Published online Jul 26, 2013. doi: 10.4330/wjc.v5.i7.254
Revised: April 25, 2013
Accepted: June 1, 2013
Published online: July 26, 2013
Processing time: 174 Days and 7.1 Hours
Patent foramen ovale (PFO) closure for systemic hypoxemia is controversial. The first systematic, albeit retrospective, study was recently presented which showed good procedural and clinical success for PFO closure for this indication. We present a case of acute right to left intra-cardiac shunt across PFO where the shunting is not persistent. Hence making a decision on PFO closure based on the aforementioned promising trial may not have been the right decision for the patient. This case highlights that the decision on PFO closure for such indication needs to be individualized. We also review the sparse literature on PFO closure for this indication and discuss how the decision making for such indication needs to be individualized.
Core tip: Patent foramen ovale (PFO) is a common, yet benign entity most of the time. Rarely, it is known to play role in causation of stroke, migraine and even rarely, profound hypoxemia. We report a rare case of severe hypoxemia due to PFO where the shunting is not persistent. We also review the sparse literature on PFO closure for this indication and discuss how the decision making for such indication needs to be individualized.
- Citation: Pant S, Hayes K, Deshmukh A, Rutlen DL. Hypoxemia without persistent right-to-left pressure gradient across a patent foramen ovale: A clinical challenge. World J Cardiol 2013; 5(7): 254-257
- URL: https://www.wjgnet.com/1949-8462/full/v5/i7/254.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i7.254
Patent foramen ovale (PFO) closure for systemic hypoxemia is controversial. The first systematic, albeit retrospective, study was recently presented which showed good procedural and clinical success for PFO closure for this indication.
A 83-year-old female was transferred from an outside facility after an extensive evaluation for acute hypoxemia. She initially presented with worsening shortness of breath over a few days, aggravated by exertion but without any orthopnea or paroxysmal nocturnal dyspnea. She denied cough or chest pain. Her past medical history was significant for hypertension, osteoarthritis, transient ischemic attacks, gastroesophageal reflux disease, osteoporosis and coronary artery disease. During the recent admission to the outside facility, she had undergone a left heart catheterization (LHC) with stenting of the left circumflex and obtuse marginal arteries. The right coronary was chronically totally occluded and attempt to revascularize it was unsuccessful. The pressure and oxygen saturation data is presented in Table 1. Ventilation/perfusion scan showed low probability for pulmonary embolism (PE). Lung perfusion scintigraphy demonstrated increased uptake underlying the calvarium suspicious for right to left shunt.
| Location | Pressure (mmHg) | Oxygen saturation |
| Right atrium | 2 | |
| High | 65% | |
| Medium | 63% | |
| Low | 67% | |
| Right ventricle | 2/18 | 60% |
| Pulmonary artery | 20/6 | 61% |
| Left atrium | 3 | 95% |
| Aorta | 95% | |
| Inferior venacava | 73% | |
| Superior venacava | 70% |
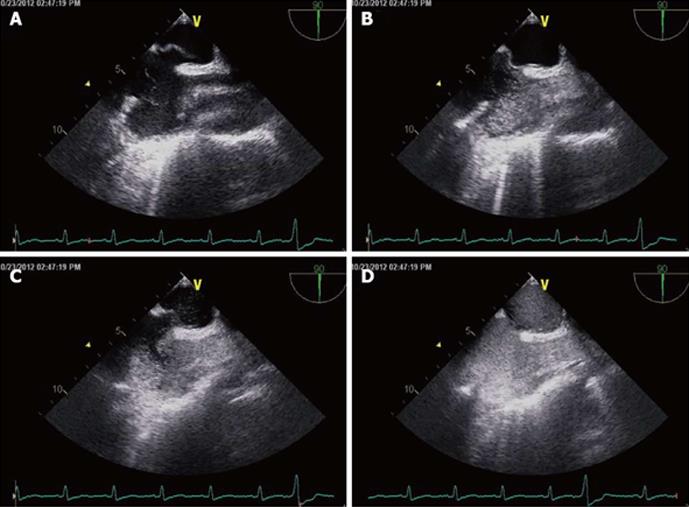
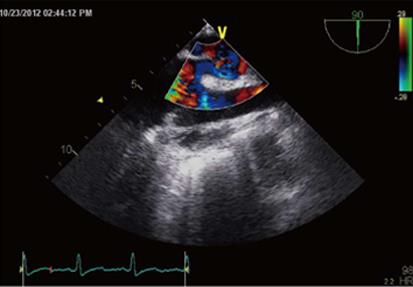
At presentation to our facility, her blood pressure was 139/73 mmHg, heart rate 113 beats per minute, respiratory rate 23 and oxygen saturation was 90% on nasal canula oxygen of 15 L/min. Systemic examination was unremarkable. Arterial blood gas on admission was pH 7.5, pCO2 25 mmHg, pO2 54 mmHg and HCO3- 19.5 mEq/L. Chest roentgenogram was normal. Computed tomography angiogram chest PE protocol was negative. The possibility of intra-cardiac shunt was initially thought less likely in the absence of a right-to-left pressure gradient on recent heart catheterization. The patient continued to remain hypoxemic. Blood gas evaluation performed with and without oxygen revealed no significant improvement in PaO2 with oxygen, suggesting right to left shunting at the intracardiac or intrapulmonary level. A transesophageal echocardiogram with bubble and doppler studies was subsequently done (Figures 1 and 2). Significant right to left shunting across a PFO was observed. The inter-atrial septum was markedly deviated to the left atrial side during systole and represented an atrial septal aneurysm. QP (pulmonary flow): QS (systemic flow) ratio could not be precisely estimated due to limited views of the right ventricular outflow tract but was approximately 0.7. This observation suggested significant right to left shunting. She was also found to have healthcare associated pneumonia during that time which was adequately treated with antibiotics. PFO closure was considered but it was thought that the large right to left shunting at the atrial level observed earlier was likely related to pulmonary vasoconstriction related to her pneumonia. After a few days, her oxygen requirement decreased. Blood gas evaluation was performed with (pH 7.3, pCO2 37 mmHg, pO2 68 mmHg and HCO3- 22 mEq/L) and without oxygen (pH 7.4, pCO2 34 mmHg, pO2 56 mmHg and HCO3- 21 mEq/L). Repeat echocardiogram showed persistent but decreased shunting. She was subsequently discharged to a nursing home on 2 L oxygen.
PFO occurs in nearly 30% of the adult population[1]. During the last decade, PFO and right-to-left shunting of venous blood has been linked to a number of disorders including cryptogenic headache, migraine and vascular headache, and decompression sickness with air embolism[2-4]. Recent reports have documented that acute right-to-left inter-atrial shunt (ARLIAS) across PFO may cause profound and difficult-to-treat hypoxemia[5-7]. This is often diagnosed unexpectedly during investigation for other causes of acute hypoxia. Echocardiography with bubble contrast remains the most sensitive, non-invasive and first line investigation for detection of ARLIAS[5]. The data on closure of PFO for hypoxemia derives mainly from case reports and series. Successful closure in these cases demands not only an acceptable peri-procedural and long term risk (known as “procedural success”) but also a complete reversal of the shunt and resolution of hypoxemia (known as “clinical success”). A systematic review by Khairy et al[7] in 2003 found that the incidence of major and minor complications of PFO closure was 1.5% and 7.9% respectively. Cardiac arrhythmias, device embolization, hemopericardium, right heart failure, transient ischemic attack and residual moderate to severe shunt are the known complications of device closure[7-9]. The indication for transcatheter closure of PFO reviewed by Nguyen et al[10] was for presumed paradoxical emboli. Over the last decade, there has been significant progress made in PFO closure terms of device technology, as well as the technique. Recently, a single-center, retrospective study of 104 patients undergoing PFO closure for systemic hypoxemia showed a good clinical safety as well as mechanical effectiveness of PFO closure using Amplatzer Cribriform atrial septal defect Occluder or Helex Septal Occluder.
The two prerequisite for development of ARLIAS arepresence of an interatrial shunt such as PFO or less commonly, atrial septal defect and a functional component that promotes abnormal shunting of the blood through the shunt. This includes various cardiac or pulmonary insults such as pulmonary embolus, severe asthma and right ventricular infarction or coronary artery bypass grafting that raises right atrial pressure above left atrial pressure. Treatment of such precipitating factors may cause resolution of hypoxemia as evident in our patient. Hence, the shunting process may not be persistent, as a result of which, the atrial chamber pressures could have been normal in our patient at the time of catheterization. A similar case of hypoxemia, without a persistent right-to-left pressure gradient has been reported by Marples et al[6]. As the underlying process progresses, a pressure gradient may develop across the PFO leading to right-to-left shunting. The process of shunting further worsens the hypoxia. This may tempt physicians to decide on PFO closure to correct the hypoxemia. However, such decision would have only invited more complications to our patient (such as right ventricular failure) and may not have been the right therapy for the patient’s hypoxemia. Hence, it is necessary to carefully consider the risk-to-benefit ratio and give due importance to physiological considerations before deciding on percutaneous device closure as a treatment modality for hypoxemia. If a reversible trigger for development of acute right-to-left shunting exists, appropriate management of that process may alleviate the need for device closure and related complications as seen in our patient.
P- Reviewer Vermeersch P S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | Fawcett E, Blachford JV. The Frequency of an Opening between the Right and Left Auricles at the Seat of the Foetal Foramen Ovale. J Anat Physiol. 1900;35:67-70. [PubMed] |
| 2. | Di Tullio M, Sacco RL, Gopal A, Mohr JP, Homma S. Patent foramen ovale as a risk factor for cryptogenic stroke. Ann Intern Med. 1992;117:461-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 409] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 3. | Ueka K. [Myastehnia gravis]. Nihon Rinsho. 1975;33:1956-1960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Schwerzmann M, Seiler C, Lipp E, Guzman R, Lövblad KO, Kraus M, Kucher N. Relation between directly detected patent foramen ovale and ischemic brain lesions in sport divers. Ann Intern Med. 2001;134:21-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Laybourn KA, Martin ET, Cooper RA, Holman WL. Platypnea and orthodeoxia: shunting associated with an aortic aneurysm. J Thorac Cardiovasc Surg. 1997;113:955-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Marples IL, Heap MJ, Suvarna SK, Mills GH. Acute right-to-left inter-atrial shunt; an important cause of profound hypoxia. Br J Anaesth. 2000;85:921-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Khairy P, O’Donnell CP, Landzberg MJ. Transcatheter closure versus medical therapy of patent foramen ovale and presumed paradoxical thromboemboli: a systematic review. Ann Intern Med. 2003;139:753-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 265] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 8. | Dewan NA, Gayasaddin M, Angelillo VA, O’Donohue WJ, Mohiuddin S. Persistent hypoxemia due to patent foramen ovale in a patient with adult respiratory distress syndrome. Chest. 1986;89:611-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Lemaire F, Richalet JP, Carlet J, Brun-Buisson C, MacLean C. Postoperative hypoxemia due to opening of a patent foramen ovale confirmed by a right atrium-left atrium pressure gradient during mechanical ventilation. Anesthesiology. 1982;57:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Nguyen BH, Satterfield L, Kim MS, Fenster B, Weinberger H. Percutaneous Closure of Patent Foramen Ovale for Systemic Hypoxemia: Patient Characteristics and Results in 104 Patients. American Heart Association 2012. Catheter-based and Surgical Interventions. Cited 2011-12-02. Available from: http: //circ.ahajournals.org/cgi/content/meetingabstract/122/21MeetingAbstracts/A21075. |