Published online Jun 26, 2013. doi: 10.4330/wjc.v5.i6.157
Revised: April 14, 2013
Accepted: May 17, 2013
Published online: June 26, 2013
Processing time: 171 Days and 7.9 Hours
Atrial fibrillation (AF) is a common arrhythmia with rising incidence. Obstructive sleep apnea (OSA) is prevalent among patients with AF. This observation has prompted significant research in understanding the relationship between OSA and AF. Multiple studies support a role of OSA in the initiation and progression of AF. This association has been independent of obesity, body mass index and hypertension. Instability of autonomic tone and wide swings in intrathoracic pressure are seen in OSA. These have been mechanistically linked to initiation of AF in OSA patients by lowering atrial effective refractory period, promoting pulmonary vein discharges and atrial dilation. OSA not only promotes initiation of AF but also makes management of AF difficult. Drug therapy and electrical cardioversion for AF are less successful in presence of OSA. There has been higher rate of early and overall recurrence after catheter ablation of AF in patients with OSA. Treatment of OSA with continuous positive airway pressure has been shown to improve control of AF. However, additional studies are needed to establish a stronger relationship between OSA treatment and success of AF therapies. There should be heightened suspicion of OSA in patients with AF. There is a need for guidelines to screen for OSA as a part of AF management.
Core tip: Obstructive sleep apnea (OSA) has been linked with the initiation and progression of atrial fibrillation (AF). Patients with OSA have lower success with therapies for AF. Continuous positive airway pressure has been shown to be effective in treatment of OSA and there is some evidence suggesting its role in improving AF control in patients with OSA. In this article, we review and discuss the available data explaining the potential pathophysiological mechanisms linking OSA and AF as well as the therapeutic and prognostic implications of the presence of OSA in AF patients.
- Citation: Goyal SK, Sharma A. Atrial fibrillation in obstructive sleep apnea. World J Cardiol 2013; 5(6): 157-163
- URL: https://www.wjgnet.com/1949-8462/full/v5/i6/157.htm
- DOI: https://dx.doi.org/10.4330/wjc.v5.i6.157
Atrial fibrillation (AF) is the most common cardiac arrhythmia and its prevalence has increased significantly in past three decades[1-3]. Hypertension, thyroid disease, coronary artery disease, cardiomyopathy and structural heart diseases are conventionally associated with high risk of AF[2,3]. Recently, a high prevalence of obstructive sleep apnea (OSA) has been noted among patients with AF indicating that OSA might be contributing to initiation and progression of AF[4,5].
OSA is a relatively common disorder and the prevalence of sleep apnea has been noted to be as high as 16% among men and 5% among women between 30 and 65 years of age[6]. Five percent of adults have undiagnosed sleep apnea[7]. OSA is even more common among patients with cardiovascular disorders and is associated with multiple autonomic and metabolic derangements. Sleep apnea has been implicated in pathogenesis of multiple cardiovascular disorders including arrhythmias, hypertension, heart failure and stroke[4-9]. Its modifiable nature and high prevalence makes it a potential therapeutic target. In this article, we review and discuss the available data explaining the potential pathophysiological mechanisms linking OSA and AF, as well as the therapeutic and prognostic implications of the presence of OSA in AF patients.
OSA is characterized by episodes of nocturnal hypoxemia secondary to diminished and/or interrupted airflow during sleep. Apneic episodes are defined by complete cessation of airflow for ≥ 10 s, while hypopnea episodes are characterized by either ≥ 30% reduction in airflow and ≥ 4% reduction in blood oxygen saturation from baseline for at least 10 s or 50% reduction in air flow and ≥ 3% reduction in oxygen saturation from baseline for at least 10 s or arousal from sleep. It can be categorized as central (absence of inspiratory effort), obstructive (intermittent airway obstruction with preserved/increased respiratory efforts) or mixed sleep apnea (combination of central and OSA). Several easy to use questionnaires have been developed to screen patients for sleep apnea including the Epworth Sleepiness scale[10], the Berlin Questionnaire[11], the STOP and STOP-BANG Questionnaires[12]. Overnight polysomnography is the gold standard test to diagnose and stratify sleep apnea based on the apnea/hypopnea index (AHI)[13,14]. OSA is defined as five or more episodes of apnea and hypopnea per hour of sleep (AHI ≥ 5) and can be classified as mild (AHI 5-15), moderate (AHI 16-30), or severe (AHI > 30)[13,15].
Obesity, OSA and AF have a multifaceted relationship. Obesity increases risk of OSA and is also an independent risk factor for development of AF. The risk of AF increases by 4% for every one-unit increase in body mass index (BMI)[16-18]. This association is stronger for patients aged < 65 years[19]. Sleep apnea (both central and OSA) is more common in patients with congestive heart failure (CHF), and CHF itself is associated with high risk of AF[20-23]. Hence, several confounders must be taken into consideration while analyzing the multidimensional relationship between AF and OSA.
The first insight into a potential link between OSA and AF came from an observational study which reported episodes of AF seen on ambulatory electrocardiographic monitoring among 3% of subjects with OSA[24]. This association was supported by the complete resolution of paroxysmal AF episodes among those who were successfully treated for OSA[24]. Higher prevalence of cardiac arrhythmias among patients with OSA has been confirmed in subsequent studies[25]. The Sleep Heart Health Study reported four times higher prevalence of AF in patients with sleep apnea vs those without sleep apnea (4.8% vs 0.9%)[26]. High frequency paroxysmal AF and persistent AF are both associated with presence of OSA[27]. The episodes of AF and nonsustained ventricular tachycardia have been noted to be significantly higher during the night after apneic episodes, an observation that further supports the temporal association between AF and sleep apnea[28]. Sleep apnea is also an independent predictor for occurrence of postoperative AF among coronary artery bypass surgery patients. In a study by Mooe et al[29], the rate of postoperative AF was significantly higher (32% vs 18%) among patients with OSA (AHI ≥ 5) compared to those without OSA.
Obstructive sleep apnea is more prevalent among patients with AF than the general population. Gami et al[4] reported significantly higher prevalence (49% vs 32%) and a strong association (adjusted odds ratio of 2.19) between sleep apnea and AF in patients undergoing electrical cardioversion as compared patients without AF. This association was independent of age, sex, body mass index, hypertension and heart failure. High rates of sleep apnea are seen among patients with chronic persistent and permanent AF even after matching for age, sex and other relevant co morbid conditions[5]. The association between AF and sleep apnea may be underestimated, as most studies have reported a strong association between AF and sleep apnea despite using higher (AHI > 15) than standard (AHI > 5) threshold to diagnose OSA.
The association between AF and sleep apnea could be attributed to a higher prevalence of traditional risk factors for AF (especially obesity and hypertension) among OSA patients[30,31]. However, the association between AF and sleep apnea is found to be stronger than that of sleep apnea and traditional risk factors for AF[4]. OSA is more prevalent even among younger AF patients with normal left ventricular function[27]. This association remains statistically significant even after adjustment for covariates including hypertension, body mass index, and neck circumference. These findings highlight OSA as an independent risk factor for AF.
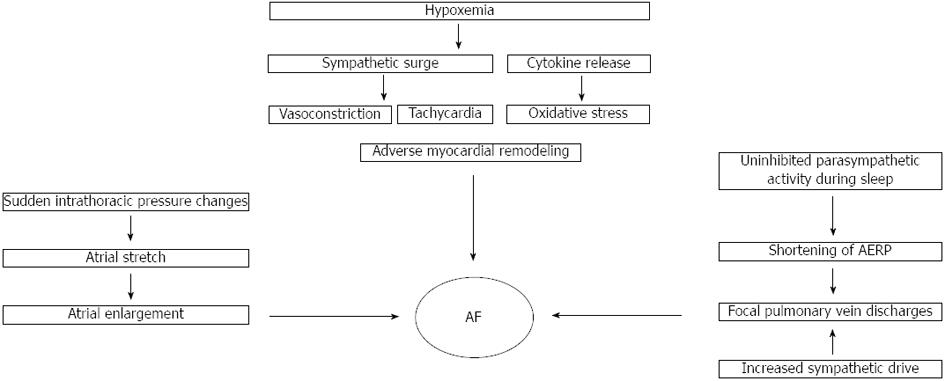
The suspected role of OSA in the pathogenesis of AF is based on sound physiological observations (Figure 1). OSA is characterized by repeated episodes of nocturnal hypoxemia. Intermittent hypoxemia causes mitochondrial dysfunction by altering redox state of cytochrome oxidase and results in repetitive oxidative stress[32,33]. Hypoxemic episodes induce transcription factors like nuclear factor kappa-B leading to increased production of inflammatory cytokines such as tumor necrosis factor α and interleukin 6. These cytokines, in concert with increased oxidative stress, lead to endothelial dysfunction, insulin resistance, hypercoagulability, and adverse myocardial remodeling[34-37].
Hypoxemic episodes induce sympathetic surges leading to vasoconstriction, hypertension and tachycardia[38,39], and ultimately increased myocardial oxygen demand. This increased stress on myocardium results in adverse myocardial remodeling, which is a substrate for cardiac arrhythmias[40,41].
Autonomic tone instability seen in OSA also contributes to pathogenesis of AF. Increases in parasympathetic and sympathetic tone are known to trigger AF[42]. During normal sleep afferent inputs from stretch receptors in lung tissue inhibit the paroxysmal parasympathetic discharges that occur during rapid eye movement sleep[43,44]. These receptors are activated due to lung expansion during normal ventilation. However, in apneic patients this response is attenuated due to pauses in breathing. Uninhibited paroxysmal parasympathetic discharges lead to marked paroxysmal bradycardia. Bradycardia is associated with decrease in atrial effective refractory period (AERP). The reduction in AERP promotes rapid electrical firing from atrial tissue in pulmonary vein ostia, thereby leading to AF[42,45,46]. Hypoxemia and hypercapnea associated with apneic episodes promote chronically heightened sympathetic activity[38,47,48]. Heightened sympathetic tone induces focal discharges from pulmonary veins, which have high concentration of adrenergic and vagal nerve endings[49-51]. Hypoxemia may exert an effect on cardiac arrhythmias that is independent and additive of sleep apnea. This hypothesis is supported by increased rates of ventricular ectopy among chronic obstructive pulmonary disease patients who have nocturnal hypoxemia without sleep apnea[52-54].
OSA is also associated with sudden and frequent changes in intrathoracic pressures, which are transmitted to thin walled atria and cause atrial stretch. Repetitive stretch may result in atrial enlargement and structural changes in pulmonary vein ostia, predisposing to development of AF[42,45].
AF patients with OSA respond poorly to both pharmacological and non-pharmacological therapy (cardioversion or ablation) with high rate of recurrence[55-58].
The rate of non-response to pharmacologic treatment increases with the increase in OSA severity[56]. Apneic patients have higher awake and nocturnal sympathetic tone, which may explain the suboptimal response to rate control strategy in AF patients with OSA[38]. Autonomic tone instability contributes to the genesis and propagation of AF in OSA. Acetylcholine-dependent potassium channels (IKACh) are thought to be one of the most relevant components by which vagal tone induces AERP shortening in the atrium[59]. Antiarrhythmic drugs such as amiodarone, which block acetylcholine-dependent activation of IKACh, along with beta-receptors and other potassium channels, could be superior in maintaining sinus rhythm over those antiarrhythmic drugs that do not block IKACh. However, studies showing superiority of amiodarone did not specifically address AF patients with sleep apnea. The clinical efficacy of such pharmacotherapy in patients with OSA needs to be investigated in future clinical trials[60].
Kanagala et al[58] followed 118 patients after direct current cardioversion (for AF/atrial flutter) and found that the presence of polysomnography-established OSA was associated with significantly higher rates of recurrent AF. Increased risk among patients with OSA was independent of age, sex, body mass index, hypertension, diabetes, echocardiographic parameters or antiarrhythmic therapy. Patients with OSA who were treated appropriately with continuous positive airway pressure (CPAP) had 82% lower rate of recurrence than patients who did not received treatment[58].
The presence of OSA is associated with a high rate of recurrent AF after ablation[61]. In a retrospective study, Jongnarangsin et al[62] reported presence of OSA as a strong predictor of AF recurrence after radiofrequency catheter ablation. This risk was independent of atrial size and body mass index. Chilukuri et al[63] reported high rates of recurrence after catheter ablation among patients who were classified as high risk for OSA on Berlin questionnaire. Tang et al[64] classified 178 patients into high risk and low risk for OSA depending on Berlin questionnaire and prospectively followed them for 11 mo after pulmonary vein isolation. They reported no statistically significant difference in the rate of AF recurrence among patients with different risk profiles for OSA at the end of the follow up period. These patients were classified in different risk categories for OSA based on Berlin questionnaire, but no confirmatory test was performed to establish diagnosis of OSA. Thus, misclassification bias cannot be excluded. Matiello et al[65] overcame this limitation; They prospectively followed 174 patients after circumferential pulmonary vein isolation and classified them as low or high risk for OSA on Berlin questionnaire. High-risk patients underwent a sleep study to diagnose OSA and classify its severity. OSA was an independent predictor for AF recurrence after ablation, and risk of recurrence increased with increasing severity of OSA. Naruse et al[66] prospectively studied 153 patients who underwent pulmonary vein isolation for drug refractory AF. The standard overnight polysomnographic evaluation was performed one week after ablation, and the total duration and the number of central or OSA or hypopnea episodes were examined. Of 153 patients, 116 patients were identified as having OSA. Eighty-two patients with OSA underwent CPAP therapy as 34 patients with OSA refused CPAP therapy. Data regarding the use of CPAP and recurrences of AF were obtained in all patients. During a mean follow-up period of 18.8 ± 10.3 mo, 51 (33%) patients experienced AF recurrences after ablation. A Cox regression analysis revealed that the left atrial volume (HR = 1.11; 95%CI: 1.01-1.23; P < 0.05), concomitant OSA (HR = 2.61; 95%CI: 1.12-6.09; P < 0.05), and usage of CPAP therapy (HR = 0.41; 95%CI: 0.22-0.76; P < 0.01) were associated with AF recurrences during the follow-up period.
Available evidence supports the role of effective OSA therapy in reducing the risk of AF recurrence[24,58]. The exact mechanism by which CPAP use improves success of AF therapies in OSA is not clear. The use of the CPAP may reduce the structural and electrical remodeling of the atria due to OSA, resulting in a lower AF recurrence rate. Serum markers of oxidative stress and free radical production predict AF recurrences after AF ablation[67]. CPAP therapy has been known to decrease oxidative stress in OSA[68,69]. An improvement in the oxidative stress by using CPAP could help attenuate the risk of recurrent AF.
However, currently available data is not robust, and supporting studies have small sample size and several limitations[24,58,62,66]. CPAP therapy is known to be associated with a reduction in preload. Its use in patients with systolic heart failure and AF may compromise diastolic ventricle filling, which is already compromised due to loss of organized atrial contraction[70]. Hence careful patient selection is warranted. Further data from prospective randomized control trials is needed before advocating widespread use of CPAP in patients with systolic heart failure and AF.
Several observational studies have indicated a high prevalence of OSA among patients with AF. Concomitant OSA is associated with poor response to treatment for AF. Limited data indicate that treatment of OSA results in a lower rate of AF recurrence. Patients with AF may be screened for OSA with a simple tool such as Berlin questionnaire, and high-risk patients should be considered for formal sleep study. The educational, behavioral and therapeutic interventions for sleep apnea should be offered to AF patients with OSA.
P- Reviewers Fazio S, Goldhammer E, Lehmann L, Sochman J, Trohman R, Yao YC S- Editor Huang XZ L- Editor A E- Editor Ma S
| 1. | Braunwald E. Shattuck lecture--cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med. 1997;337:1360-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 967] [Cited by in RCA: 917] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 2. | Wolf PA, Benjamin EJ, Belanger AJ, Kannel WB, Levy D, D’Agostino RB. Secular trends in the prevalence of atrial fibrillation: The Framingham Study. Am Heart J. 1996;131:790-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 285] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Calkins H, Brugada J, Packer DL, Cappato R, Chen SA, Crijns HJ, Damiano RJ, Davies DW, Haines DE, Haissaguerre M. HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation developed in partnership with the European Heart Rhythm Association (EHRA) and the European Cardiac Arrhythmia Society (ECAS); in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), and the Society of Thoracic Surgeons (STS). Endorsed and approved by the governing bodies of the American College of Cardiology, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, and the Heart Rhythm Society. Europace. 2007;9:335-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 520] [Cited by in RCA: 513] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 4. | Gami AS, Pressman G, Caples SM, Kanagala R, Gard JJ, Davison DE, Malouf JF, Ammash NM, Friedman PA, Somers VK. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 747] [Cited by in RCA: 776] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 5. | Braga B, Poyares D, Cintra F, Guilleminault C, Cirenza C, Horbach S, Macedo D, Silva R, Tufik S, De Paola AA. Sleep-disordered breathing and chronic atrial fibrillation. Sleep Med. 2009;10:212-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Bounhoure JP, Galinier M, Didier A, Leophonte P. Sleep apnea syndromes and cardiovascular disease. Bull Acad Natl Med. 2005;189:445-459; discussion 460-464. [PubMed] |
| 7. | Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2765] [Cited by in RCA: 2763] [Article Influence: 120.1] [Reference Citation Analysis (0)] |
| 8. | Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003;290:1906-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 812] [Cited by in RCA: 836] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 9. | Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52:686-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 597] [Cited by in RCA: 638] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 10. | Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540-545. [PubMed] |
| 11. | Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485-491. [PubMed] |
| 12. | Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaesth. 2010;57:423-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 373] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 13. | Practice parameters for the indications for polysomnography and related procedures. Polysomnography Task Force, American Sleep Disorders Association Standards of Practice Committee. Sleep. 1997;20:406-422. [PubMed] |
| 14. | Meoli AL, Casey KR, Clark RW, Coleman JA, Fayle RW, Troell RJ, Iber C. Hypopnea in sleep-disordered breathing in adults. Sleep. 2001;24:469-470. [PubMed] |
| 15. | Fleetham J, Ayas N, Bradley D, Ferguson K, Fitzpatrick M, George C, Hanly P, Hill F, Kimoff J, Kryger M. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J. 2006;13:387-392. [PubMed] |
| 16. | Dublin S, French B, Glazer NL, Wiggins KL, Lumley T, Psaty BM, Smith NL, Heckbert SR. Risk of new-onset atrial fibrillation in relation to body mass index. Arch Intern Med. 2006;166:2322-2328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 210] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 17. | Frost L, Hune LJ, Vestergaard P. Overweight and obesity as risk factors for atrial fibrillation or flutter: the Danish Diet, Cancer, and Health Study. Am J Med. 2005;118:489-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 330] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 18. | Wang TJ, Parise H, Levy D, D’Agostino RB, Wolf PA, Vasan RS, Benjamin EJ. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004;292:2471-2477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 973] [Cited by in RCA: 1047] [Article Influence: 49.9] [Reference Citation Analysis (0)] |
| 19. | Gami AS, Hodge DO, Herges RM, Olson EJ, Nykodym J, Kara T, Somers VK. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J Am Coll Cardiol. 2007;49:565-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 713] [Cited by in RCA: 776] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 20. | Larned JM, Raja Laskar S. Atrial fibrillation and heart failure. Congest Heart Fail. 2009;15:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Maisel WH, Stevenson LW. Atrial fibrillation in heart failure: epidemiology, pathophysiology, and rationale for therapy. Am J Cardiol. 2003;91:2D-8D. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 633] [Cited by in RCA: 717] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 22. | Cleland JG, Swedberg K, Follath F, Komajda M, Cohen-Solal A, Aguilar JC, Dietz R, Gavazzi A, Hobbs R, Korewicki J. The EuroHeart Failure survey programme-- a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur Heart J. 2003;24:442-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 963] [Cited by in RCA: 902] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 23. | Caldwell JC, Contractor H, Petkar S, Ali R, Clarke B, Garratt CJ, Neyses L, Mamas MA. Atrial fibrillation is under-recognized in chronic heart failure: insights from a heart failure cohort treated with cardiac resynchronization therapy. Europace. 2009;11:1295-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Guilleminault C, Connolly SJ, Winkle RA. Cardiac arrhythmia and conduction disturbances during sleep in 400 patients with sleep apnea syndrome. Am J Cardiol. 1983;52:490-494. [PubMed] |
| 25. | Hoffstein V, Mateika S. Cardiac arrhythmias, snoring, and sleep apnea. Chest. 1994;106:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 529] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 26. | Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, Sahadevan J, Redline S. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am J Respir Crit Care Med. 2006;173:910-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 873] [Cited by in RCA: 846] [Article Influence: 44.5] [Reference Citation Analysis (1)] |
| 27. | Stevenson IH, Teichtahl H, Cunnington D, Ciavarella S, Gordon I, Kalman JM. Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J. 2008;29:1662-1669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 169] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 28. | Monahan K, Storfer-Isser A, Mehra R, Shahar E, Mittleman M, Rottman J, Punjabi N, Sanders M, Quan SF, Resnick H. Triggering of nocturnal arrhythmias by sleep-disordered breathing events. J Am Coll Cardiol. 2009;54:1797-1804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 189] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 29. | Mooe T, Gullsby S, Rabben T, Eriksson P. Sleep-disordered breathing: a novel predictor of atrial fibrillation after coronary artery bypass surgery. Coron Artery Dis. 1996;7:475-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 122] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 30. | Porthan KM, Melin JH, Kupila JT, Venho KK, Partinen MM. Prevalence of sleep apnea syndrome in lone atrial fibrillation: a case-control study. Chest. 2004;125:879-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Wolk R, Kara T, Somers VK. Sleep-disordered breathing and cardiovascular disease. Circulation. 2003;108:9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 153] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 32. | McGown AD, Makker H, Elwell C, Al Rawi PG, Valipour A, Spiro SG. Measurement of changes in cytochrome oxidase redox state during obstructive sleep apnea using near-infrared spectroscopy. Sleep. 2003;26:710-716. [PubMed] |
| 33. | Peng Y, Yuan G, Overholt JL, Kumar GK, Prabhakar NR. Systemic and cellular responses to intermittent hypoxia: evidence for oxidative stress and mitochondrial dysfunction. Adv Exp Med Biol. 2003;536:559-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP. Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab. 1997;82:1313-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 178] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 35. | Lurie A. Endothelial dysfunction in adults with obstructive sleep apnea. Adv Cardiol. 2011;46:139-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 36. | Shamsuzzaman AS, Winnicki M, Lanfranchi P, Wolk R, Kara T, Accurso V, Somers VK. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation. 2002;105:2462-2464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 640] [Cited by in RCA: 645] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 37. | Vgontzas AN, Bixler EO, Chrousos GP. Metabolic disturbances in obesity versus sleep apnoea: the importance of visceral obesity and insulin resistance. J Intern Med. 2003;254:32-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 214] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 38. | Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96:1897-1904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1725] [Cited by in RCA: 1743] [Article Influence: 58.1] [Reference Citation Analysis (0)] |
| 39. | Tilkian AG, Guilleminault C, Schroeder JS, Lehrman KL, Simmons FB, Dement WC. Hemodynamics in sleep-induced apnea. Studies during wakefulness and sleep. Ann Intern Med. 1976;85:714-719. [PubMed] |
| 40. | Prabhakar NR. Sleep apneas: an oxidative stress. Am J Respir Crit Care Med. 2002;165:859-860. [PubMed] |
| 41. | Lévy P, Pépin JL, Arnaud C, Tamisier R, Borel JC, Dematteis M, Godin-Ribuot D, Ribuot C. Intermittent hypoxia and sleep-disordered breathing: current concepts and perspectives. Eur Respir J. 2008;32:1082-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 131] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 42. | Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:e257-e354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1263] [Cited by in RCA: 1385] [Article Influence: 72.9] [Reference Citation Analysis (0)] |
| 43. | Kara T, Narkiewicz K, Somers VK. Chemoreflexes--physiology and clinical implications. Acta Physiol Scand. 2003;177:377-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 247] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 44. | Cooper VL, Pearson SB, Bowker CM, Elliott MW, Hainsworth R. Interaction of chemoreceptor and baroreceptor reflexes by hypoxia and hypercapnia - a mechanism for promoting hypertension in obstructive sleep apnoea. J Physiol. 2005;568:677-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 110] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 45. | Caples SM, Somers VK. Sleep-disordered breathing and atrial fibrillation. Prog Cardiovasc Dis. 2009;51:411-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 46. | Chen LY, Shen WK. Epidemiology of atrial fibrillation: a current perspective. Heart Rhythm. 2007;4:S1-S6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 47. | Somers VK, Mark AL, Zavala DC, Abboud FM. Influence of ventilation and hypocapnia on sympathetic nerve responses to hypoxia in normal humans. J Appl Physiol. 1989;67:2095-2100. [PubMed] |
| 48. | Somers VK, Mark AL, Zavala DC, Abboud FM. Contrasting effects of hypoxia and hypercapnia on ventilation and sympathetic activity in humans. J Appl Physiol. 1989;67:2101-2106. [PubMed] |
| 49. | Tan AY, Zhou S, Ogawa M, Song J, Chu M, Li H, Fishbein MC, Lin SF, Chen LS, Chen PS. Neural mechanisms of paroxysmal atrial fibrillation and paroxysmal atrial tachycardia in ambulatory canines. Circulation. 2008;118:916-925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 268] [Cited by in RCA: 250] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 50. | Tan AY, Chen PS, Chen LS, Fishbein MC. Autonomic nerves in pulmonary veins. Heart Rhythm. 2007;4:S57-S60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 51. | Chen PS. Douglas P. Zipes Lecture. Neural mechanisms of atrial fibrillation. Heart Rhythm. 2006;3:1373-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 52. | Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006;48:e247-e346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 916] [Cited by in RCA: 883] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 53. | Flick MR, Block AJ. Nocturnal vs diurnal cardiac arrhythmias in patients with chronic obstructive pulmonary disease. Chest. 1979;75:8-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 75] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 54. | Douglas NJ. Nocturnal hypoxemia in patients with chronic obstructive pulmonary disease. Clin Chest Med. 1992;13:523-532. [PubMed] |
| 55. | Ng CY, Liu T, Shehata M, Stevens S, Chugh SS, Wang X. Meta-analysis of obstructive sleep apnea as predictor of atrial fibrillation recurrence after catheter ablation. Am J Cardiol. 2011;108:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 251] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 56. | Monahan K, Brewster J, Wang L, Parvez B, Goyal S, Roden DM, Darbar D. Relation of the severity of obstructive sleep apnea in response to anti-arrhythmic drugs in patients with atrial fibrillation or atrial flutter. Am J Cardiol. 2012;110:369-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 57. | Patel D, Mohanty P, Di Biase L, Shaheen M, Lewis WR, Quan K, Cummings JE, Wang P, Al-Ahmad A, Venkatraman P. Safety and efficacy of pulmonary vein antral isolation in patients with obstructive sleep apnea: the impact of continuous positive airway pressure. Circ Arrhythm Electrophysiol. 2010;3:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 176] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 58. | Kanagala R, Murali NS, Friedman PA, Ammash NM, Gersh BJ, Ballman KV, Shamsuzzaman AS, Somers VK. Obstructive sleep apnea and the recurrence of atrial fibrillation. Circulation. 2003;107:2589-2594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 662] [Cited by in RCA: 649] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 59. | Schotten U, Verheule S, Kirchhof P, Goette A. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev. 2011;91:265-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 797] [Cited by in RCA: 898] [Article Influence: 64.1] [Reference Citation Analysis (0)] |
| 60. | Singh BN, Singh SN, Reda DJ, Tang XC, Lopez B, Harris CL, Fletcher RD, Sharma SC, Atwood JE, Jacobson AK. Amiodarone versus sotalol for atrial fibrillation. N Engl J Med. 2005;352:1861-1872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 545] [Cited by in RCA: 500] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 61. | Hoyer FF, Lickfett LM, Mittmann-Braun E, Ruland C, Kreuz J, Pabst S, Schrickel J, Juergens U, Tasci S, Nickenig G. High prevalence of obstructive sleep apnea in patients with resistant paroxysmal atrial fibrillation after pulmonary vein isolation. J Interv Card Electrophysiol. 2010;29:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 62. | Jongnarangsin K, Chugh A, Good E, Mukerji S, Dey S, Crawford T, Sarrazin JF, Kuhne M, Chalfoun N, Wells D. Body mass index, obstructive sleep apnea, and outcomes of catheter ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2008;19:668-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 172] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 63. | Chilukuri K, Dalal D, Marine JE, Scherr D, Henrikson CA, Cheng A, Nazarian S, Spragg D, Berger R, Calkins H. Predictive value of obstructive sleep apnoea assessed by the Berlin Questionnaire for outcomes after the catheter ablation of atrial fibrillation. Europace. 2009;11:896-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 64. | Tang RB, Dong JZ, Liu XP, Kang JP, Ding SF, Wang L, Long DY, Yu RH, Liu XH, Liu S. Obstructive sleep apnoea risk profile and the risk of recurrence of atrial fibrillation after catheter ablation. Europace. 2009;11:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 65. | Matiello M, Nadal M, Tamborero D, Berruezo A, Montserrat J, Embid C, Rios J, Villacastín J, Brugada J, Mont L. Low efficacy of atrial fibrillation ablation in severe obstructive sleep apnoea patients. Europace. 2010;12:1084-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 116] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 66. | Naruse Y, Tada H, Satoh M, Yanagihara M, Tsuneoka H, Hirata Y, Ito Y, Kuroki K, Machino T, Yamasaki H. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm. 2013;10:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 195] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 67. | Shimano M, Shibata R, Inden Y, Yoshida N, Uchikawa T, Tsuji Y, Murohara T. Reactive oxidative metabolites are associated with atrial conduction disturbance in patients with atrial fibrillation. Heart Rhythm. 2009;6:935-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 68. | Murri M, García-Delgado R, Alcázar-Ramírez J, Fernández de Rota L, Fernández-Ramos A, Cardona F, Tinahones FJ. Continuous positive airway pressure therapy reduces oxidative stress markers and blood pressure in sleep apnea-hypopnea syndrome patients. Biol Trace Elem Res. 2011;143:1289-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 69. | Murri M, García-Delgado R, Alcázar-Ramírez J, Fernández-Ramos A, Alcaide J, Cardona F, Tinahones FJ. Effect of CPAP on oxidative stress and circulating progenitor cell levels in sleep patients with apnea-hypopnea syndrome. Respir Care. 2011;56:1830-1836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 70. | Kiely JL, Deegan P, Buckley A, Shiels P, Maurer B, McNicholas WT. Efficacy of nasal continuous positive airway pressure therapy in chronic heart failure: importance of underlying cardiac rhythm. Thorax. 1998;53:957-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |