith GC, McKenna WJ, Frenneaux MP, Nihoyannopoulos P. Echocardiographic pitfalls in the diagnosis of hypertrophic cardiomyopathy. Heart. 1999;82 Suppl 3:III8-III15. [PubMed] |
| 19. | Olszewski R, Timperley J, Szmigielski C, Monaghan M, Nihoyannopoulos P, Senior R, Becher H. The clinical applications of contrast echocardiography. Eur J Echocardiogr. 2007;8:S13-S23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Ward RP, Weinert L, Spencer KT, Furlong KT, Bednarz J, DeCara J, Lang RM. Quantitative diagnosis of apical cardiomyopathy using contrast echocardiography. J Am Soc Echocardiogr. 2002;15:316-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Soman P, Swinburn J, Callister M, Stephens NG, Senior R. Apical hypertrophic cardiomyopathy: bedside diagnosis by intravenous contrast echocardiography. J Am Soc Echocardiogr. 2001;14:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Mulvagh SL, Rakowski H, Vannan MA, Abdelmoneim SS, Becher H, Bierig SM, Burns PN, Castello R, Coon PD, Hagen ME. American Society of Echocardiography Consensus Statement on the Clinical Applications of Ultrasonic Contrast Agents in Echocardiography. J Am Soc Echocardiogr. 2008;21:1179-1201; quiz 1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 324] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 23. | Spirito P, Maron BJ. Relation between extent of left ventricular hypertrophy and occurrence of sudden cardiac death in hypertrophic cardiomyopathy. J Am Coll Cardiol. 1990;15:1521-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 115] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 24. | Reddy M, Thatai D, Bernal J, Pradhan J, Afonso L. Apical hypertrophic cardiomyopathy: potential utility of Strain imaging. Eur J Echocardiogr. 2008;9:560-562. [PubMed] |
| 25. | Abecasis J, Dourado R, Arroja I, Azevedo J, Silva A. Utility of tissue characterization in apical hypertrophic cardiomyopathy diagnosis. Eur J Echocardiogr. 2009;10:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Crowley JJ, Dardas PS, Shapiro LM. Assessment of apical hypertrophic cardiomyopathy using transoesophageal echocardiography. Cardiology. 1997;88:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Wang Y, Takigawa O, Handa S, Hatakeyama K, Suzuki Y. [The mechanism of giant negative T wave in electrocardiogram in patients with apical hypertrophic cardiomyopathy: evaluation with thallium-201 and iodine-123 metaiodobenzylguanidine myocardial scintigraphy]. Kaku Igaku. 1996;33:999-1004. [PubMed] |
| 28. | Reddy V, Korcarz C, Weinert L, Al-Sadir J, Spencer KT, Lang RM. Apical hypertrophic cardiomyopathy. Circulation. 1998;98:2354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Bertrand ME, Tilmant PY, Lablanche JM, Thieuleux FA. Apical hypertrophic cardiomyopathy: clinical and metabolic studies. Eur Heart J. 1983;4 Suppl F:127-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Maron BJ, Epstein SE, Roberts WC. Hypertrophic cardiomyopathy and transmural myocardial infarction without significant atherosclerosis of the extramural coronary arteries. Am J Cardiol. 1979;43:1086-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 260] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 31. | Cannon RO, Rosing DR, Maron BJ, Leon MB, Bonow RO, Watson RM, Epstein SE. Myocardial ischemia in patients with hypertrophic cardiomyopathy: contribution of inadequate vasodilator reserve and elevated left ventricular filling pressures. Circulation. 1985;71:234-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 311] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 32. | O’Gara PT, Bonow RO, Maron BJ, Damske BA, Van Lingen A, Bacharach SL, Larson SM, Epstein SE. Myocardial perfusion abnormalities in patients with hypertrophic cardiomyopathy: assessment with thallium-201 emission computed tomography. Circulation. 1987;76:1214-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 175] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 33. | Morishita S, Kondo Y, Nomura M, Miyajima H, Nada T, Ito S, Nakaya Y. Impaired retention of technetium-99m tetrofosmin in hypertrophic cardiomyopathy. Am J Cardiol. 2001;87:743-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 34. | Chu WW, Wallhaus TR, Bianco JA. SPECT imaging of apical hypertrophic cardiomyopathy. Clin Nucl Med. 2002;27:785-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Ward RP, Pokharna HK, Lang RM, Williams KA. Resting “Solar Polar” map pattern and reduced apical flow reserve: characteristics of apical hypertrophic cardiomyopathy on SPECT myocardial perfusion imaging. J Nucl Cardiol. 2003;10:506-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 36. | Cianciulli TF, Saccheri MC, Masoli OH, Redruello MF, Lax JA, Morita LA, Gagliardi JA, Dorelle AN, Prezioso HA, Vidal LA. Myocardial perfusion SPECT in the diagnosis of apical hypertrophic cardiomyopathy. J Nucl Cardiol. 2009;16:391-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 37. | Dresios C, Apostolakis S, Tzortzis S, Lazaridis K, Gardikiotis A. Apical hypertrophic cardiomyopathy associated with multiple coronary artery-left ventricular fistulae: a report of a case and review of the literature. Eur J Echocardiogr. 2010;11:E9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 38. | Abdulla J, Abildstrom SZ, Gotzsche O, Christensen E, Kober L, Torp-Pedersen C. 64-multislice detector computed tomography coronary angiography as potential alternative to conventional coronary angiography: a systematic review and meta-analysis. Eur Heart J. 2007;28:3042-3050. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 243] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 39. | Hamon M, Biondi-Zoccai GG, Malagutti P, Agostoni P, Morello R, Valgimigli M, Hamon M. Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol. 2006;48:1896-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 317] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 40. | Mowatt G, Cook JA, Hillis GS, Walker S, Fraser C, Jia X, Waugh N. 64-Slice computed tomography angiography in the diagnosis and assessment of coronary artery disease: systematic review and meta-analysis. Heart. 2008;94:1386-1393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 340] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 41. | Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P, Rubin GD. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Cardiovasc Comput Tomogr. 2010;4:407.e1-407.33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 112] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 42. | Hoffmann U, Nagurney JT, Moselewski F, Pena A, Ferencik M, Chae CU, Cury RC, Butler J, Abbara S, Brown DF. Coronary multidetector computed tomography in the assessment of patients with acute chest pain. Circulation. 2006;114:2251-2260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 259] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 43. | Rubinshtein R, Halon DA, Gaspar T, Jaffe R, Karkabi B, Flugelman MY, Kogan A, Shapira R, Peled N, Lewis BS. Usefulness of 64-slice cardiac computed tomographic angiography for diagnosing acute coronary syndromes and predicting clinical outcome in emergency department patients with chest pain of uncertain origin. Circulation. 2007;115:1762-1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 245] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 44. | Goldstein JA, Gallagher MJ, O’Neill WW, Ross MA, O’Neil BJ, Raff GL. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol. 2007;49:863-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 490] [Cited by in RCA: 440] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 45. | Coles DR, Smail MA, Negus IS, Wilde P, Oberhoff M, Karsch KR, Baumbach A. Comparison of radiation doses from multislice computed tomography coronary angiography and conventional diagnostic angiography. J Am Coll Cardiol. 2006;47:1840-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 188] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 46. | Zanzonico P, Rothenberg LN, Strauss HW. Radiation exposure of computed tomography and direct intracoronary angiography: risk has its reward. J Am Coll Cardiol. 2006;47:1846-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 47. | Yoshida M, Takamoto T. Left ventricular hypertrophic patterns and wall motion dynamics in hypertrophic cardiomyopathy: an electron beam computed tomographic study. Intern Med. 1997;36:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 48. | Ghersin E, Lessick J, Litmanovich D, Engel A, Reisner S. Comprehensive multidetector CT assessment of apical hypertrophic cardiomyopathy. Br J Radiol. 2006;79:e200-e204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Juergens KU, Wessling J, Fallenberg EM, Mönnig G, Wichter T, Fischbach R. Multislice cardiac spiral CT evaluation of atypical hypertrophic cardiomyopathy with a calcified left ventricular thrombus. J Comput Assist Tomogr. 2000;24:688-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Williams TJ, Manghat NE, McKay-Ferguson A, Ring NJ, Morgan-Hughes GJ, Roobottom CA. Cardiomyopathy: appearances on ECG-gated 64-detector row computed tomography. Clin Radiol. 2008;63:464-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 51. | Kramer CM, Budoff MJ, Fayad ZA, Ferrari VA, Goldman C, Lesser JR, Martin ET, Rajogopalan S, Reilly JP, Rodgers GP. ACCF/AHA 2007 clinical competence statement on vascular imaging with computed tomography and magnetic resonance: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training: developed in collaboration with the Society of Atherosclerosis Imaging and Prevention, the Society for Cardiovascular Angiography and Interventions, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society for Vascular Medicine and Biology. Circulation. 2007;116:1318-1335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Knickelbine T, Lesser JR, Haas TS, Brandenburg ER, Gleason-Han BK, Flygenring B, Longe TF, Schwartz RS, Maron BJ. Identification of unexpected nonatherosclerotic cardiovascular disease with coronary CT angiography. JACC Cardiovasc Imaging. 2009;2:1085-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 53. | Chen CC, Chen MT, Lei MH, Hsu YC, Chung SL, Sung YJ. Assessing myocardial bridging and left ventricular configuration by 64-slice computed tomography in patients with apical hypertrophic cardiomyopathy presenting with chest pain. J Comput Assist Tomogr. 2010;34:70-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 54. | Pennell DJ, Sechtem UP, Higgins CB, Manning WJ, Pohost GM, Rademakers FE, van Rossum AC, Shaw LJ, Yucel EK. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report. Eur Heart J. 2004;25:1940-1965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 545] [Cited by in RCA: 481] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 55. | Budoff MJ, Cohen MC, Garcia MJ, Hodgson JM, Hundley WG, Lima JA, Manning WJ, Pohost GM, Raggi PM, Rodgers GP. ACCF/AHA clinical competence statement on cardiac imaging with computed tomography and magnetic resonance: a report of the American College of Cardiology Foundation/American Heart Association/American College of Physicians Task Force on Clinical Competence and Training. J Am Coll Cardiol. 2005;46:383-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 159] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 56. | Bellenger NG, Francis JM, Davies CL, Coats AJ, Pennell DJ. Establishment and performance of a magnetic resonance cardiac function clinic. J Cardiovasc Magn Reson. 2000;2:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 57. | Rickers C, Wilke NM, Jerosch-Herold M, Casey SA, Panse P, Panse N, Weil J, Zenovich AG, Maron BJ. Utility of cardiac magnetic resonance imaging in the diagnosis of hypertrophic cardiomyopathy. Circulation. 2005;112:855-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 367] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 58. | Moon JC, Fisher NG, McKenna WJ, Pennell DJ. Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart. 2004;90:645-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 276] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 59. | Pons-Lladó G, Carreras F, Borrás X, Palmer J, Llauger J, Bayés de Luna A. Comparison of morphologic assessment of hypertrophic cardiomyopathy by magnetic resonance versus echocardiographic imaging. Am J Cardiol. 1997;79:1651-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 60. | Tsukamoto M, Hirasaki S, Kuribayashi T, Matsuo A, Matsui H, Sawada T, Nakamura T, Azuma A, Sugihara H, Matsubara H. Systolic outward motion of the left ventricular apical wall as detected by magnetic resonance tagging in patients with apical hypertrophic cardiomyopathy. J Cardiovasc Magn Reson. 2006;8:453-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 61. | Maron MS, Finley JJ, Bos JM, Hauser TH, Manning WJ, Haas TS, Lesser JR, Udelson JE, Ackerman MJ, Maron BJ. Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy. Circulation. 2008;118:1541-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 386] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 62. | Nakamura T, Matsubara K, Furukawa K, Azuma A, Sugihara H, Katsume H, Nakagawa M. Diastolic paradoxic jet flow in patients with hypertrophic cardiomyopathy: evidence of concealed apical asynergy with cavity obliteration. J Am Coll Cardiol. 1992;19:516-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 85] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 63. | Matsubara K, Nakamura T, Kuribayashi T, Azuma A, Nakagawa M. Sustained cavity obliteration and apical aneurysm formation in apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2003;42:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 100] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 64. | Fattori R, Biagini E, Lorenzini M, Buttazzi K, Lovato L, Rapezzi C. Significance of magnetic resonance imaging in apical hypertrophic cardiomyopathy. Am J Cardiol. 2010;105:1592-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 65. | van Rugge FP, Holman ER, van der Wall EE, de Roos A, van der Laarse A, Bruschke AV. Quantitation of global and regional left ventricular function by cine magnetic resonance imaging during dobutamine stress in normal human subjects. Eur Heart J. 1993;14:456-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 66. | Langerak SE, Vliegen HW, de Roos A, Zwinderman AH, Jukema JW, Kunz P, Lamb HJ, van Der Wall EE. Detection of vein graft disease using high-resolution magnetic resonance angiography. Circulation. 2002;105:328-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 76] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 67. | Mahrholdt H, Wagner A, Deluigi CC, Kispert E, Hager S, Meinhardt G, Vogelsberg H, Fritz P, Dippon J, Bock CT. Presentation, patterns of myocardial damage, and clinical course of viral myocarditis. Circulation. 2006;114:1581-1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 661] [Cited by in RCA: 589] [Article Influence: 31.0] [Reference Citation Analysis (0)] |
| 68. | Silva C, Moon JC, Elkington AG, John AS, Mohiaddin RH, Pennell DJ. Myocardial late gadolinium enhancement in specific cardiomyopathies by cardiovascular magnetic resonance: a preliminary experience. J Cardiovasc Med (Hagerstown). 2007;8:1076-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 69. | Adabag AS, Maron BJ, Appelbaum E, Harrigan CJ, Buros JL, Gibson CM, Lesser JR, Hanna CA, Udelson JE, Manning WJ. Occurrence and frequency of arrhythmias in hypertrophic cardiomyopathy in relation to delayed enhancement on cardiovascular magnetic resonance. J Am Coll Cardiol. 2008;51:1369-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 499] [Cited by in RCA: 465] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 70. | Moon JC, McKenna WJ, McCrohon JA, Elliott PM, Smith GC, Pennell DJ. Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. J Am Coll Cardiol. 2003;41:1561-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 575] [Cited by in RCA: 511] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 71. | Yamada M, Teraoka K, Kawade M, Hirano M, Yamashina A. Frequency and distribution of late gadolinium enhancement in magnetic resonance imaging of patients with apical hypertrophic cardiomyopathy and patients with asymmetrical hypertrophic cardiomyopathy: a comparative study. Int J Cardiovasc Imaging. 2009;25 Suppl 1:131-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 72. | Gebker R, Neuss M, Paetsch I, Nagel E. Images in cardiovascular medicine. Progressive myocardial fibrosis in a patient with apical hypertrophic cardiomyopathy detected by cardiovascular magnetic resonance. Circulation. 2006;114:e75-e76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |