Published online Mar 26, 2024. doi: 10.4330/wjc.v16.i3.118
Peer-review started: December 22, 2023
First decision: January 17, 2024
Revised: January 19, 2024
Accepted: February 20, 2024
Article in press: February 20, 2024
Published online: March 26, 2024
Processing time: 89 Days and 17.8 Hours
Thoracic ultrasound has attracted much interest in detecting pleural effusion or pulmonary consolidation after cardiac surgery. In 2016, Trovato reported, in the World Journal of Cardiology, the interest of using, in addition to echocardiography, thoracic ultrasound. In this editorial, we highlight the value of assessing diaphragm function after cardiac surgery and interventional cardiology pro
Core Tip: Diaphragm dysfunction can be secondary to cardiac surgery or atrial fibrillation ablation via phrenic nerve injury. In patients with comorbidities such as obesity and cardiac or respiratory diseases, unilateral diaphragm paralysis may be poorly tolerated. Diaphragm ultrasound is the most appropriate tool for early diagnosis.
- Citation: Boussuges M, Blanc P, Bregeon F, Boussuges A. Interest of thoracic ultrasound after cardiac surgery or interventional cardiology. World J Cardiol 2024; 16(3): 118-125
- URL: https://www.wjgnet.com/1949-8462/full/v16/i3/118.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i3.118
The diaphragm is the main inspiratory muscle and contributes to 60%-70% of the total ventilation at rest. It is a musculotendinous structure (2-4 mm) with a central tendinous portion and a peripheral muscular portion. It includes two hemidiaphragms: The right with a dome positioned higher than the left. Motor innervation of the diaphragm comes from two phrenic nerves formed from the C3-C5 nerve roots. The left and right phrenic nerves cross the neck and thorax between the mediastinal surface of the parietal pleura and the fibrous pericardium to reach the corresponding hemidiaphragm. The left phrenic nerve is close to the subclavian artery and passes in front of the pericardial sac of the left ventricle. The right phrenic nerve runs superficial to the anterior scalene muscle and right subclavian artery and passes over the right atrium and right ventricle. Arterial blood flow to the diaphragm comes from collaterals of the internal mammary artery, collaterals of the abdominal aorta, and vessels originating from intercostal arteries. During contraction, the diaphragm shortens and moves caudally, leading to an expansion of the thoracic cavity. This phenomenon increases abdominal pressure and decreases alveolar pressure below atmospheric pressure resulting in airflow into the lungs[1]. Various procedures used in patients with heart diseases can impair diaphragmatic function. Diaphragm dysfunction was exceptionally reported after central vein cannulation and pacemaker battery change[2,3]. In contrast, this was regularly observed after cardiac surgery and atrial fibrillation ablation[4,5]. We underline in this editorial the interest of assessing diaphragm function after such procedures.
Impaired diaphragmatic function was reported in a significant percentage of patients after cardiac surgery. Depending on the detection method and the delay from the surgery, diaphragm dysfunction has been variously estimated: 21% for Dimopoulou et al[6], 38% for Bruni et al[7], 46% for DeVita et al[8], and 75% for Moury et al[9]. In a recent observational study[10], symptomatic diaphragm dysfunction was found in 272 out of 3577 patients (7.6%). In our experience (unpublished study), the percentage of diaphragm dysfunction in patients admitted in a cardiac rehabilitation center after cardiac surgery was 15% (39 out of 264 patients). Diaphragm ultrasound detected weakness in 10% of cases and hemidiaphragm paralysis in 5%. Various mechanisms may explain diaphragm dysfunction in these patients. Diaphragmatic motion may be reduced by chest pain secondary to sternotomy, pleural effusion or impaired muscle function[11]. Furthermore, phrenic nerve damage is a well-known, complication of cardiac surgery. It has been shown that the phrenic nerve can be injured through thermal lesions secondary to topical cardiac cooling with ice-cold solution in the pericardium. To reduce the risk of injury, the use of insulation pads placed between the heart and the left pericardium has been proposed to protect the phrenic nerve from hypothermic surgery[12,13]. The use of warm-blood cardioplegia has also demonstrated its interest in reducing the risk of diaphragm paralysis[14]. However, other mechanisms may explain phrenic nerve damage during cardiac surgery. During coronary artery bypass grafting, phrenic nerve injury may be secondary to direct surgical trauma during dissection of the internal mammary artery (IMA) or indirect injury due to stretching by the sternal retractor[15]. In addition, IMA harvesting may result in decreased blood flow to the phrenic nerve through ligation of some branches such as the pericardiacophrenic artery. These mechanisms could explain the increased risk of phrenic nerve dysfunction in patiens who underwent IMA harvesting compared to the group that did not undergo IMA harvesting[16]. Inflammation secondary to cardiopulmonary bypass surgery may also be involved in the development of diaphragm dysfunction via significant production of reactive oxygen species and proinflammatory and pro-apoptotic signaling pathways activation[17].
Minimally invasive treatment of atrial fibrillation appeared in the late 1990s and is now widely used as a safe alternative to antiarrhythmic drugs. Procedures have improved while the number of patients eligible for such treatments has increased.
The most commonly used fibrillation ablation techniques are thermal energy sources with cold (cryoablation around -55°C) or heat (radiofrequency heating around +55°C). Due to the short distance between the ablation site and the phrenic nerve, thermal injury is not uncommon (mainly on the right side) resulting in diaphragmatic dysfunction. Electro
Chest ultrasound has gained much interest in detecting pleural effusion and pulmonary consolidation or edema after cardiac surgery. In 2016, Trovato[23] reported, in the World Journal of Cardiology, the interest of using, in addition to echocardiography, thoracic ultrasound for cardiologists. Since the frequency of diaphragm dysfunction is significant after cardiac surgery and atrial fibrillation ablation, the ultrasound analysis of diaphragm function is important.
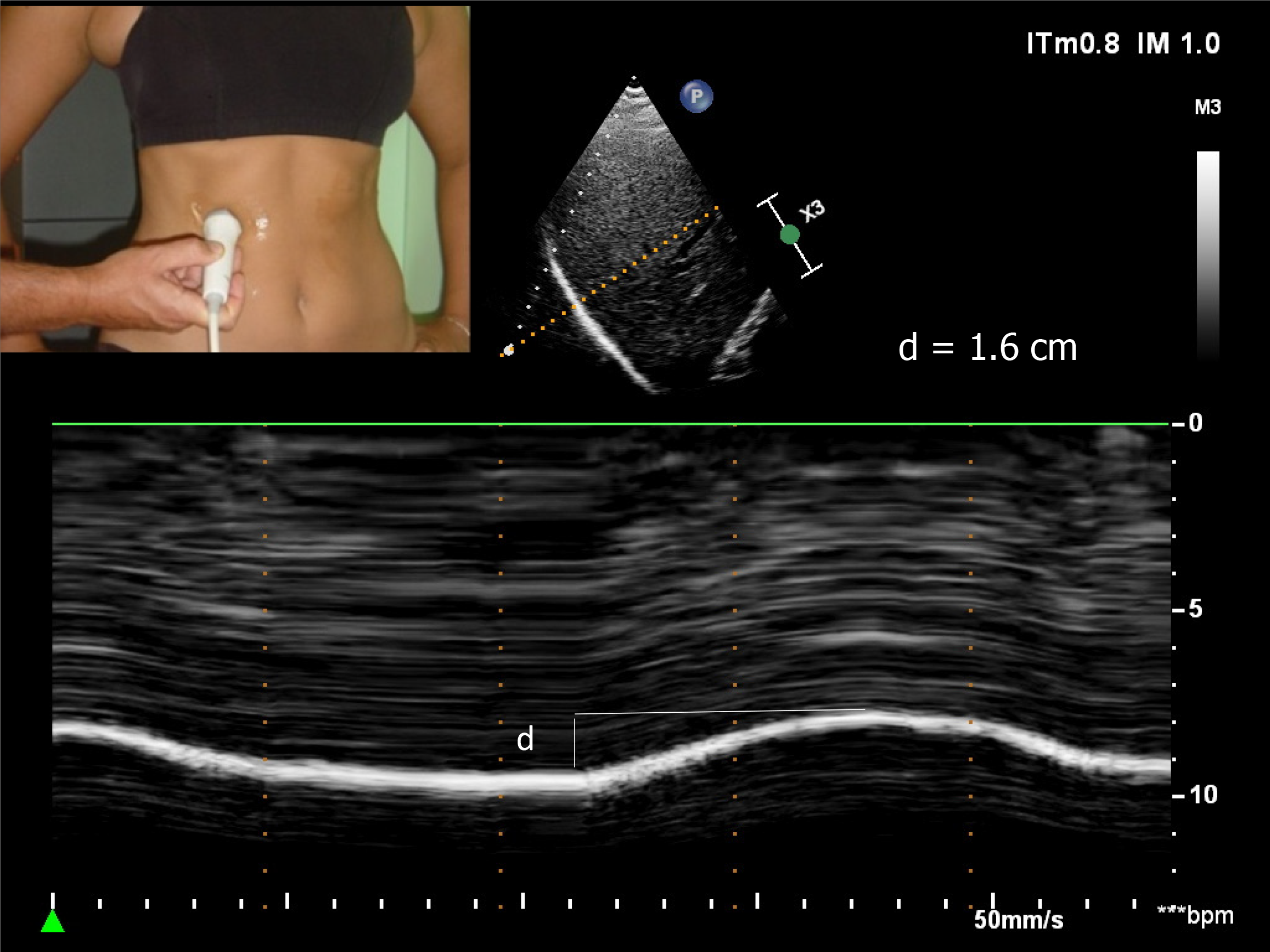
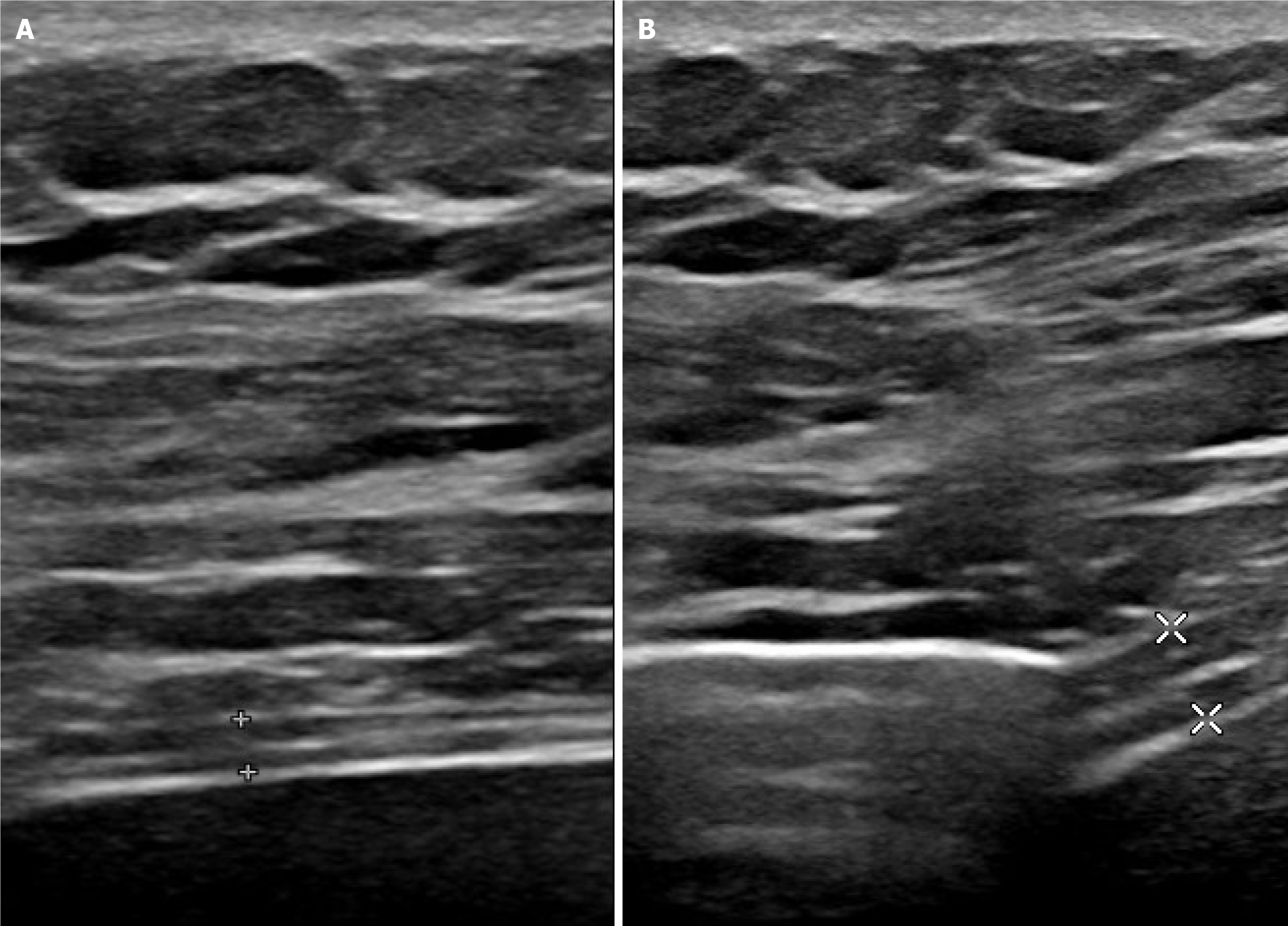
The two hemidiaphragms can be studied by two complementary ultrasound methods. Diaphragm mobility can be recorded by a sub-costal approach using a cardiac probe[24-26]. Excursions of both hemidiaphragms are measured by M-mode ultrasonography during various volitional maneuvers such as quiet breathing (Figure 1) voluntary sniffing and deep inspiration. In addition, it is useful to measure the thickness changes at the zone of apposition during breathing (Figure 2, Video) by a superficial probe using B-mode[27]. The percentage of thickening during inspiration provides important information about the quality of the muscle function of the diaphragm[28]. These two approaches make it possible to detect paralysis or weakness of hemidiaphragm.
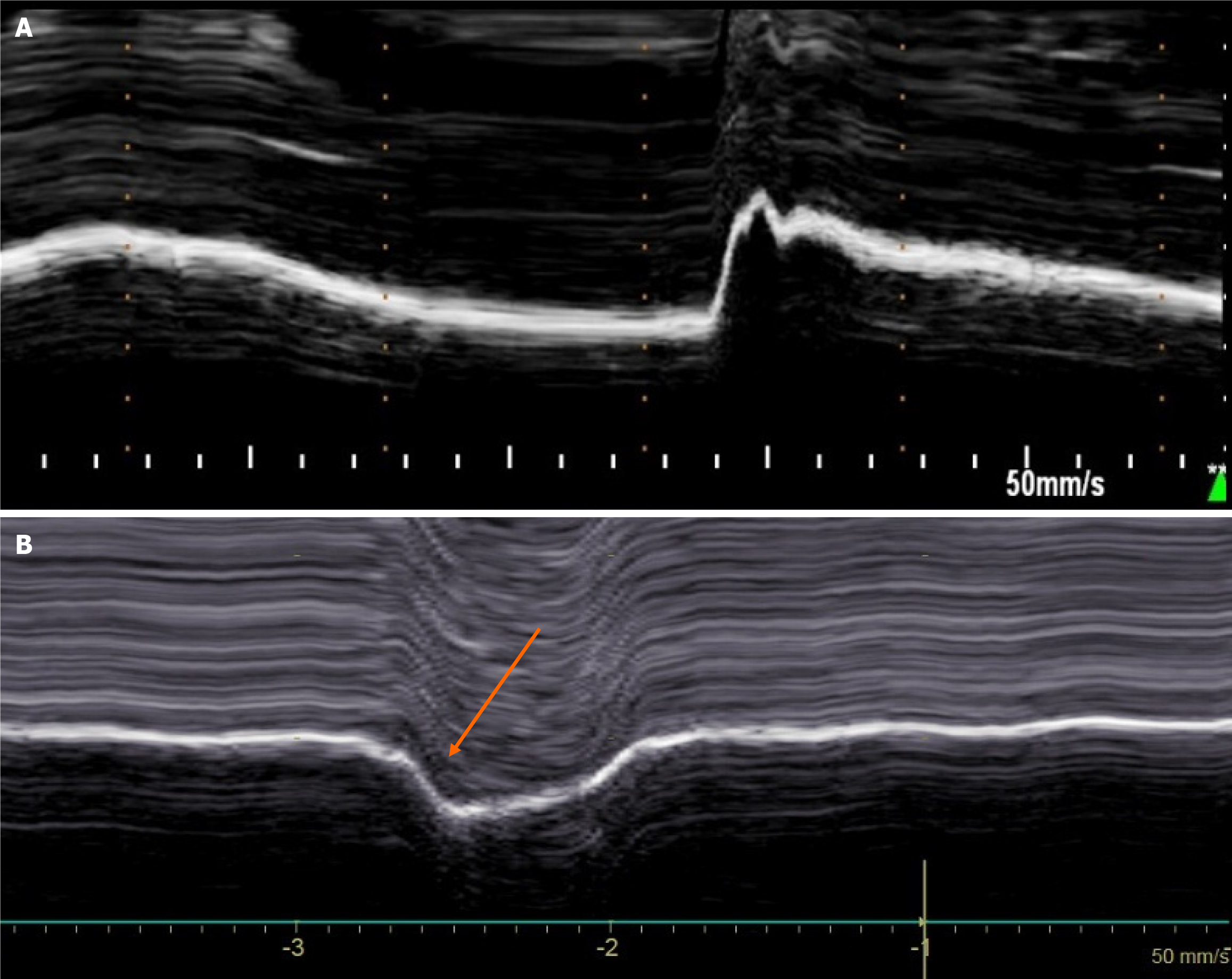
In patients with unilateral diaphragmatic paralysis, hemidiaphragm movement is absent or paradoxical when breathing at rest[29,30]. During voluntary sniffing, a paradoxical movement (i.e. cranial) of the hemidiaphragm (Figure 3) is reported using M-mode ultrasonography[29,30]. During deep inspiration, a biphasic movement can be recorded with a first paradoxical movement followed by a cranio-caudal excursion[30]. The study of inspiratory thickening is important to support the results of the diaphragm excursion analysis. The failure of the paralyzed diaphragm to thicken results in a decrease in the thickening fraction (TF) calculated as the difference between the diaphragm thickness measured at the end of maximal inspiration and the diaphragm thickness at the end of expiration divided by the diaphragm thickness at the end of expiration×100. No significant thickening (TF less than 20%) or thinning of paralyzed hemidiaphragm is observed[31].
In some patients, diaphragm dysfunction occurred without complete paralysis i.e. diaphragm weakness. Diaphragm weakness can be detected using normal values of excursions and thickening previously determined from the study of healthy controls[32,33]. First, no criteria for complete paralysis should be recorded by ultrasound: No paradoxical movement should be observed during the various maneuvers and the TF should be greater than 20%. Secondly, excursions during deep inspiration should be below the lower limit of normal (LLN) depending on the side and gender according to the reference values[32].
Severity of the weakness may be based on the decrease of the excursion from the lower limit of the normal and the measurement of the thickening fraction[34].
Patients can be classified as follows: (1) Mild hemidiaphragm dysfunction when the excursion is slightly below the lower limit of normal during deep inspiration (excursion > LLN – 1 cm) and a normal or slightly decreased thickening fraction (> 40%); (2) Severe hemidiaphragm dysfunction in patients with a marked decrease in hemidiaphragm excursion (< LLN – 1 cm) associated with a marked decrease in thickening fraction (< 40%).
The complete loss of function of one hemidiaphragm leads to a restrictive syndrome with a decrease in vital capacity of about 25%. After unilateral diaphragm paralysis, a compensatory increase in neural drive to the functioning hemidiaphragm was demonstrated[35], leading to large excursions to the healthy side[36]. The activity of accessory inspiratory muscles is also increased[37].
Disorders induced by diaphragm paralysis can take a wide variety of clinical pictures[38]. Bilateral diaphragm paralysis leads to respiratory failure most often requiring ventilatory support. In case of unilateral hemidiaphragm dysfunction, the compensatory mechanism is effective in patients without severe comorbidities and clinical disorders remain weak. Most often, dyspnea is mild and appears during exercise or in supine position. In contrast, in patients with obesity or with severe pre-existing cardiac or respiratory disease, the impairment in respiratory function leads to clinical disorders that can reach respiratory failure. After cardiac surgery, diaphragm dysfunction is associated with a risk of postoperative pneumonia, mechanical ventilation (non-invasive and invasive ventilation) and increased length of stay in the intensive care unit[39].
Diagnosis may be delayed, indeed, respiratory disorders induced by diaphragm dysfunction are frequently attributed to pre-existing heart disease or pulmonary complications secondary to the procedure. Furthermore, elevated hemidiaphragm secondary to diaphragm dysfunction is sometimes not seen on chest X-ray perfomed in supine position in the intensive care unit. Diagnosis is sometimes made later, for exemple when admitted to a cardiac rehabilitation center[40]. It remains important because persistent diaphragm dysfunction is associated with late respiratory complications[39].
In addition, high frequency of obstructive sleep apnea (OSA) has been reported in patients with diaphragm dys
Less frequently, right-to-left shunt was associated with right hemidiaphragm paralysis[43,44]. The mechanism was a redirection of blood flow from the inferior vena cava directly through the patent foramen ovale secondary to a distortion of cardiac anatomy induced by hemidiaphragmatic paralysis. In patients with hypoxemia, closure of the patent foramen ovale may be necessary[45].
Treatment of diaphragm dysfunction is mainly based on respiratory physiotherapy. In unilateral diaphragm paralysis, inspiratory muscle training improves clinical condition through strengthening of healthy hemidiaphragm and accessory inspiratory muscles[46,47]. The long-term prognosis of hemidiaphragm paralysis is usually favorable with a decrease in respiratory disorders due either to the adaptation of healthy inspiratory muscles, or to the spontaneous improvement of diaphragmatic function.
In a population of patients with diaphragm paralysis of various etiologies, Gayan-Ramirez et al[48] reported functional recovery in the first year after diagnosis in 43% of cases and in two years in 52% of cases. After pediatric cardiac surgery complicated by phrenic nerve injury, recovery was documented in about 55% of children over a median follow-up period of 353 d[49]. In patients with hemidiaphragm paralysis secondary to atrial fibrillation ablation, after a mean follow-up of 3 years, 66% of the study population had complete recovery, 17% had partial recovery, and 17% had no recovery[5]. The average recovery time was 4 months after injury. In cases of poor tolerance of diaphragm paralysis, mechanical ventilatory support such as non-invasive ventilation may be required[50]. In patients with hemidiaphragm paralysis having no recovery and suffering from disabling respiratory disorders, diaphragm plication can be proposed. Surgery is performed through open thoracotomy or video-assisted thoracoscopy[51]. Plication of hemidiaphragm reduces dyspnea, and increases both lung function test and exercise capacity[52,53]. The improvement in quality of life persists for a long time. It is therefore recommended to consider diaphragm plication in patients with unilateral diaphragm paralysis who have an impairment of quality of life secondary to chronic dyspnea.
Cardiac surgery and atrial fibrillation ablation can damage the phrenic nerve causing diaphragm dysfunction. Clinical disorders can be wrongly attributed to pre-existing heart or respiratory diseases, so systematic evaluation of diaphragm function by ultrasound after a procedure at risk of phrenic nerve injury is particularly useful. In such patients, respiratory physiotherapy is able to improve respiratory function through the strengthening of inspiratory muscles. Repeated ultrasound examinations should be performed to monitor potential recovery of diaphragm function. In case of lack of recovery and persistent disabling respiratory disorders, diaphragm plication can be proposed.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: France
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lee SS, South Korea S-Editor: Liu JH L-Editor: A P-Editor: Zhao S
| 1. | Benditt JO. Esophageal and gastric pressure measurements. Respir Care. 2005;50:68-75; discussion 75. [PubMed] |
| 2. | Shawyer A, Chippington S, Quyam S, Schulze-Neick I, Roebuck D. Phrenic nerve injury after image-guided insertion of a tunnelled right internal jugular central venous catheter. Pediatr Radiol. 2012;42:875-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Harris K, Maniatis G, Siddiqui F, Maniatis T. Phrenic nerve injury and diaphragmatic paralysis following pacemaker pulse generator replacement. Heart Lung. 2013;42:65-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Aguirre VJ, Sinha P, Zimmet A, Lee GA, Kwa L, Rosenfeldt F. Phrenic nerve injury during cardiac surgery: mechanisms, management and prevention. Heart Lung Circ. 2013;22:895-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Sacher F, Monahan KH, Thomas SP, Davidson N, Adragao P, Sanders P, Hocini M, Takahashi Y, Rotter M, Rostock T, Hsu LF, Clémenty J, Haïssaguerre M, Ross DL, Packer DL, Jaïs P. Phrenic nerve injury after atrial fibrillation catheter ablation: characterization and outcome in a multicenter study. J Am Coll Cardiol. 2006;47:2498-2503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 246] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 6. | Dimopoulou I, Daganou M, Dafni U, Karakatsani A, Khoury M, Geroulanos S, Jordanoglou J. Phrenic nerve dysfunction after cardiac operations: electrophysiologic evaluation of risk factors. Chest. 1998;113:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 80] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Bruni A, Garofalo E, Pasin L, Serraino GF, Cammarota G, Longhini F, Landoni G, Lembo R, Mastroroberto P, Navalesi P; MaGIC (Magna Graecia Intensive care and Cardiac surgery) Group. Diaphragmatic Dysfunction After Elective Cardiac Surgery: A Prospective Observational Study. J Cardiothorac Vasc Anesth. 2020;34:3336-3344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | DeVita MA, Robinson LR, Rehder J, Hattler B, Cohen C. Incidence and natural history of phrenic neuropathy occurring during open heart surgery. Chest. 1993;103:850-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Moury PH, Cuisinier A, Durand M, Bosson JL, Chavanon O, Payen JF, Jaber S, Albaladejo P. Diaphragm thickening in cardiac surgery: A perioperative prospective ultrasound study. Ann Intensive Care. 2019;9:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Laghlam D, Lê MP, Srour A, Monsonego R, Estagnasié P, Brusset A, Squara P. Diaphragm Dysfunction After Cardiac Surgery: Reappraisal. J Cardiothorac Vasc Anesth. 2021;35:3241-3247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Mali S, Haghaninejad H. Pulmonary complications following cardiac surgery. Arch Med Sci Atheroscler Dis. 2019;4:e280-e285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Esposito RA, Spencer FC. The effect of pericardial insulation on hypothermic phrenic nerve injury during open-heart surgery. Ann Thorac Surg. 1987;43:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Wheeler WE, Rubis LJ, Jones CW, Harrah JD. Etiology and prevention of topical cardiac hypothermia-induced phrenic nerve injury and left lower lobe atelectasis during cardiac surgery. Chest. 1985;88:680-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Maccherini M, Davoli G, Sani G, Rossi P, Giani S, Lisi G, Mazzesi G, Toscano M. Warm heart surgery eliminates diaphragmatic paralysis. J Card Surg. 1995;10:257-261. [PubMed] |
| 15. | Lerolle N, Guérot E, Dimassi S, Zegdi R, Faisy C, Fagon JY, Diehl JL. Ultrasonographic diagnostic criterion for severe diaphragmatic dysfunction after cardiac surgery. Chest. 2009;135:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 146] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Tripp HF, Sees DW, Lisagor PG, Cohen DJ. Is phrenic nerve dysfunction after cardiac surgery related to internal mammary harvesting? J Card Surg. 2001;16:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Zakkar M, Guida G, Suleiman MS, Angelini GD. Cardiopulmonary bypass and oxidative stress. Oxid Med Cell Longev. 2015;2015:189863. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 18. | Lakhani M, Saiful F, Parikh V, Goyal N, Bekheit S, Kowalski M. Recordings of diaphragmatic electromyograms during cryoballoon ablation for atrial fibrillation accurately predict phrenic nerve injury. Heart Rhythm. 2014;11:369-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Miyazaki S, Ichihara N, Nakamura H, Taniguchi H, Hachiya H, Araki M, Takagi T, Iwasawa J, Kuroi A, Hirao K, Iesaka Y. Prospective Evaluation of Electromyography-Guided Phrenic Nerve Monitoring During Superior Vena Cava Isolation to Anticipate Phrenic Nerve Injury. J Cardiovasc Electrophysiol. 2016;27:390-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Mol D, Renskers L, Balt JC, Bhagwandien RE, Blaauw Y, van Driel VJHM, Driessen AHG, Elvan A, Folkeringa R, Hassink RJ, Hooft van Huysduynen B, Luermans JGLM, Stevenhagen JY, van der Voort PH, Westra SW, de Groot JR, de Jong JSSG; Netherlands Heart Registration Ablation Committee. Persistent phrenic nerve palsy after atrial fibrillation ablation: Follow-up data from The Netherlands Heart Registration. J Cardiovasc Electrophysiol. 2022;33:559-564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 21. | Almorad A, Del Monte A, Della Rocca DG, Pannone L, Ramak R, Overeinder I, Bala G, Ströker E, Sieira J, Dubois A, Sorgente A, El Haddad M, Iacopino S, Boveda S, de Asmundis C, Chierchia GB. Outcomes of pulmonary vein isolation with radiofrequency balloon vs. cryoballoon ablation: a multi-centric study. Europace. 2023;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 22. | Urbanek L, Bordignon S, Schaack D, Chen S, Tohoku S, Efe TH, Ebrahimi R, Pansera F, Hirokami J, Plank K, Koch A, Schulte-Hahn B, Schmidt B, Chun KJ. Pulsed Field Versus Cryoballoon Pulmonary Vein Isolation for Atrial Fibrillation: Efficacy, Safety, and Long-Term Follow-Up in a 400-Patient Cohort. Circ Arrhythm Electrophysiol. 2023;16:389-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 72] [Reference Citation Analysis (0)] |
| 23. | Trovato GM. Thoracic ultrasound: A complementary diagnostic tool in cardiology. World J Cardiol. 2016;8:566-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Targhetta R, Chavagneux R, Ayoub J, Lemerre C, Préfaut C, Bourgeois JM, Balmes P. [Right diaphragmatic kinetics measured by TM-mode ultrasonography with concomitant spirometry in normal subjects and asthmatic patients. Preliminary results]. Rev Med Interne. 1995;16:819-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Kantarci F, Mihmanli I, Demirel MK, Harmanci K, Akman C, Aydogan F, Mihmanli A, Uysal O. Normal diaphragmatic motion and the effects of body composition: determination with M-mode sonography. J Ultrasound Med. 2004;23:255-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 81] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Epelman M, Navarro OM, Daneman A, Miller SF. M-mode sonography of diaphragmatic motion: description of technique and experience in 278 pediatric patients. Pediatr Radiol. 2005;35:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen JA, Watson JC, Sorenson EJ. Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve. 2013;47:884-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 211] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 28. | Summerhill EM, Angov N, Garber C, McCool FD. Respiratory muscle strength in the physically active elderly. Lung. 2007;185:315-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Lloyd T, Tang YM, Benson MD, King S. Diaphragmatic paralysis: the use of M mode ultrasound for diagnosis in adults. Spinal Cord. 2006;44:505-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 30. | Boussuges A, Brégeon F, Blanc P, Gil JM, Poirette L. Characteristics of the paralysed diaphragm studied by M-mode ultrasonography. Clin Physiol Funct Imaging. 2019;39:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Gottesman E, McCool FD. Ultrasound evaluation of the paralyzed diaphragm. Am J Respir Crit Care Med. 1997;155:1570-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 216] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 32. | Boussuges A, Finance J, Chaumet G, Brégeon F. Diaphragmatic motion recorded by M-mode ultrasonography: limits of normality. ERJ Open Res. 2021;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 33. | Boussuges A, Rives S, Finance J, Chaumet G, Vallée N, Risso JJ, Brégeon F. Ultrasound Assessment of Diaphragm Thickness and Thickening: Reference Values and Limits of Normality When in a Seated Position. Front Med (Lausanne). 2021;8:742703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 34. | Boussuges A, Habert P, Chaumet G, Rouibah R, Delorme L, Menard A, Million M, Bartoli A, Guedj E, Gouitaa M, Zieleskiewicz L, Finance J, Coiffard B, Delliaux S, Brégeon F. Diaphragm dysfunction after severe COVID-19: An ultrasound study. Front Med (Lausanne). 2022;9:949281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 35. | Katagiri M, Young RN, Platt RS, Kieser TM, Easton PA. Respiratory muscle compensation for unilateral or bilateral hemidiaphragm paralysis in awake canines. J Appl Physiol (1985). 1994;77:1972-1982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Houston JG, Fleet M, Cowan MD, McMillan NC. Comparison of ultrasound with fluoroscopy in the assessment of suspected hemidiaphragmatic movement abnormality. Clin Radiol. 1995;50:95-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 115] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 37. | LoMauro A, Aliverti A, Perchiazzi G, Frykholm P. Physiological changes and compensatory mechanisms by the action of respiratory muscles in a porcine model of phrenic nerve injury. J Appl Physiol (1985). 2021;130:813-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 38. | Ben-Dov I, Kaminski N, Reichert N, Rosenman J, Shulimzon T. Diaphragmatic paralysis: a clinical imitator of cardiorespiratory diseases. Isr Med Assoc J. 2008;10:579-583. [PubMed] |
| 39. | Laghlam D, Naudin C, Srour A, Monsonego R, Malvy J, Rahoual G, Squara P, Nguyen LS, Estagnasié P. Persistent diaphragm dysfunction after cardiac surgery is associated with adverse respiratory outcomes: a prospective observational ultrasound study. Can J Anaesth. 2023;70:228-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 40. | Boussuges A, Chaumet G, Poirette L. Interest of ultrasonographic assessment of diaphragmatic function in cardiac rehabilitation center: a case report. Medicine (Baltimore). 2015;94:e801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Sarac S, Salturk C, Oruc O, Metin SK, Bayram S, Karakurt Z, Yalcınkaya I. Sleep-related breathing disorders in diaphragmatic pathologies. Sleep Breath. 2022;26:959-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 42. | Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK. Sleep Apnea: Types, Mechanisms, and Clinical Cardiovascular Consequences. J Am Coll Cardiol. 2017;69:841-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 570] [Cited by in RCA: 914] [Article Influence: 114.3] [Reference Citation Analysis (0)] |
| 43. | Darchis JS, Ennezat PV, Charbonnel C, Aubert JM, Gonin X, Auffray JL, Bauchart JJ, Le Tourneau T, Rey C, Godart F, Goldstein P, Asseman P. Hemidiaphragmatic paralysis: an underestimated etiology of right-to-left shunt through patent foramen ovale? Eur J Echocardiogr. 2007;8:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 44. | Wiertsema MH, Dickinson MG, Hoendermis ES, Geluk CA. Platypnea orthodeoxia syndrome after recent stroke: a case report of a sandwiched right atrium. Eur Heart J Case Rep. 2022;6:ytac275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 45. | Fabris T, Buja P, Cucchini U, D'Amico G, Cazzuffi R, Balestro E, Tarantini G. Right-to-left interatrial shunt secondary to right hemidiaphragmatic paralysis: an unusual scenario for urgent percutaneous closure of patent foramen ovale. Heart Lung Circ. 2015;24:e56-e59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 46. | Kodric M, Trevisan R, Torregiani C, Cifaldi R, Longo C, Cantarutti F, Confalonieri M. Inspiratory muscle training for diaphragm dysfunction after cardiac surgery. J Thorac Cardiovasc Surg. 2013;145:819-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 47. | Schaeffer MR, Louvaris Z, Rodrigues A, Poddighe D, Gayan-Ramirez G, Gojevic T, Geerts L, Heyndrickx E, Van Hollebeke M, Janssens L, Gosselink R, Testelmans D, Langer D. Effects of inspiratory muscle training on exertional breathlessness in patients with unilateral diaphragm dysfunction: a randomised trial. ERJ Open Res. 2023;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 48. | Gayan-Ramirez G, Gosselin N, Troosters T, Bruyninckx F, Gosselink R, Decramer M. Functional recovery of diaphragm paralysis: a long-term follow-up study. Respir Med. 2008;102:690-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 49. | Smith BM, Ezeokoli NJ, Kipps AK, Azakie A, Meadows JJ. Course, predictors of diaphragm recovery after phrenic nerve injury during pediatric cardiac surgery. Ann Thorac Surg. 2013;96:938-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 50. | Carlson CS, Brown SR, Wilson MW, Choi PJ. Noninvasive ventilation: An important option in the management of hemidiaphragm paralysis. J Card Surg. 2021;36:3921-3923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 51. | Beshay M, Abdel Bary M, Kösek V, Vordemvenne T, Mertzlufft F, Schulte Am Esch J. Minimally-Invasive Diaphragmatic Plication in Patients with Unilateral Diaphragmatic Paralysis. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 52. | Freeman RK, Van Woerkom J, Vyverberg A, Ascioti AJ. Long-term follow-up of the functional and physiologic results of diaphragm plication in adults with unilateral diaphragm paralysis. Ann Thorac Surg. 2009;88:1112-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 53. | Hunt AR, Stuart CM, Gergen AK, Bang TJ, Reihman AE, Helmkamp LJ, Lin Y, Mitchell JD, Meguid RA, Scott CD, Wojcik BM. Long-Term Patient-Reported Symptom Improvement and Quality of Life after Transthoracic Diaphragm Plication in Adults. J Am Coll Surg. 2023;237:533-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |