Published online Mar 26, 2024. doi: 10.4330/wjc.v16.i3.109
Peer-review started: December 15, 2023
First decision: January 25, 2024
Revised: February 1, 2024
Accepted: March 4, 2024
Article in press: March 4, 2024
Published online: March 26, 2024
Processing time: 96 Days and 23 Hours
Autophagy is a prosurvival mechanism for the clearance of accumulated abnormal proteins, damaged organelles, and excessive lipids within mammalian cells. A growing body of data indicates that autophagy is reduced in aging cells. This reduction leads to various diseases, such as myocardial hypertrophy, infarction, and atherosclerosis. Recent studies in animal models of an aging heart showed that fasting-induced autophagy improved cardiac function and longevity. This improvement is related to autophagic clearance of damaged cellular components via either bulk or selective autophagy (such as mitophagy). In this editorial, we summarize the mechanisms of autophagy in normal and aging hearts. In addition, the protective effect of fasting-induced autophagy in cardiac aging has been highlighted.
Core Tip: Autophagy is an essential mechanism for the clearance of harmful cellular components, which accumulate with age. However, autophagic machinery decreases with age, resulting in various diseases, such as cardiac hypertrophy. Recently, fasting-induced autophagy has been reported to improve cardiac function in animal models of aging via normalization of defective autophagic machinery. Therefore, autophagy is an important target for the prevention of cardiac pathologies in the geriatric population.
- Citation: Parvaresh H, Paczek K, Al-Bari MAA, Eid N. Mechanistic insights into fasting-induced autophagy in the aging heart. World J Cardiol 2024; 16(3): 109-117
- URL: https://www.wjgnet.com/1949-8462/full/v16/i3/109.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i3.109
Improvements in treatment procedures have contributed to increased life expectancy and growth in the aged population, especially in industrialized countries[1]. Aging is associated with a structural and functional decline in multiple organs, such as the heart. A sedentary lifestyle can also accelerate the incidence of aging-related diseases, including cardio
Cardiovascular aging affects both the heart and the blood circulation system through slow and progressive alterations that can result in the development of left ventricular hypertrophy, diastolic dysfunction, coronary artery disease, stroke, hypertension, atherosclerosis, atrial fibrillation, and heart failure[6-9]. Aortic valve sclerosis is a valvulopathy associated with aging and is characterized by myxomatous degeneration, collagen deposition, and progression to aortic stenosis (AS)[10]. AS is an indicator of increased CVD risk and is mainly defined as increased leaflet calcification and decreased leaflet mobility[11]. Moreover, approximately 13%-16% of elderly people suffer from aortic regurgitation[12], which results in left ventricular dilation and dysfunction over time. Another valvular change related to aging is mitral annular calcification, which usually accompanies aortic valve sclerosis[13].
The free radical theory of aging and the mitochondrial theory have been suggested to explain the cellular deterioration observed in aging and suggest that the age-related decline in mitochondrial function and structure is a major driver of cardiomyocyte senescence, which causes endothelial dysfunction, alteration in the vasculature, and/or vascular injury[14].
Cellular senescence is activated following multiple stressors, including the elevation of reactive oxygen species (ROSs); proinflammatory cytokines; and metabolic, mechanical, and chemical toxicity. Cellular senescence impairs the repair and regeneration of damaged cells in cardiovascular tissues[15-17]. Cellular senescence is characterized by genome instability, telomere attrition, and mitochondrial dysfunction[18].
Dysfunctional mitochondria produce less ATP while also generating increased amounts of ROS[19], exposing aged cardiomyocytes to high levels of oxidative stress. Autophagic and proteasomal degradation are the main mechanisms for the removal of damaged mitochondria and abnormal proteins in aged postmitotic cardiomyocytes. However, these mechanisms decline with age[20]. Eventually, when these mechanisms are unable to compensate for the accumulated cellular damage, stem-cell exhaustion and altered intercellular communication occur, further contributing to aging[18].
Autophagy activity is usually reduced with age[21]. A decrease in autophagy in the hearts of aged flies[22] and aged C57BL/6 mice (20-26 months old) has been reported[23,24].
Autophagy is a protective housekeeping mechanism critical for cellular homeostasis and survival. Long-lived, damaged, and dysfunctional organelles; misfolded proteins; and invading pathogens are eliminated through this degradation process, providing building components for cellular renovation to effectively adapt cells to stressful conditions, such as nutrient deprivation, hypoxia, or oxidative stress[25,26].
Autophagy can be selective or nonselective. Under starvation conditions, the protein and any cytoplasmic content can be non-selectively targeted for catabolic recycling to maintain cellular energy production. However, there are also selective forms of autophagy that specifically target damaged organelles. For instance, mitophagy is a type of autophagy that selectively removes damaged mitochondria[27]. Mitochondria play a substantial role in cellular functions as well as cellular death. Thus, mitochondrial dysfunction is a crucial determinant of lifespan across species[28,29].
Three types of autophagy have been recognized: Macroautophagy, microautophagy, and chaperone-mediated autophagy, all of which lead to the turnover of intracellular components via various mechanisms. “Autophagy” is a term that generally refers to macroautophagy, which is the most prevalent form of autophagy[30,31].
Autophagy is initiated when several autophagy-related gene products (Atg1-Atg12) and other proteins are organized to form a phagophore. These proteins consist of at least five molecular components that mediate fusion between autophagosome (AP) and lysosomes: (1) The Atg1/unc-51-like kinase complex; (2) the Beclin 1/class III phosphatidylinositol 3-kinase (PI3K) complex; (3) Atg9 and vacuole membrane protein 1; (4) two ubiquitin-like proteins (Atg12 and Atg8/LC3) conjugation systems; and (5) proteins that mediate fusion between APs and lysosomes[25,32].
The initial step of AP formation starts with Beclin1 (Atg6) and class III PI3K, which play crucial roles in vesicle isolation. Other Atg proteins are involved in Beclin-1-mediated formation of the Class III PI3K complex. In the next step, the AP undergoes elongation via two conjugation systems. First, Atg12 is conjugated to Atg5 with the help of Atg7 and Atg10[33,34], followed by the conjugation of phosphatidylethanolamine to microtubule-associated protein 1 LC3 via Atg4, Atg7 and Atg3. Consequently, the cytoplasmic LC3 (LC3-I) is converted to membranous (LC3-II) form, which is responsible for formation and maturation of the AP[35]. In the end, fusion of APs and lysosomes occurs with the formation of autolysosome (AL) for degradation and recycling[36].
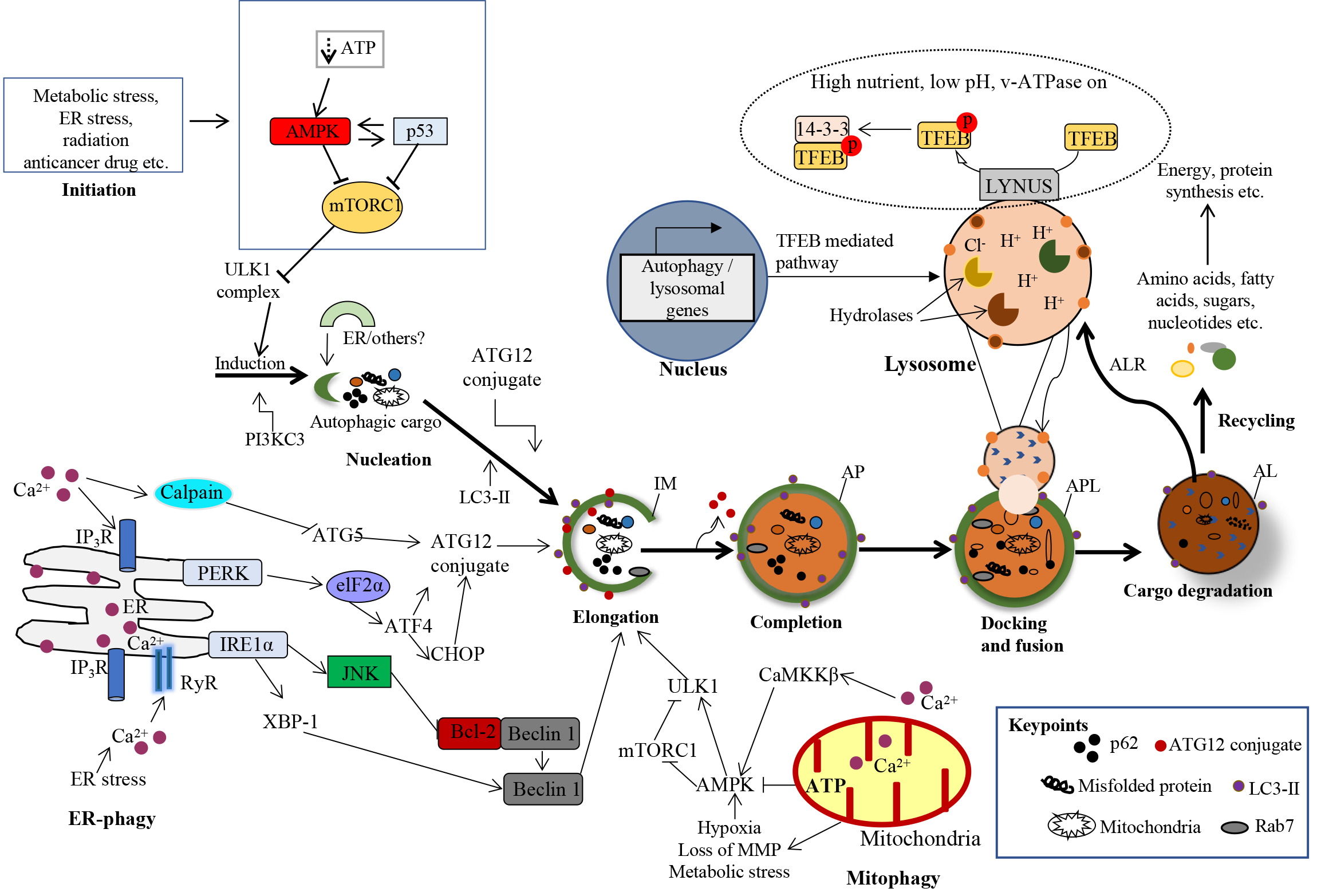
The protein kinases mammalian target of rapamycin (mTOR) and AMP-activated protein kinase (AMPK) are implicated in the regulatory mechanisms of autophagy. Autophagy is inhibited by the mTOR. Phosphorylation of Unc-51 Like autophagy activating kinase-1 (ULK1) by AMPK is involved in autophagy promotion, although mTOR represses this process[37]. Figure 1 demonstrates the various mechanisms of autophagy in mammalian cells.
Accumulating evidence reveals that autophagy plays essential homeostatic roles in the heart under normal physiological conditions and during the aging process; additionally, it has an essential role in improving the immune response and reducing inflammation[38]. Consequently, any perturbations to this process in the cardiovascular system can elicit harmful effects on health.
Autophagy attenuates with age and has serious implications for heart structure and function. A decrease in autophagy causes the development of heart failure, hypertension, atherosclerosis, and ischemic heart disease[39].
Mitophagy is the selective autophagic clearance of damaged mitochondria and is crucial for the bioenergetics of the cardiovascular system; thus, mitophagy dysfunction is generally accompanied by cardiac disorders[27,40,41]. In addition, studies have suggested that autophagic degradation of damaged mitochondria decelerates cardiovascular senescence and has a positive effect on the healthy lifespan of animals[42-44].
Cardiomyocytes undergo age-related changes in proteostasis pathways, resulting in calcium homeostasis impairment, ROSs induction, hypertrophy and fibrosis, and eventual structural damage and diminished cardiac function. Moreover, with age, the MTOR-1 complex is significantly upregulated, and the AMPK pathway is downregulated. In addition, transcription factors involved in autophagy and lysosomal proteins such as TFEB and Forkhead transcription factor (FOXO) 3 are deactivated with advanced aging, resulting in reduced expression of autophagy genes[28-31].
Any defect in the autophagy process accelerates aging; likewise, aging is suppressed when autophagy is stimulated. Deletion of atg5, a cardiac-specific autophagy-related gene, in adult mice leads to an accelerated aging phenotype, including the development of cardiac hypertrophy, left ventricular dilatation, and contractile dysfunction[20,45].
Mutations in the atg4c gene increase the risk of heart disease in elderly patients and eventually death[46]. Cardiomyocyte-specific deletion of glycogen synthase kinase-3 in mice reduced basal autophagy levels and accelerated cardiac aging[47]. Dysfunction of autophagy with age slows the turnover of damaged proteasomes and contributes to age-associated CVD and cardiomyocyte senescence[48]. Mitophagy is impaired in aged mice, and mitophagy induction improves mitochondrial function and reduces arterial wall stiffness[49].
Acyl-coenzyme A binding protein (ACBP), which is encoded by a diazepambinding inhibitor (DBI), acts as an extracellular feedback inhibitor of autophagy[50]. It appears that high ACBP/DBI values correlate with future cardiovascular events (such as heart surgery, myocardial infarction, and stroke), suggesting that ACBP/DBI is indeed a biomarker of biological aging[39].
Although there are many potential causes underlying the decline in cardiovascular function with age, a major determinant of the aging process is likely the progressive loss of quality control due to reduced autophagy.
Hyperactivation of mTOR and reduced AMPK activity[51] in old age can directly inhibit autophagy by inactivating the pro-autophagic ULK1 complex[52], contributing to the downregulation of autophagy activity.
It is conceivable that exposure to excessive ROS during aging promotes the accumulation of oxidized proteins, mitochondrial DNA mutations, and protein misfolding[53]. Additionally, several cytosolic and mitochondrion-localized proteins involved in autophagy regulation become dysfunctional, thus contributing to abnormal mitochondrial turnover and the removal of damaged mitochondria[54]. This chain of events results in impaired autophagy due to exhaustion of the aged autophagic machinery.
In addition, it has been proposed that a hallmark of aging in postmitotic cells, such as cardiomyocytes, is the aggregation of nondegradable structures inside lysosomes, termed lipofuscin, which impedes lysosomal function and therefore can likely inhibit autophagy[55].
It has been shown that intracellular calcium has a key regulatory effect on cardiomyocyte autophagy. Inositol 1,4,5-trisphosphate (IP3) receptors mediate calcium release and transfer to mitochondria. This process inhibits autophagy by suppressing AMPK activation[56]. Since evidence has shown that IP3 receptors are upregulated in the aged, hyper
FOXO and sirtuin proteins are also major metabolic regulators that mediate age-related vascular changes, particularly endothelial dysfunction[9].
Dietary interventions involving caloric restriction (CR) and fasting are among several stress stimuli that can induce autophagy in response to food deprivation[60-62]. CR was defined as a reduction in caloric intake using a diet containing adequate amounts of protein, vitamins, and minerals[63]. CR is a potent inducer of autophagy in the heart[64], and its positive impacts on health and lifespan in various model organisms, primates and humans have been studied[65-67]. CR is the most potent physiological stimulus of autophagy and ameliorates cardiac dysfunction (systolic and diastolic) and attenuates myocardial hypertrophy and fibrosis at the cardiomyocyte level. CR reduces mitochondrial damage, lipid accumulation, oxidative stress, apoptosis, telomere shortening, senescence marker levels, and circulating proinflammatory cytokine levels[68].
Autophagy plays an important role in CR-mediated longevity[69] via clearance of damaged mitochondria, reduction of oxidative stress, improvement of insulin sensitivity and suppression of inflammatory responses[61,62].
Short-term CR for 10 wk in mice rejuvenated symptoms of the aging heart, such as significant improvement in diastolic function and regression of age-dependent cardiac hypertrophy[70]. Moreover, CR reversed age-dependent cardiac proteome remodeling and mitigated oxidative damage and ubiquitination in these mice.
In aged animals, hypertrophy, and fibrosis, as well as systolic and diastolic dysfunctions, improved after CR[68,71]. The beneficial effects of CR observed in cardiomyocytes include enhanced mitochondrial fitness and reduced oxidative stress, apoptotic cell death, inflammation, and importantly, senescence[68]. In vasculature, CR helps improve endothelial cell function and attenuates collagen deposition, elastin remodeling, and oxidative stress; as a result, CR reduces arterial stiffness[72]. Another study revealed improvements in numerous markers of cardiovascular health in humans after short-term periodic fasting, which is also a pro-autophagic dietary regimen[73].
Intermittent fasting (IF) has attracted the attention of researchers as a dietary intervention associated with better compliance and long-term adherence than CR in recent years[74]. IF consists of regular cycles of times with no or minimal caloric intake interrupted by periods of normal food consumption. Alternate day fasting delays cardiac aging in rats, as determined by reduced hypertrophy and fibrosis[75,76] and extended lifespan[77]. The advantageous effects of life-long alternate-day fasting were attributed to reduced phosphoinositide 3-kinase signaling, which was associated with reduced myocardial collagen deposition, oxidative stress, inflammatory markers, and B-type natriuretic peptide levels[75,78].
A fasting-mimicking diet (FMD) is considered another form of dietary intervention in which individuals consume low amounts of calories, sugars, and proteins but high amounts of unsaturated fats. Studies of FMD effects in mice have shown improved cognitive function and a rejuvenated immune system, in addition to promoting lifespan and health factors by reducing cancer incidence, obesity, and inflammation[79]. FMD was investigated in humans, and the findings showed reduced age-related CVD risk factors, including reduced blood pressure, body mass index, fasting glucose, and inflammation, as well as an improved lipid profile[80].
The efficacy of fasting on autophagy in the heart was assessed in male FBN rats by randomly dividing them into different groups of equal amounts of protein, vitamin, and mineral intake, while the CR groups received 20% less food from a 125% fortified diet for six weeks. Additionally, in addition to one simple CR group, two other CR groups were given 5 or 50 mg/kg/day resveratrol. Compared with AL group, a marked reduction of expression of p62 (autophagy substrate) in the left ventricle was observed in the CR and Resv-50 rats, indicating enhanced cardiac autophagy in the CR group. Similarly, a significant overexpression of Beclin-1 was found in the Resv-50 and CR animals. The CR + Resv-50 group of rats showed dramatically attenuated doxorubicin-induced damage, which can be due to enhanced autophagy[81]. Another study investigated the autophagic response of CR on diabetic rat hearts. Diabetic and nondiabetic rats were exposed to a CR diet (30% energy reduction) for 32 wk. Compared with those of diabetic AL rats, diabetic CR rats exhibited an increase in the hepatic and cardiac LC3-II/LC3-I ratio (indicating enhanced autophagy)[82].
A high-fat diet (HFD) (fat 60% kcal/100 kcal fat) was given to the FVBN male mice for 4-20 wk, after which they were subjected to overnight fasting to study the mechanisms of fasting-induced autophagy in the fatty mice heart. After 24 h of fasting, there was a significant conversion of LC3-I conversion to LC3-II in lean mice heart but was not associated with a change in diet-induced obesity (DIO) mice. Furthermore, fasting suppressed mTOR in both lean and DIO mice, as indicated by increased AMPK phosphorylation and enhanced dephosphorylation of S6. Interestingly, mTOR inhibition was greater in obese mice. Taken together, these findings indicate that fasting activates autophagy in the hearts of lean mice[83].
Godar et al[84] investigated the impacts of IF on the autophagy-lysosome machinery in the myocardium. The authors studied the effects of fasting after 24 h, followed by 24 h of refeeding or 24 and 48 h of fasting for six weeks. The AP abundance increased dramatically after 48 h of fasting. Treatment with chloroquine (an autophagy inhibitor) was associated with a significant increase in LC3-II and SQSTM1/p62 after 24 h of fasting but not in fed mice. Thus, fasting induces autophagy in cardiomyocytes; however, autophagy returns to basal levels on gestational days.
The effects of IF on right ventricular (RV) function in a rat model of pulmonary arterial hypertension (characterized by RV mitochondrial dysfunction and resultant lipotoxicity and microbiome dysbiosis) were explored. IF improved RV systolic and diastolic function and decreased RV cardiomyocyte hypertrophy and fibrosis, which was likely mediated by autophagy activation[85]. These protective effects could be related to autophagy activation.
Recent findings from studies also show that cardiometabolic parameters (e.g., adiposity, insulin sensitivity, and cardiac function) can be influenced by the time of day at which food is consumed[86]. To test the hypothesis that fasting during the sleep period elicits beneficial adaptation effects on cardiac function, wild-type mice were fasted for 24 h or for either the 12-h light/sleep phase or the 12-h dark/awake phase. Repression of myocardial p-mTOR and protein synthesis occurred during the dark phase; both parameters remained elevated in the hearts of fasted mice during the light phase. In contrast, markers of autophagy (e.g., LC3-II) exhibited peak responses to fasting during the light phase. Collectively, these data show that the responsiveness of the heart to fasting is temporally partitioned[86].
IF alleviated HFD-induced obesity cardiomyopathy in male C57BL/6J mice by improving cardiac functional and structural impairment and serum lipid metabolic disorders induced by HFD through decreasing lipid deposition, apoptosis and m6A methylation in the heart[87].
Researchers compared the effects of alternate day fasting on elderly (aged 24 months) and young (aged 6 months) male rats. The results of this study indicated that alternate day fasting protected against inflammation and fibrosis in the heart during aging by inhibiting oxidative damage and NF-κB activation[76]. Other studies have shown that fasting preconditioning activates AMPK, induces autophagy, decreases ROS levels, and inhibits NF-κB signaling in the cardiac tissues of rats[88]. In addition, compared with fasting controls, IF in human subjects resulted in autophagy upregulation and reduced levels of proinflammatory cytokines, indicating the protective effects of fasting on the vascular system. This effect is most likely mediated by the anti-inflammatory effects of autophagy[89]. We investigated fasting-induced autophagy among large groups of population in the UAE during Ramadan (the holy Islamic fasting month). The results of this study will be published shortly in specific journals. Furthermore, these results were presented in part at the Sharjah First International Conference on Fasting, February 28-29, 2024, at Sharjah University, United Arab Emirates[90].
In conclusion, fasting-induced autophagy is beneficial for ensuring cardiac function, preventing disease, and improving longevity. However, additional studies in vivo in animal models of cardiac aging are needed to determine the specific molecular mechanisms involved in normalizing autophagy by fasting. In addition, large-scale studies on humans are needed. Ramadan fasting, a type of IF (a common religious practice) in Islamic countries, could be investigated in large groups of geriatric people with or without cardiac diseases. Importantly, further in vitro research should be directed toward human cardiac tissues to better understand the molecular mechanisms of fasting-induced autophagy and its beneficial effects on longevity pathways and prevention of CVDs.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wu L, China S-Editor: Qu XL L-Editor: A P-Editor: Guo X
| 1. | Lutz W, Sanderson W, Scherbov S. The coming acceleration of global population ageing. Nature. 2008;451:716-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 816] [Cited by in RCA: 717] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 2. | Mattson MP. Lifelong brain health is a lifelong challenge: from evolutionary principles to empirical evidence. Ageing Res Rev. 2015;20:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 3. | Mattson MP, Arumugam TV. Hallmarks of Brain Aging: Adaptive and Pathological Modification by Metabolic States. Cell Metab. 2018;27:1176-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 755] [Cited by in RCA: 752] [Article Influence: 107.4] [Reference Citation Analysis (0)] |
| 4. | Evans MA, Sano S, Walsh K. Cardiovascular Disease, Aging, and Clonal Hematopoiesis. Annu Rev Pathol. 2020;15:419-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 105] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 5. | Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020;141:e139-e596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3254] [Cited by in RCA: 5489] [Article Influence: 1097.8] [Reference Citation Analysis (1)] |
| 6. | Cai Y, Liu H, Song E, Wang L, Xu J, He Y, Zhang D, Zhang L, Cheng KK, Jin L, Wu M, Liu S, Qi D, Lopaschuk GD, Wang S, Xu A, Xia Z. Deficiency of telomere-associated repressor activator protein 1 precipitates cardiac aging in mice via p53/PPARα signaling. Theranostics. 2021;11:4710-4727. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 7. | Hu C, Zhang X, Teng T, Ma ZG, Tang QZ. Cellular Senescence in Cardiovascular Diseases: A Systematic Review. Aging Dis. 2022;13:103-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 95] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 8. | Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part I: aging arteries: a "set up" for vascular disease. Circulation. 2003;107:139-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1567] [Cited by in RCA: 1570] [Article Influence: 71.4] [Reference Citation Analysis (0)] |
| 9. | North BJ, Sinclair DA. The intersection between aging and cardiovascular disease. Circ Res. 2012;110:1097-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 640] [Cited by in RCA: 998] [Article Influence: 76.8] [Reference Citation Analysis (0)] |
| 10. | Otto CM. Why is aortic sclerosis associated with adverse clinical outcomes? J Am Coll Cardiol. 2004;43:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Dai DF, Chen T, Johnson SC, Szeto H, Rabinovitch PS. Cardiac aging: from molecular mechanisms to significance in human health and disease. Antioxid Redox Signal. 2012;16:1492-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 239] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 12. | Nassimiha D, Aronow WS, Ahn C, Goldman ME. Association of coronary risk factors with progression of valvular aortic stenosis in older persons. Am J Cardiol. 2001;87:1313-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Jeon DS, Atar S, Brasch AV, Luo H, Mirocha J, Naqvi TZ, Kraus R, Berman DS, Siegel RJ. Association of mitral annulus calcification, aortic valve sclerosis and aortic root calcification with abnormal myocardial perfusion single photon emission tomography in subjects age < or =65 years old. J Am Coll Cardiol. 2001;38:1988-1993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Zhao RZ, Jiang S, Zhang L, Yu ZB. Mitochondrial electron transport chain, ROS generation and uncoupling (Review). Int J Mol Med. 2019;44:3-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 236] [Cited by in RCA: 556] [Article Influence: 92.7] [Reference Citation Analysis (0)] |
| 15. | Colavitti R, Finkel T. Reactive oxygen species as mediators of cellular senescence. IUBMB Life. 2005;57:277-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 191] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 16. | Olivieri F, Prattichizzo F, Grillari J, Balistreri CR. Cellular Senescence and Inflammaging in Age-Related Diseases. Mediators Inflamm. 2018;2018:9076485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 17. | Lewis-McDougall FC, Ruchaya PJ, Domenjo-Vila E, Shin Teoh T, Prata L, Cottle BJ, Clark JE, Punjabi PP, Awad W, Torella D, Tchkonia T, Kirkland JL, Ellison-Hughes GM. Aged-senescent cells contribute to impaired heart regeneration. Aging Cell. 2019;18:e12931. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 209] [Cited by in RCA: 219] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 18. | López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153:1194-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10570] [Cited by in RCA: 10393] [Article Influence: 866.1] [Reference Citation Analysis (0)] |
| 19. | Lesnefsky EJ, Chen Q, Hoppel CL. Mitochondrial Metabolism in Aging Heart. Circ Res. 2016;118:1593-1611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 242] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 20. | Taneike M, Yamaguchi O, Nakai A, Hikoso S, Takeda T, Mizote I, Oka T, Tamai T, Oyabu J, Murakawa T, Nishida K, Shimizu T, Hori M, Komuro I, Takuji Shirasawa TS, Mizushima N, Otsu K. Inhibition of autophagy in the heart induces age-related cardiomyopathy. Autophagy. 2010;6:600-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 354] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 21. | Russ DW, Boyd IM, McCoy KM, McCorkle KW. Muscle-specificity of age-related changes in markers of autophagy and sphingolipid metabolism. Biogerontology. 2015;16:747-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Chang C, Kang P, Liu Y, Huang K, Taylor E, Sagona AP, Nezis IP, Bodmer R, Ocorr K, Bai H. Activin Signaling Regulates Autophagy and Cardiac Aging through mTORC2. BioRxiv. 2017;139360. [DOI] [Full Text] |
| 23. | Ren J, Yang L, Zhu L, Xu X, Ceylan AF, Guo W, Yang J, Zhang Y. Akt2 ablation prolongs life span and improves myocardial contractile function with adaptive cardiac remodeling: role of Sirt1-mediated autophagy regulation. Aging Cell. 2017;16:976-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 24. | Linton PJ, Gurney M, Sengstock D, Mentzer RM Jr, Gottlieb RA. This old heart: Cardiac aging and autophagy. J Mol Cell Cardiol. 2015;83:44-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 25. | Kroemer G, Mariño G, Levine B. Autophagy and the integrated stress response. Mol Cell. 2010;40:280-293. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2886] [Cited by in RCA: 2759] [Article Influence: 183.9] [Reference Citation Analysis (0)] |
| 26. | He C, Bassik MC, Moresi V, Sun K, Wei Y, Zou Z, An Z, Loh J, Fisher J, Sun Q, Korsmeyer S, Packer M, May HI, Hill JA, Virgin HW, Gilpin C, Xiao G, Bassel-Duby R, Scherer PE, Levine B. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature. 2012;481:511-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 904] [Cited by in RCA: 902] [Article Influence: 69.4] [Reference Citation Analysis (0)] |
| 27. | Alim Al-Bari A, Ito Y, Thomes PG, Menon MB, García-Macia M, Fadel R, Stadlin A, Peake N, Faris ME, Eid N, Klionsky DJ. Emerging mechanistic insights of selective autophagy in hepatic diseases. Front Pharmacol. 2023;14:1149809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Reference Citation Analysis (0)] |
| 28. | Al-Bari MAA, Ito Y, Ahmed S, Radwan N, Ahmed HS, Eid N. Targeting Autophagy with Natural Products as a Potential Therapeutic Approach for Cancer. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 29. | Eid N, Ito Y, Otsuki Y. The autophagic response to alcohol toxicity: the missing layer. J Hepatol. 2013;59:398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Parzych KR, Klionsky DJ. An overview of autophagy: morphology, mechanism, and regulation. Antioxid Redox Signal. 2014;20:460-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1222] [Cited by in RCA: 1844] [Article Influence: 167.6] [Reference Citation Analysis (0)] |
| 31. | Koutouroushis C, Sarkar O. Role of Autophagy in Cardiovascular Disease and Aging. Cureus. 2021;13:e20042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Wang L, Ye X, Zhao T. The physiological roles of autophagy in the mammalian life cycle. Biol Rev Camb Philos Soc. 2019;94:503-516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 33. | Meijer AJ, Codogno P. Regulation and role of autophagy in mammalian cells. Int J Biochem Cell Biol. 2004;36:2445-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 438] [Cited by in RCA: 461] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 34. | Sun Q, Fan W, Chen K, Ding X, Chen S, Zhong Q. Identification of Barkor as a mammalian autophagy-specific factor for Beclin 1 and class III phosphatidylinositol 3-kinase. Proc Natl Acad Sci U S A. 2008;105:19211-19216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 417] [Cited by in RCA: 414] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 35. | Nishida K, Kyoi S, Yamaguchi O, Sadoshima J, Otsu K. The role of autophagy in the heart. Cell Death Differ. 2009;16:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 305] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 36. | Gatica D, Chiong M, Lavandero S, Klionsky DJ. Molecular mechanisms of autophagy in the cardiovascular system. Circ Res. 2015;116:456-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 215] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 37. | Russell RC, Tian Y, Yuan H, Park HW, Chang YY, Kim J, Kim H, Neufeld TP, Dillin A, Guan KL. ULK1 induces autophagy by phosphorylating Beclin-1 and activating VPS34 lipid kinase. Nat Cell Biol. 2013;15:741-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1001] [Cited by in RCA: 1233] [Article Influence: 102.8] [Reference Citation Analysis (0)] |
| 38. | Rubinsztein DC, Mariño G, Kroemer G. Autophagy and aging. Cell. 2011;146:682-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1509] [Cited by in RCA: 1639] [Article Influence: 117.1] [Reference Citation Analysis (0)] |
| 39. | Sasaki Y, Ikeda Y, Iwabayashi M, Akasaki Y, Ohishi M. The Impact of Autophagy on Cardiovascular Senescence and Diseases. Int Heart J. 2017;58:666-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 40. | Bravo-San Pedro JM, Kroemer G, Galluzzi L. Autophagy and Mitophagy in Cardiovascular Disease. Circ Res. 2017;120:1812-1824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 337] [Cited by in RCA: 632] [Article Influence: 79.0] [Reference Citation Analysis (0)] |
| 41. | Nicolás-Ávila JA, Lechuga-Vieco AV, Esteban-Martínez L, Sánchez-Díaz M, Díaz-García E, Santiago DJ, Rubio-Ponce A, Li JL, Balachander A, Quintana JA, Martínez-de-Mena R, Castejón-Vega B, Pun-García A, Través PG, Bonzón-Kulichenko E, García-Marqués F, Cussó L, A-González N, González-Guerra A, Roche-Molina M, Martin-Salamanca S, Crainiciuc G, Guzmán G, Larrazabal J, Herrero-Galán E, Alegre-Cebollada J, Lemke G, Rothlin CV, Jimenez-Borreguero LJ, Reyes G, Castrillo A, Desco M, Muñoz-Cánoves P, Ibáñez B, Torres M, Ng LG, Priori SG, Bueno H, Vázquez J, Cordero MD, Bernal JA, Enríquez JA, Hidalgo A. A Network of Macrophages Supports Mitochondrial Homeostasis in the Heart. Cell. 2020;183:94-109.e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 483] [Article Influence: 96.6] [Reference Citation Analysis (0)] |
| 42. | Zaglia T, Milan G, Ruhs A, Franzoso M, Bertaggia E, Pianca N, Carpi A, Carullo P, Pesce P, Sacerdoti D, Sarais C, Catalucci D, Krüger M, Mongillo M, Sandri M. Atrogin-1 deficiency promotes cardiomyopathy and premature death via impaired autophagy. J Clin Invest. 2014;124:2410-2424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 43. | Gong G, Song M, Csordas G, Kelly DP, Matkovich SJ, Dorn GW 2nd. Parkin-mediated mitophagy directs perinatal cardiac metabolic maturation in mice. Science. 2015;350:aad2459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 366] [Cited by in RCA: 359] [Article Influence: 35.9] [Reference Citation Analysis (0)] |
| 44. | Eisenberg T, Abdellatif M, Schroeder S, Primessnig U, Stekovic S, Pendl T, Harger A, Schipke J, Zimmermann A, Schmidt A, Tong M, Ruckenstuhl C, Dammbrueck C, Gross AS, Herbst V, Magnes C, Trausinger G, Narath S, Meinitzer A, Hu Z, Kirsch A, Eller K, Carmona-Gutierrez D, Büttner S, Pietrocola F, Knittelfelder O, Schrepfer E, Rockenfeller P, Simonini C, Rahn A, Horsch M, Moreth K, Beckers J, Fuchs H, Gailus-Durner V, Neff F, Janik D, Rathkolb B, Rozman J, de Angelis MH, Moustafa T, Haemmerle G, Mayr M, Willeit P, von Frieling-Salewsky M, Pieske B, Scorrano L, Pieber T, Pechlaner R, Willeit J, Sigrist SJ, Linke WA, Mühlfeld C, Sadoshima J, Dengjel J, Kiechl S, Kroemer G, Sedej S, Madeo F. Cardioprotection and lifespan extension by the natural polyamine spermidine. Nat Med. 2016;22:1428-1438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 838] [Article Influence: 93.1] [Reference Citation Analysis (0)] |
| 45. | Nakai A, Yamaguchi O, Takeda T, Higuchi Y, Hikoso S, Taniike M, Omiya S, Mizote I, Matsumura Y, Asahi M, Nishida K, Hori M, Mizushima N, Otsu K. The role of autophagy in cardiomyocytes in the basal state and in response to hemodynamic stress. Nat Med. 2007;13:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1138] [Cited by in RCA: 1215] [Article Influence: 67.5] [Reference Citation Analysis (0)] |
| 46. | Walter S, Atzmon G, Demerath EW, Garcia ME, Kaplan RC, Kumari M, Lunetta KL, Milaneschi Y, Tanaka T, Tranah GJ, Völker U, Yu L, Arnold A, Benjamin EJ, Biffar R, Buchman AS, Boerwinkle E, Couper D, De Jager PL, Evans DA, Harris TB, Hoffmann W, Hofman A, Karasik D, Kiel DP, Kocher T, Kuningas M, Launer LJ, Lohman KK, Lutsey PL, Mackenbach J, Marciante K, Psaty BM, Reiman EM, Rotter JI, Seshadri S, Shardell MD, Smith AV, van Duijn C, Walston J, Zillikens MC, Bandinelli S, Baumeister SE, Bennett DA, Ferrucci L, Gudnason V, Kivimaki M, Liu Y, Murabito JM, Newman AB, Tiemeier H, Franceschini N. A genome-wide association study of aging. Neurobiol Aging. 2011;32:2109.e15-2109.e28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 47. | Zhou J, Force T. Focusing the spotlight on GSK-3 in aging. Aging (Albany NY). 2013;5:388-389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Korolchuk VI, Menzies FM, Rubinsztein DC. A novel link between autophagy and the ubiquitin-proteasome system. Autophagy. 2009;5:862-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 98] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 49. | LaRocca TJ, Hearon CM Jr, Henson GD, Seals DR. Mitochondrial quality control and age-associated arterial stiffening. Exp Gerontol. 2014;58:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 50. | Bravo-San Pedro JM, Sica V, Martins I, Anagnostopoulos G, Maiuri C, Kroemer G. Cell-autonomous, paracrine and neuroendocrine feedback regulation of autophagy by DBI/ACBP (diazepam binding inhibitor, acyl-CoA binding protein): the obesity factor. Autophagy. 2019;15:2036-2038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 51. | Johnson SC, Rabinovitch PS, Kaeberlein M. mTOR is a key modulator of ageing and age-related disease. Nature. 2013;493:338-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1093] [Cited by in RCA: 1256] [Article Influence: 104.7] [Reference Citation Analysis (0)] |
| 52. | Kim J, Kundu M, Viollet B, Guan KL. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat Cell Biol. 2011;13:132-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4208] [Cited by in RCA: 5536] [Article Influence: 395.4] [Reference Citation Analysis (0)] |
| 53. | Dai DF, Rabinovitch PS, Ungvari Z. Mitochondria and cardiovascular aging. Circ Res. 2012;110:1109-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 318] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 54. | Ikeda Y, Sciarretta S, Nagarajan N, Rubattu S, Volpe M, Frati G, Sadoshima J. New insights into the role of mitochondrial dynamics and autophagy during oxidative stress and aging in the heart. Oxid Med Cell Longev. 2014;2014:210934. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 95] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 55. | Brunk UT, Terman A. Lipofuscin: mechanisms of age-related accumulation and influence on cell function. Free Radic Biol Med. 2002;33:611-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 627] [Cited by in RCA: 638] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 56. | Cárdenas C, Miller RA, Smith I, Bui T, Molgó J, Müller M, Vais H, Cheung KH, Yang J, Parker I, Thompson CB, Birnbaum MJ, Hallows KR, Foskett JK. Essential regulation of cell bioenergetics by constitutive InsP3 receptor Ca2+ transfer to mitochondria. Cell. 2010;142:270-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 879] [Cited by in RCA: 854] [Article Influence: 56.9] [Reference Citation Analysis (0)] |
| 57. | Wu X, Zhang T, Bossuyt J, Li X, McKinsey TA, Dedman JR, Olson EN, Chen J, Brown JH, Bers DM. Local InsP3-dependent perinuclear Ca2+ signaling in cardiac myocyte excitation-transcription coupling. J Clin Invest. 2006;116:675-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 376] [Cited by in RCA: 382] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 58. | Yamda J, Ohkusa T, Nao T, Ueyama T, Yano M, Kobayashi S, Hamano K, Esato K, Matsuzaki M. Up-regulation of inositol 1,4,5 trisphosphate receptor expression in atrial tissue in patients with chronic atrial fibrillation. J Am Coll Cardiol. 2001;37:1111-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 59. | Decuypere JP, Welkenhuyzen K, Luyten T, Ponsaerts R, Dewaele M, Molgó J, Agostinis P, Missiaen L, De Smedt H, Parys JB, Bultynck G. Ins(1,4,5)P3 receptor-mediated Ca2+ signaling and autophagy induction are interrelated. Autophagy. 2011;7:1472-1489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 60. | Aris JP, Alvers AL, Ferraiuolo RA, Fishwick LK, Hanvivatpong A, Hu D, Kirlew C, Leonard MT, Losin KJ, Marraffini M, Seo AY, Swanberg V, Westcott JL, Wood MS, Leeuwenburgh C, Dunn WA Jr. Autophagy and leucine promote chronological longevity and respiration proficiency during calorie restriction in yeast. Exp Gerontol. 2013;48:1107-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 61. | Libert S, Guarente L. Metabolic and neuropsychiatric effects of calorie restriction and sirtuins. Annu Rev Physiol. 2013;75:669-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 62. | Rickenbacher A, Jang JH, Limani P, Ungethüm U, Lehmann K, Oberkofler CE, Weber A, Graf R, Humar B, Clavien PA. Fasting protects liver from ischemic injury through Sirt1-mediated downregulation of circulating HMGB1 in mice. J Hepatol. 2014;61:301-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 91] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 63. | Most J, Tosti V, Redman LM, Fontana L. Calorie restriction in humans: An update. Ageing Res Rev. 2017;39:36-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 347] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 64. | Wohlgemuth SE, Julian D, Akin DE, Fried J, Toscano K, Leeuwenburgh C, Dunn WA Jr. Autophagy in the heart and liver during normal aging and calorie restriction. Rejuvenation Res. 2007;10:281-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 136] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 65. | Roth GS, Mattison JA, Ottinger MA, Chachich ME, Lane MA, Ingram DK. Aging in rhesus monkeys: relevance to human health interventions. Science. 2004;305:1423-1426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 235] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 66. | Fontana L, Meyer TE, Klein S, Holloszy JO. Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A. 2004;101:6659-6663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 641] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 67. | Postnikoff SDL, Johnson JE, Tyler JK. The integrated stress response in budding yeast lifespan extension. Microb Cell. 2017;4:368-375. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 68. | Sheng Y, Lv S, Huang M, Lv Y, Yu J, Liu J, Tang T, Qi H, Di W, Ding G. Opposing effects on cardiac function by calorie restriction in different-aged mice. Aging Cell. 2017;16:1155-1167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 69. | Ntsapi C, Loos B. Caloric restriction and the precision-control of autophagy: A strategy for delaying neurodegenerative disease progression. Exp Gerontol. 2016;83:97-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 70. | Dai DF, Karunadharma PP, Chiao YA, Basisty N, Crispin D, Hsieh EJ, Chen T, Gu H, Djukovic D, Raftery D, Beyer RP, MacCoss MJ, Rabinovitch PS. Altered proteome turnover and remodeling by short-term caloric restriction or rapamycin rejuvenate the aging heart. Aging Cell. 2014;13:529-539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 203] [Cited by in RCA: 258] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 71. | Shinmura K, Tamaki K, Sano M, Murata M, Yamakawa H, Ishida H, Fukuda K. Impact of long-term caloric restriction on cardiac senescence: caloric restriction ameliorates cardiac diastolic dysfunction associated with aging. J Mol Cell Cardiol. 2011;50:117-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 72. | Donato AJ, Walker AE, Magerko KA, Bramwell RC, Black AD, Henson GD, Lawson BR, Lesniewski LA, Seals DR. Life-long caloric restriction reduces oxidative stress and preserves nitric oxide bioavailability and function in arteries of old mice. Aging Cell. 2013;12:772-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 145] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 73. | Stekovic S, Hofer SJ, Tripolt N, Aon MA, Royer P, Pein L, Stadler JT, Pendl T, Prietl B, Url J, Schroeder S, Tadic J, Eisenberg T, Magnes C, Stumpe M, Zuegner E, Bordag N, Riedl R, Schmidt A, Kolesnik E, Verheyen N, Springer A, Madl T, Sinner F, de Cabo R, Kroemer G, Obermayer-Pietsch B, Dengjel J, Sourij H, Pieber TR, Madeo F. Alternate Day Fasting Improves Physiological and Molecular Markers of Aging in Healthy, Non-obese Humans. Cell Metab. 2019;30:462-476.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 268] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 74. | Johnstone A. Fasting for weight loss: an effective strategy or latest dieting trend? Int J Obes (Lond). 2015;39:727-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 75. | Castello L, Maina M, Testa G, Cavallini G, Biasi F, Donati A, Leonarduzzi G, Bergamini E, Poli G, Chiarpotto E. Alternate-day fasting reverses the age-associated hypertrophy phenotype in rat heart by influencing the ERK and PI3K signaling pathways. Mech Ageing Dev. 2011;132:305-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 76. | Castello L, Froio T, Maina M, Cavallini G, Biasi F, Leonarduzzi G, Donati A, Bergamini E, Poli G, Chiarpotto E. Alternate-day fasting protects the rat heart against age-induced inflammation and fibrosis by inhibiting oxidative damage and NF-kB activation. Free Radic Biol Med. 2010;48:47-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 77. | Goodrick CL, Ingram DK, Reynolds MA, Freeman JR, Cider NL. Effects of intermittent feeding upon growth and life span in rats. Gerontology. 1982;28:233-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 101] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 78. | Inuzuka Y, Okuda J, Kawashima T, Kato T, Niizuma S, Tamaki Y, Iwanaga Y, Yoshida Y, Kosugi R, Watanabe-Maeda K, Machida Y, Tsuji S, Aburatani H, Izumi T, Kita T, Shioi T. Suppression of phosphoinositide 3-kinase prevents cardiac aging in mice. Circulation. 2009;120:1695-1703. [PubMed] [DOI] [Full Text] |
| 79. | Brandhorst S, Choi IY, Wei M, Cheng CW, Sedrakyan S, Navarrete G, Dubeau L, Yap LP, Park R, Vinciguerra M, Di Biase S, Mirzaei H, Mirisola MG, Childress P, Ji L, Groshen S, Penna F, Odetti P, Perin L, Conti PS, Ikeno Y, Kennedy BK, Cohen P, Morgan TE, Dorff TB, Longo VD. A Periodic Diet that Mimics Fasting Promotes Multi-System Regeneration, Enhanced Cognitive Performance, and Healthspan. Cell Metab. 2015;22:86-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 511] [Cited by in RCA: 611] [Article Influence: 61.1] [Reference Citation Analysis (0)] |
| 80. | Wei M, Brandhorst S, Shelehchi M, Mirzaei H, Cheng CW, Budniak J, Groshen S, Mack WJ, Guen E, Di Biase S, Cohen P, Morgan TE, Dorff T, Hong K, Michalsen A, Laviano A, Longo VD. Fasting-mimicking diet and markers/risk factors for aging, diabetes, cancer, and cardiovascular disease. Sci Transl Med. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 365] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 81. | Dutta D, Xu J, Dirain ML, Leeuwenburgh C. Calorie restriction combined with resveratrol induces autophagy and protects 26-month-old rat hearts from doxorubicin-induced toxicity. Free Radic Biol Med. 2014;74:252-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 82. | Makino N, Oyama J, Maeda T, Koyanagi M, Higuchi Y, Tsuchida K. Calorie restriction increases telomerase activity, enhances autophagy, and improves diastolic dysfunction in diabetic rat hearts. Mol Cell Biochem. 2015;403:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 83. | Andres AM, Kooren JA, Parker SJ, Tucker KC, Ravindran N, Ito BR, Huang C, Venkatraman V, Van Eyk JE, Gottlieb RA, Mentzer RM Jr. Discordant signaling and autophagy response to fasting in hearts of obese mice: Implications for ischemia tolerance. Am J Physiol Heart Circ Physiol. 2016;311:H219-H228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 84. | Godar RJ, Ma X, Liu H, Murphy JT, Weinheimer CJ, Kovacs A, Crosby SD, Saftig P, Diwan A. Repetitive stimulation of autophagy-lysosome machinery by intermittent fasting preconditions the myocardium to ischemia-reperfusion injury. Autophagy. 2015;11:1537-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 144] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 85. | Prisco SZ, Eklund M, Moutsoglou DM, Prisco AR, Khoruts A, Weir EK, Thenappan T, Prins KW. Intermittent Fasting Enhances Right Ventricular Function in Preclinical Pulmonary Arterial Hypertension. J Am Heart Assoc. 2021;10:e022722. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 86. | Brewer RA, Collins HE, Berry RD, Brahma MK, Tirado BA, Peliciari-Garcia RA, Stanley HL, Wende AR, Taegtmeyer H, Rajasekaran NS, Darley-Usmar V, Zhang J, Frank SJ, Chatham JC, Young ME. Temporal partitioning of adaptive responses of the murine heart to fasting. Life Sci. 2018;197:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 87. | Xu Z, Qin Y, Lv B, Tian Z, Zhang B. Intermittent Fasting Improves High-Fat Diet-Induced Obesity Cardiomyopathy via Alleviating Lipid Deposition and Apoptosis and Decreasing m6A Methylation in the Heart. Nutrients. 2022;14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 44] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 88. | Yue XY, Wang XB, Zhao RZ, Jiang S, Zhou X, Jiao B, Zhang L, Yu ZB. Fasting improves tolerance to acute hypoxia in rats. Biochem Biophys Res Commun. 2021;569:161-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 89. | Malinowski B, Zalewska K, Węsierska A, Sokołowska MM, Socha M, Liczner G, Pawlak-Osińska K, Wiciński M. Intermittent Fasting in Cardiovascular Disorders-An Overview. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 150] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 90. | Eid N, Al-Bari MAA, Menon MB. Fasting-induced autophagy in health and disease: history, mechanisms, and benefits. Sharjah First International Conference on Fasting. 2024. Available from: https://www.sharjah.ac.ae/en/Media/Conferences/1FR/Pages/default.aspx. |