Published online Aug 26, 2025. doi: 10.4330/wjc.v17.i8.110366
Revised: June 20, 2025
Accepted: July 22, 2025
Published online: August 26, 2025
Processing time: 77 Days and 14.8 Hours
Pheochromocytoma, a rare catecholamine-secreting tumor, typically presents with the classic triad of headache, palpitations, and diaphoresis, often accompanied by cardiovascular manifestations. While vomiting occurs in approximately 34.5% of cases, it is rarely the predominant and persistent presenting symptom. Pheochro
A 53-year-old female presented predominantly with persistent and refractory vomiting as her chief complaint, accompanied by signs of acute heart failure [left ventricular ejection fraction (LVEF) 30%]. Initial evaluation at a primary hospital, including coronary angiography (revealing only mild stenosis), led to a misdiagnosis of coronary artery disease. Despite standard anti-thrombotic, anti-heart failure, and anti-emetic therapy, her vomiting persisted and heart failure did not resolve. Subsequent hospitalization revealed dramatic paroxysmal hypertension (202/129 mmHg to 97/51 mmHg) and fever. Significantly elevated plasma meta
This case highlights a highly atypical presentation of pheochromocytoma domi
Core Tip: This case highlights an exceptionally atypical presentation of pheochromocytoma dominated by refractory vomiting and complicated by acute catecholamine-induced cardiomyopathy with heart failure (left ventricular ejection fraction 30%). Initial misdiagnosis as coronary artery disease occurred due to mild stenosis on angiography. The critical diagnostic clue emerged with dramatic paroxysmal hypertension (fluctuating from 202/129 mmHg to 97/51 mmHg). This report underscores that pheochromocytoma must be considered in patients with unexplained treatment-resistant vomiting coexisting with acute heart failure, particularly when labile hypertension appears. Timely biochemical screening (catecholamine metabolites) and adrenal imaging are essential to prevent life-threatening delays.
- Citation: Cheng H, Gu LT, Yang J. Pheochromocytoma presenting with vomiting and heart failure: A case report. World J Cardiol 2025; 17(8): 110366
- URL: https://www.wjgnet.com/1949-8462/full/v17/i8/110366.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i8.110366
Pheochromocytoma is a rare endocrine tumor originating in the chromaffin tissue of the neuroectoderm. Its secreted catecholamine can cause persistent or paroxysmal hypertension, multiple organ dysfunctions and metabolic disorders. The most common symptoms include a triad of headache, palpitations and diaphoresis.
While nausea and vomiting symptoms occur in 34.5% of cases[1], these are rarely the dominant and most persistent presenting symptoms, as observed in this patient. This atypical presentation can lead to diagnostic challenges and delays, and is associated with higher mortality[1]. Furthermore, the concomitant presentation of acute heart failure at admission significantly deviates from the classic triad, which may be associated with elevated catecholamine levels[2]. This unusual combination of symptoms, where refractory vomiting dominates the clinical presentation alongside acute heart failure, presents a significant diagnostic challenge and often leads to delayed recognition. Given the high misdiagnosis rate of pheochromocytoma-related hypertension and digestive symptoms, it is crucial to combine imaging and blood pressure monitoring to better analyze clinical symptoms and guide treatment.
Recurrent chest tightness accompanied by nausea and vomiting for 9 days.
A 53-year-old female presented to the emergency department with recurrent chest tightness, nausea, and vomiting lasting 9 days, representing her second hospitalization for these symptoms. Ten days previously, emotional distress due to family changes precipitated sudden nausea, vomiting, chest tightness, and diarrhea, prompting evaluation at a primary hospital. Initial testing revealed elevated B-type natriuretic peptide (BNP) and troponin, electrocardiography (ECG) showed sinus rhythm with ST-T changes, and coronary angiography identified 30% stenosis with mild thrombus in the mid-left anterior descending artery. She was discharged on anti-thrombotic and gastric-protective therapy but expe
Upon admission, echocardiography demonstrated uncoordinated left ventricular wall motion, severely reduced systo
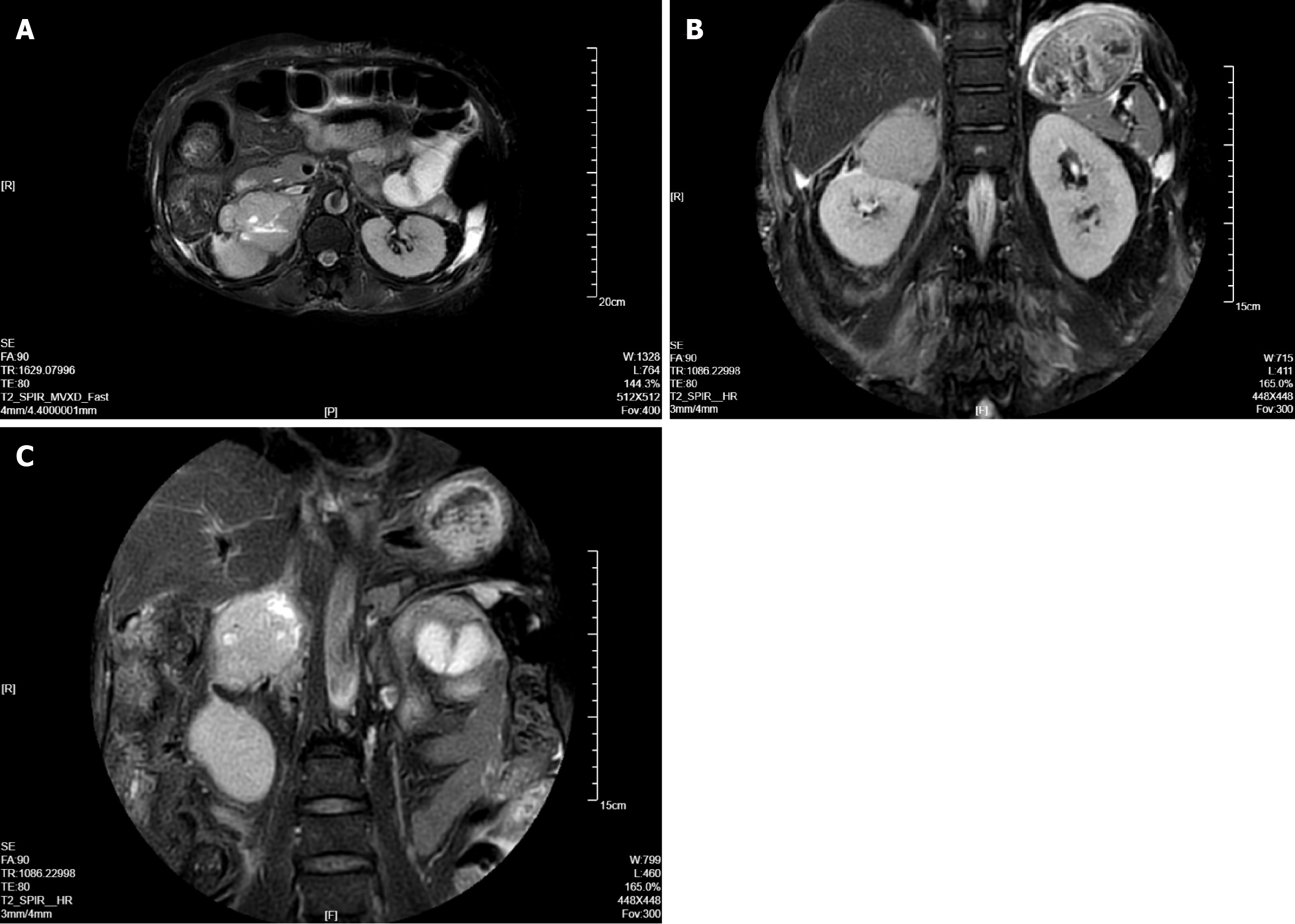
This combination of refractory cardiac and gastrointestinal symptoms that were more severe than expected given the mild coronary disease, along with extreme hemodynamic lability and unexplained fever, raised suspicion for catecholamine excess. Biochemical testing confirmed profound elevations in catecholamine. Abdominal CT revealed a right adrenal mass, subsequently confirmed as pheochromocytoma by adrenal magnetic resonance imaging (MRI), establishing the definitive etiology of her presentation.
The patient's history of past illness also indicated that she was diagnosed with diabetes mellitus 1 year ago and has been controlling her blood sugar through oral metformin, 2 tablets twice daily.
The patient denies any family history of genetic diseases or similar conditions.
On admission, physical examination revealed a temperature of 37°C, pulse rate of 89 bpm, respiratory rate of 14 breaths per minute, and blood pressure of 122/74 mmHg. Cardiac examination showed a normally positioned heart with the apex beat palpable 0.5 cm medial to the left midclavicular line in the fifth intercostal space; heart sounds were regular at 89 bpm with normal S1 and S2 intensity, absent murmurs or extra sounds. Abdominal assessment demonstrated a flat, non-tender abdomen without palpable masses or hepatosplenomegaly. However, during hospitalization, she developed dramatic hemodynamic instability characterized by paroxysmal hypertension with extreme diurnal fluctuations (e.g., 202/129 mmHg to 97/51 mmHg) and nocturnal excursions (201/115 mmHg to 121/56 mmHg), accompanied by inter
Initial testing at the primary hospital revealed elevated serum BNP and troponin. Upon admission to our hospital, plasma biomarkers confirmed significant cardiac stress, including troponin (192.2 pg/mL), myoglobin (320.0 ng/mL), and mar
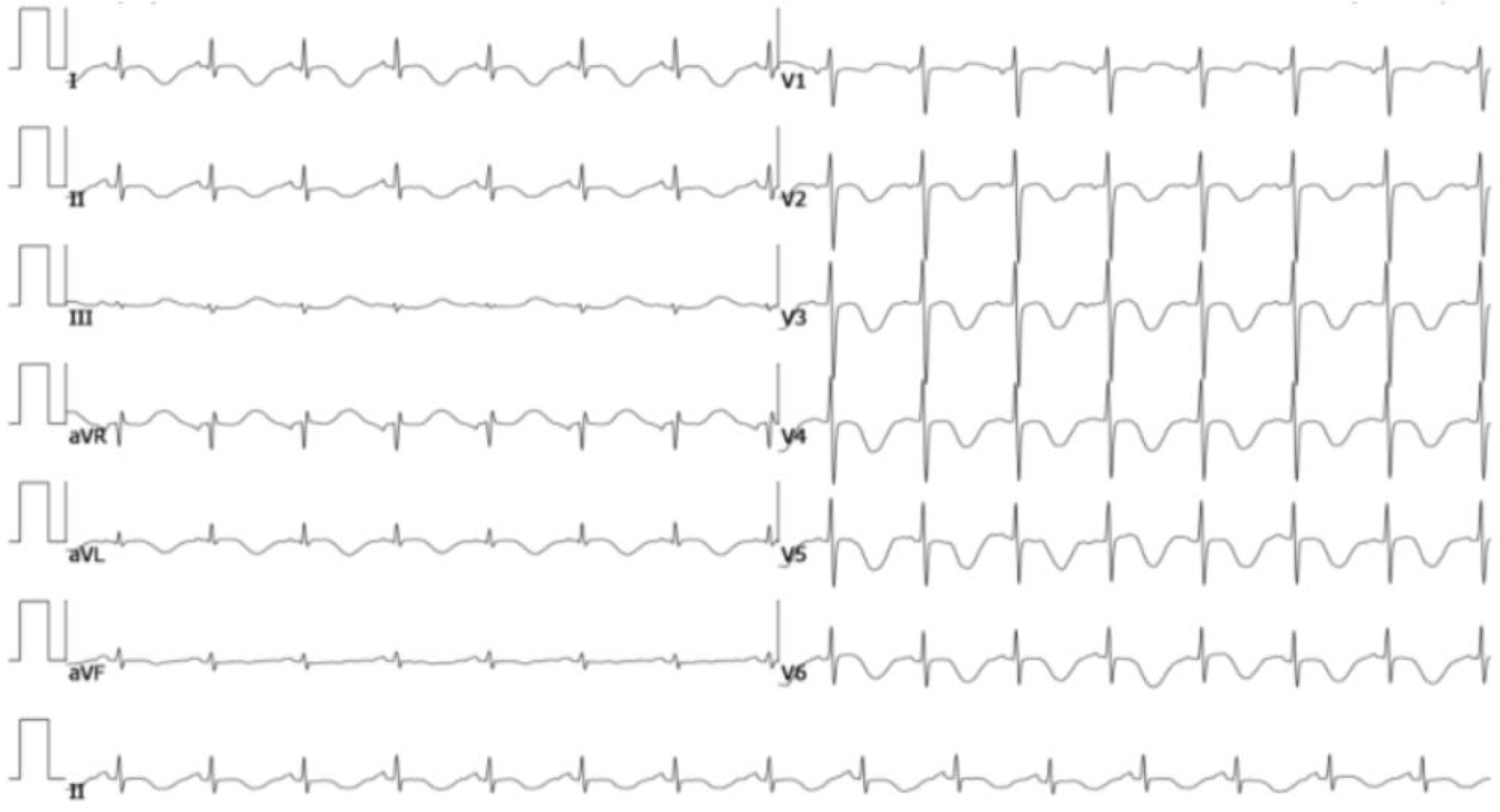
At the primary hospital, an initial ECG showed sinus rhythm with ST-T changes. Coronary angiography identified mild disease with 30% stenosis and a thrombus shadow in the near-middle left anterior descending artery; no significant stenosis was noted in other coronary vessels. Upon transfer to our institution, emergency department ECG revealed sinus tachycardia (137 bpm; Figure 1). Echocardiography demonstrated uncoordinated left ventricular wall motion, severely reduced systolic function (ejection fraction 30%), moderate tricuspid regurgitation, and hypovolemia. A head CT ruled out intracranial causes of vomiting, showing no abnormalities. Subsequent abdominal CT revealed a mixed-density mass in the right adrenal region (Figure 2), while chest CT incidentally noted two pulmonary nodules and tracheal diverticula. Adrenal MRI confirmed a right adrenal pheochromocytoma (Figure 3).
We did not consult a multidisciplinary team.
The patient was finally diagnosed with: (1) Class III heart function [New York Heart Association (NYHA) classification]; (2) Pheochromocytoma-induced hypertension; (3) Coronary atherosclerosis; and (4) Type 2 diabetes mellitus.
The patient decided to return home for surgical treatment at a local hospital.
A significant limitation of this case report is the absence of follow-up data. After diagnosis was confirmed, the patient opted for surgical management at their hometown hospital and was subsequently lost to our follow-up. This precludes assessment of critical outcomes such as the resolution of cardiomyopathy, normalization of hemodynamics, cessation of vomiting, confirmation of complete tumor resection, and long-term biochemical remission or genetic testing results. The absence of this information limits our understanding of the full clinical trajectory and recovery potential following pheochromocytoma removal in this complex presentation.
This case exemplifies the significant diagnostic challenges of pheochromocytoma, particularly when presenting with atypical features dominating the clinical picture. While the tumor's adrenal location and final diagnosis via imaging and biochemistry were typical, the patient's initial and persistent presentation centered on refractory vomiting and profound acute heart failure [left ventricular ejection fraction (LVEF) 30%]. This was quite different from the classic signs of headache, palpitations and diaphoresis. This divergence led to considerable diagnostic delay and initial misdiagnosis.
Understandably, the focus at the primary hospital was on the prominent gastrointestinal symptoms and acute cardiac dysfunction. The finding of mild coronary stenosis on angiography further anchored the diagnosis towards ischemic heart disease. However, the patient's persistent vomiting and inadequate improvement in cardiac function despite appropriate conventional therapy for heart failure, potential ischemia, and nausea created a critical diagnostic impasse. Common gastrointestinal and neurological causes for vomiting were reasonably excluded, yet the etiology remained elusive. The pivotal diagnostic turning point was the emergence of dramatic, paroxysmal hypertension with extreme fluctuations (202/129 mmHg to 97/51 mmHg) and unexplained fever. This profound hemodynamic lability, highly unusual in common gastrointestinal disorders or uncomplicated heart failure, strongly suggested unregulated catechola
While vomiting occurs in approximately one-third of pheochromocytoma cases[1], it is rarely the dominant and most persistent presenting symptom, as in this patient. The process of vomiting is controlled by a balance between the gastrointestinal enteric nervous system and the central nervous system. The pathogenesis of vomiting in pheochromocytoma is likely multifactorial, involving direct effects of catecholamines (particularly dopamine) on receptors in the brainstem and gastrointestinal tract, disrupting the emetic control pathways[3,4]. More critically, the presence of vomi
Similarly, acute heart failure in this context is a serious complication directly attributable to catecholamine excess. High levels of catecholamines cause coronary vasospasm, myocardial stunning, increased oxygen demand, and direct toxic effects on cardiomyocytes, leading to catecholamine-induced cardiomyopathy and acute heart failure[5-7]. It has been found that a fairly complex network of Ca2+ overload, oxidative stress, mitochondrial dysfunction, apoptosis, interstitial fibrosis, hypertrophy, and inflammation underlies catecholamine-induced cardiotoxicity[5]. The co-occurrence of refractory vomiting and acute heart failure, especially when accompanied by hemodynamic instability, should strongly raise the possibility of an underlying catecholamine-secreting tumor like pheochromocytoma.
Pheochromocytoma is most common in people aged 20-50 years, and there is no significant difference in incidence between men and women. Among the clinical symptoms, the main manifestations of the cardiovascular system include paroxysmal hypertension, hypotension and shock, and catecholamine cardiomyopathy. Among them, hypertension is divided into two types: Paroxysmal and persistent, and persistent people can also have paroxysmal intensification[8]. Large retrospective case studies have detailed the prevalence of hypertension between 51% and 90% in pheochromocytoma patients[9,10]. Therefore, paroxysmal hypertension in this case has a good diagnostic role, which is also one of the breakthrough points in the diagnosis of this case. Additionally, pheochromocytoma can cause metabolic disturbances (e.g., glucose, lipid, electrolyte)[11,12] and other systemic effects like gastrointestinal issues, renal failure, abdominal mass, reduced blood volume, and leukocytosis[13-15].
Many patients have paroxysmal symptoms prior to diagnosis, suggesting excessive catecholamine release. Catecho
While previous case reports have documented pheochromocytoma presenting with vomiting or cardiomyopathy individually, the constellation of refractory vomiting as the dominant symptom, severe acute heart failure, and extreme hemodynamic lability in this case is exceptionally rare. For instance, Amina Abid reported a normotensive pheochromocytoma case initially presenting with abdominal pain and vomiting, but without cardiac involvement, which was later linked to neck swelling and medullary thyroid cancer[17]. Conversely, Pirbhat Shams described a 42-year-old woman who presented with heart failure and was found to have pheochromocytoma-induced Takotsubo-like cardiomyopathy[18]. Chen et al[19] reported a 21-year-old male with no hypertensive history who presented with congestive heart failure due to pheochromocytoma-related cardiomyopathy, and hypertension was detected at follow-up. Neither of these cases featured prominent gastrointestinal symptoms. Our case uniquely combines gastrointestinal and cardiac features, further complicated by delayed diagnosis due to initial misattribution to coronary disease. This highlights the need for heigh
In short, although the symptoms of patients are different, related symptoms have a certain suggestive role. Survey data shows that 21.2% of patients have the classic triad of headache, sweating and palpitations, 33.9% have one or two classic symptoms, and 12.7% have other paroxysmal symptoms[20]. Significant blood pressure fluctuations strongly suggest catecholamine excess, and 24 hour ambulatory blood pressure monitoring can assist in diagnosis. The core diagnostic approach combines recognition of suggestive symptoms with biochemical testing and imaging. The distinctiveness of our case lies in the patient presenting predominantly with refractory vomiting and acute heart failure, ultimately traced to pheochromocytoma. Therefore, pheochromocytoma warrants consideration in patients presenting concurrently with heart failure and unexplained vomiting. Advances in imaging (CT, MRI, abdominal ultrasound) continue to improve detection rates. Given its rarity and diverse symptom constellation, clinicians must remain vigilant for characteristic signs to facilitate timely diagnosis.
Pheochromocytoma is a rare catecholamine-secreting tumor capable of inducing multi-system dysfunction through catecholamine excess. This case exemplifies a highly atypical presentation dominated by refractory vomiting and acute heart failure, compounded by significant diagnostic delay. Accurate diagnosis relies on identifying key characteristic clues, especially labile hypertension, amidst non-specific symptoms, and is supported by targeted biochemical testing and adrenal imaging. Crucially, it underscores that pheochromocytoma must be considered in patients with unexplained vomiting and concurrent heart failure, especially when hypertension fluctuates dramatically. Timely diagnosis is impera
The authors would like to express their gratitude to the patient for granting permission to publish this case report.
| 1. | Ando Y, Ono Y, Sano A, Fujita N, Ono S, Tanaka Y. Clinical characteristics and outcomes of pheochromocytoma crisis: a literature review of 200 cases. J Endocrinol Invest. 2022;45:2313-2328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 2. | Cornu E, Motiejunaite J, Belmihoub I, Vidal-Petiot E, Mirabel M, Amar L. Acute Stress Cardiomyopathy: Heart of pheochromocytoma. Ann Endocrinol (Paris). 2021;82:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Cai QQ, Zheng LF, Fan RF, Lian H, Zhou L, Song HY, Tang YY, Feng XY, Guo ZK, Wang ZY, Zhu JX. Distribution of dopamine receptors D1- and D2-immunoreactive neurons in the dorsal motor nucleus of vagus in rats. Auton Neurosci. 2013;176:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Belkacemi L, Darmani NA. Dopamine receptors in emesis: Molecular mechanisms and potential therapeutic function. Pharmacol Res. 2020;161:105124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Du Y, Demillard LJ, Ren J. Catecholamine-induced cardiotoxicity: A critical element in the pathophysiology of stroke-induced heart injury. Life Sci. 2021;287:120106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Hašková P, Jansová H, Bureš J, Macháček M, Jirkovská A, Franz KJ, Kovaříková P, Šimůnek T. Cardioprotective effects of iron chelator HAPI and ROS-activated boronate prochelator BHAPI against catecholamine-induced oxidative cellular injury. Toxicology. 2016;371:17-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Yang J, Wang Z, Chen DL. Shikonin ameliorates isoproterenol (ISO)-induced myocardial damage through suppressing fibrosis, inflammation, apoptosis and ER stress. Biomed Pharmacother. 2017;93:1343-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 75] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Gunawardane PTK, Grossman A. Phaeochromocytoma and Paraganglioma. Adv Exp Med Biol. 2017;956:239-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Guerrero MA, Schreinemakers JM, Vriens MR, Suh I, Hwang J, Shen WT, Gosnell J, Clark OH, Duh QY. Clinical spectrum of pheochromocytoma. J Am Coll Surg. 2009;209:727-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Baguet JP, Hammer L, Mazzuco TL, Chabre O, Mallion JM, Sturm N, Chaffanjon P. Circumstances of discovery of phaeochromocytoma: a retrospective study of 41 consecutive patients. Eur J Endocrinol. 2004;150:681-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 129] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 11. | Mercado-Asis LB, Wolf KI, Jochmanova I, Taïeb D. PHEOCHROMOCYTOMA: A GENETIC AND DIAGNOSTIC UPDATE. Endocr Pract. 2018;24:78-90. [PubMed] [DOI] [Full Text] |
| 12. | Farrugia FA, Charalampopoulos A. Pheochromocytoma. Endocr Regul. 2019;53:191-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 72] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 13. | Scholten A, Cisco RM, Vriens MR, Cohen JK, Mitmaker EJ, Liu C, Tyrrell JB, Shen WT, Duh QY. Pheochromocytoma crisis is not a surgical emergency. J Clin Endocrinol Metab. 2013;98:581-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 14. | Tschuor C, Sadri H, Clavien PA. Pheochromocytoma crisis. Clin Case Rep. 2014;2:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Mannelli M, Ianni L, Cilotti A, Conti A. Pheochromocytoma in Italy: a multicentric retrospective study. Eur J Endocrinol. 1999;141:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 131] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Farrugia FA, Martikos G, Tzanetis P, Charalampopoulos A, Misiakos E, Zavras N, Sotiropoulos D. Pheochromocytoma, diagnosis and treatment: Review of the literature. Endocr Regul. 2017;51:168-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 17. | Abid A, Siddiqi AI, Shafiq W, Irfan H. A Normotensive Case of Pheochromocytoma With Unusual Presentation of Abdominal Pain. Cureus. 2023;15:e47063. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Shams P, Ahmed I, Siddique S, Abbas F, Khan AH. Takotsubo Like Cardiomyopathy with Concomitant Pheochromocytoma: A Rare Presentation. J Coll Physicians Surg Pak. 2022;32:1483-1485. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Chen S, Chen Y, Chen P. Pheochromocytoma-induced congestive heart failure and hypertension in a 21- year-old man-a Case Report. J Pak Med Assoc. 2024;74:1905-1908. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Ebbehoj A, Stochholm K, Jacobsen SF, Trolle C, Jepsen P, Robaczyk MG, Rasmussen ÅK, Feldt-Rasmussen U, Thomsen RW, Søndergaard E, Poulsen PL. Incidence and Clinical Presentation of Pheochromocytoma and Sympathetic Paraganglioma: A Population-based Study. J Clin Endocrinol Metab. 2021;106:e2251-e2261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |