Published online Aug 26, 2022. doi: 10.4330/wjc.v14.i8.454
Peer-review started: October 23, 2021
First decision: April 7, 2022
Revised: May 21, 2022
Accepted: August 5, 2022
Article in press: August 5, 2022
Published online: August 26, 2022
Processing time: 299 Days and 10.2 Hours
Timely and accurate identification of subgroup at risk for major adverse cardiovascular events among patients presenting with acute chest pain remains a challenge. Currently available risk stratification scores are suboptimal. Recently, a new scoring system called the Symptoms, history of Vascular disease, Electrocardiography, Age, and Troponin (SVEAT) score has been shown to outperform the History, Electrocardiography, Age, Risk factors and Troponin (HEART) score, one of the most used risk scores in the United States.
To assess the potential usefulness of the SVEAT score as a risk stratification tool by comparing its performance to HEART score in chest pain patients with low suspicion for acute coronary syndrome and admitted for overnight observation.
We retrospectively reviewed medical records of 330 consecutive patients admitted to our clinical decision unit for acute chest pain between January 1st to April 17th, 2019. To avoid potential biases, investigators assigned to calculate the SVEAT, and HEART scores were blinded to the results of 30-d combined endpoint of death, acute myocardial infarction or confirmed coronary artery disease requiring revascularization or medical therapy [30-d major adverse cardiovascular event (MACE)]. An area under receiving-operator characteristic curve (AUC) for each score was then calculated. C-statistic and logistic model were used to compare predictive performance of the two scores.
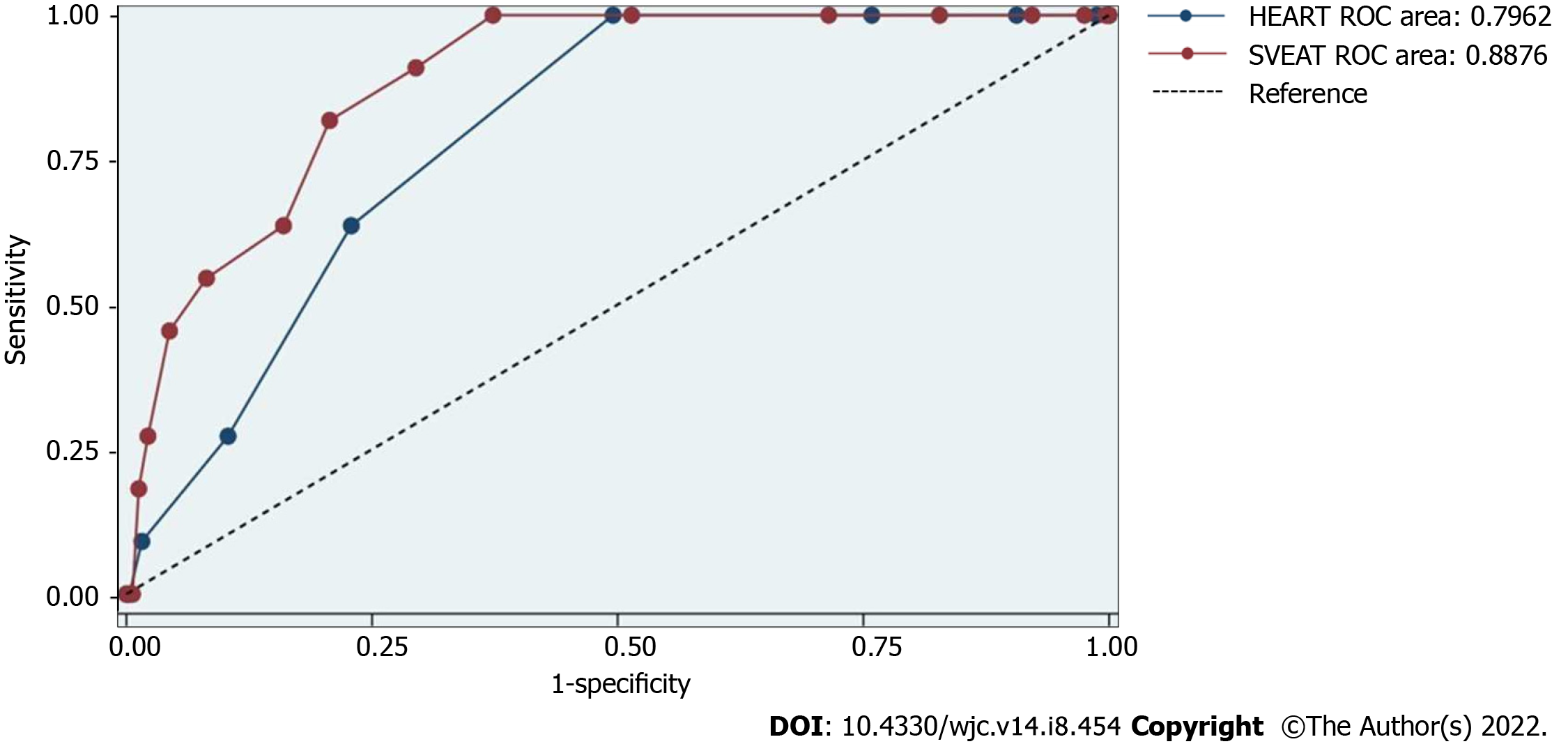
A 30-d MACE was observed in 11 patients (3.33% of the subjects). The AUC of SVEAT score (0.8876, 95%CI: 0.82-0.96) was significantly higher than the AUC of HEART score (0.7962, 95%CI: 0.71-0.88), P = 0.03. Using logistic model, SVEAT score with cut-off of 4 or less significantly predicts 30-d MACE (odd ratio 1.52, 95%CI: 1.19-1.95, P = 0.001) but not the HEART score (odd ratio 1.29, 95%CI: 0.78-2.14, P = 0.32).
The SVEAT score is superior to the HEART score as a risk stratification tool for acute chest pain in low to intermediate risk patients.
Core Tip: Most chest pain risk stratification scores do not use several readily available data. The Symptoms, history of Vascular disease, Electrocardiography, Age, and Troponin (SVEAT) score was shown to outperform the History, Electrocardiography, Age, Risk factors and Troponin (HEART) score in 30-d major adverse cardiovascular event. In our retrospective cohort study, we validated the performance of the SVEAT score and confirmed that the SVEAT score is superior to the HEART score as a risk stratification tool for acute chest pain in low to intermediate risk patients.
- Citation: Antwi-Amoabeng D, Roongsritong C, Taha M, Beutler BD, Awad M, Hanfy A, Ghuman J, Manasewitsch NT, Singh S, Quang C, Gullapalli N. SVEAT score outperforms HEART score in patients admitted to a chest pain observation unit. World J Cardiol 2022; 14(8): 454-461
- URL: https://www.wjgnet.com/1949-8462/full/v14/i8/454.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i8.454
Acute chest pain is one of the most common presenting symptoms to the emergency department[1,2]. Several non-cardiac conditions share clinical features with acute myocardial infarction and the emergency room clinician must rapidly identify those patients with chest pain who are most likely to have active coronary events from those who have chest pain due to other reasons. The key immediate task is to identify if a patient could benefit from being hospitalized for acute coronary syndrome (ACS) evaluation and those who can be safely discharged. This requires an estimation of the pretest probability of ACS. However, the accuracy of individual history, physical exam and electrocardiogram findings have been found to have limited utility for diagnosing ACS[3]. Therefore, multiple scoring systems and pathways have been proposed as risk stratification tools for these patients[4-7]. Among them, the History, Electrocardiography, Age, Risk factors and Troponin (HEART) score is arguably the most utilized particularly in the United States. Unfortunately, it has been shown in some studies to identify less than half of low-risk patients[4-6,8]. In an unselected population of chest pain patients in the emergency department, the HEART score and clinical gestalt had the same diagnostic accuracy for ACS[9]. The HEART score assigns a maximum score of 2 for chest pain deemed “highly suspicious” for ACS and suggests further inpatient evaluation for ACS for a score of 4 or more. By not clearly defining the classification of a patient’s chest pain, the score introduces subjectivity and considerable inter-rater variability[10]. The score also incorporates traditional cardiac risk factors such as diabetes, hypercholesterolemia, and hypertension, which have been shown to have limited value in diagnosis ACS especially in those older than 40 years[11]. To control health care utilization and cost, it is imperative to identify low risk patients with chest pain for discharge from the emergency department. However, it is perhaps more important to not miss real cases of ACS in otherwise low risk patients. Among patients without the traditional risk factors for ACS, the HEART score may not be sensitive in identifying those who would benefit from further evaluation. Thus, there is a need for alternative risk stratification for this patient group. Recently, a new scoring system based on five sets of clinical variables; characteristics of chest pain Symptoms, history of Vascular disease, Electrocardiography, Age, and Troponin (SVEAT score, Table 1) has been reported to outperform the HEART score[8]. The objective of this study is to assess the potential usefulness of SVEAT score as a risk stratification tool by comparing its performance to HEART score in chest pain patients with low suspicion for acute coronary syndrome and admitted for overnight observation.
| Component | Characteristics | Points |
| Symptoms | Typical unstable angina pectoris | 3 |
| Stable angina, Canadian Cardiovascular Society Class I or II | 1 | |
| Non-cardiac chest pain | -2 | |
| Vascular disease | Recent myocardial infarction or percutaneous coronary intervention < 90 days | 2 |
| Coronary artery bypass grafting > 5 years | 2 | |
| Prior coronary event other than above | 1 | |
| Prior revascularization for peripheral disease or carotid disease | 2 | |
| EKG | Dynamic or new ischemic ST or T wave changes | 3 |
| ST depression of unknown duration without cause | 2 | |
| ST changes with left ventricular hypertrophy, intraventricular conduction delay, digitalis, or metabolic issue | 1 | |
| Old Q wave indicating prior myocardial infarction or pre-existing ST changes | 1 | |
| No ST changes | 0 | |
| Normal EKG in the presence of severe ongoing chest pain | -2 | |
| Age (years) | > 75 | 2 |
| 50-75 | 1 | |
| 30-49 | 0 | |
| < 30 | -1 | |
| Troponin I (ng/mL) | 0.7 or higher | 5 |
| > 0.12 but < 0.7 | 2 | |
| > 0.04 but < or = 0.12 | 1 | |
| Normal (< or = 0.004) with unclear duration of chest pain | 0 | |
| Normal after > 4 h of constant chest pain | -2 |
The registry of patients admitted to our clinical decision units between January 1st to April 17th, 2019, were retrospectively reviewed. Our clinical decision unit allows for close observation of chest pain patients who are at low risk for true major adverse cardiovascular event (MACE). Admission to this unit allows for serial monitoring of the patient’s symptoms, cardiac enzymes, and electrocardiograms. To minimize any potential biases, one group of investigators was assigned to abstract relevant information necessary to calculate SVEAT score, and another was assigned to collect information for HEART score according to the published criteria[4,8]. The occurrence of MACE defined as all-cause mortality, acute myocardial infarction, confirmed coronary artery disease requiring revascularization or medical therapy at 30 d were then validated by two independent investigators who were blinded to the SVEAT and HEART score for each patient. The abstracted data were then provided to another set of investigators who were blinded to the outcome data to calculate the SVEAT and the HEART scores. Patients with ST segment elevation myocardial infraction were excluded from the study. The fourth-generation ultra-high sensitivity troponin I assay was used in all participants at our institution during the study period like the original SVEAT score study. Acute myocardial infarction was diagnosed based on standard criteria[12]. The predictive power of the SVEAT and HEART scores for 30-d MACE were compared using c-statistic, based on area under the receiving-operator characteristic curve (AUC). Chi-squared test for equality of area under the curve was used to compare the performance of the SVEAT score to the HEART score. Categorical variables were summarized as counts (%) and between group comparisons were performed using Fisher’s exact test. Continuous variables were summarized as means ± SD and difference between means by outcome compared using Student’s t-test. All analyses were performed at a two-tailed 5% level of significance using Stata version 16.1 (Stata Corporation, College Station, TX, United States).
A total of 330 subjects were included in the study. Baseline patient characteristics are shown in Table 2. There were slightly more male (52.1%) than female subjects. The mean age was 59.5 ± 13.9 years. The incidence of 30-d MACE in our population was 3.33%. The subjects who suffered 30-d MACE were significantly older than those who did not (74.3 ± 13.2 years vs 59.0 ± 13.6 years, P < 0.0001). There were however no other significant differences in baseline characteristics between the two groups (Table 2).
| Continuous variables | Overall (n = 330) | 30-d MACE | P value | |
| Yes, n = 11 (3.3%) | No, n = 319 (96.7%) | |||
| Age, mean ± SD (yr) | 59.5 ± 13.9 | 74.3 ± 13.2 | 59 ± 13.6 | < 0.0001 |
| BMI, mean ± SD (kg/m2) | 30.7 ± 7.8 | 27.8 ± 6.3 | 30.7 ± 7.8 | 0.23 |
| Males, n (%) | 172 (52.1) | 7 (63.6) | 165 (51.7) | 0.55 |
| Diabetes, n (%) | 94 (28.5) | 5 (45.5) | 89 (27.9) | 0.31 |
| Dyslipidemia, n (%) | 153 (46.4) | 4 (36.4) | 149 (46.7) | 0.55 |
| Hypertension, n (%) | 206 (62.4) | 10 (90.9) | 196 (61.4) | 0.06 |
| Smoker, n (%) | 177 (53.6) | 9 (81.8) | 168 (52.7) | 0.07 |
Figure 1 illustrates the receiver-operator-characteristic curves of the SVEAT and HEART scores in predicting 30-d MACE. The AUC of the SVEAT score (0.8876, 95%CI: 0.82-0.96) is significantly higher than AUC of the HEART score (0.7962, 95%CI: 0.71-0.88), P = 0.03. Using logistic model, SVEAT score ≤ 4 significantly predicted 30-d MACE (odds ratio 1.52, 95%CI: 1.19-1.95, P = 0.001) but the HEART score ≤ 3 did not (odds ratio 1.29, 95%CI: 0.78-2.14, P = 0.32) (Table 3).
| 30-d MACE | Odds ratio | P value | 95%CI |
| HEART score | 1.29 | 0.32 | 0.78-2.14 |
| SVEAT score | 1.52 | 0.001 | 1.19-1.95 |
Currently, despite numerous risk stratification protocols, most low-risk patients presenting with acute chest pain are not being released from emergency department. The 2020 European Society of Cardiology Guideline for ACS recommends using an ultrahigh sensitivity troponin (hs-Tn) assay with 0/1-h hs-Tn protocol for ruling out acute coronary syndrome but also emphasizes the importance of incorporating clinical information into the decision-making process[12]. It additionally proposes using Global Registry of Acute Coronary Events score for prognostic purposes but does not recommend any specific clinical risk score for initial risk stratification[12]. The American College of Cardiology/American Heart Association has not updated their guideline since 2014 when they stated that none of available risk prediction tools at the time was definitively demonstrated to be superior to clinician judgement[13].
The HEART score is perhaps the most widely used risk stratification tool in the United States due to its simplicity and large amount of supporting evidence[6,14,15]. The criteria for its History and EKG component are however somewhat subjective. Consequently, inter-observer variability and scoring inconsistency have been reported[16-18]. More importantly, it has been shown to be able to identify merely less than half of low-risk patients[5,17,18]. One of the potential contributing factors for the latter issue is that the HEART score does not incorporate some of the useful clinical information readily available on initial evaluation. To circumvent some of the pitfalls of the HEART score, the SVEAT score was developed. There are a few differences between the SVEAT and HEART scores. First, larger weight (higher points) is assigned to the findings associated with higher likelihood of subsequent acute coronary event clinically and negative point for those traditionally associated with negative likelihood of the events in a stepwise manner. This approach allows wider range of potential scores, and we believe theoretically could help better discriminating among various risk group of patients. Secondly, the criteria for EKG changes and assigned point for each change are much more clearly defined. Moreover, the presence of vascular disease is included in the SVEAT score instead of risk factor which has been shown to be only a weak predictor in acute chest pain evaluation[19]. In fact, the SVEAT score has recently been shown to outperform the HEART score[8]. Like the previous study, this analysis found SVEAT score to be superior risk stratification tool to HEART score for acute chest pain evaluation in low-risk patients.
There are certainly a few limitations in our study. Firstly, the overall 30-d MACE incidence of 3.3% in this study is rather low and substantially lower than in the previous report of 19.6%[13]. This may unfavorably increase the possibility of our finding to be due to statistical chance. An extremely low event rate in this study is likely explained by our study design to include only those retrospectively identified from a low-risk chest pain registry at our institution. The incidence of MACE in our population however is in line with the recent report of real-world data in the United States where ED visit for acute chest pain exceeds 8 million annually[20]. Among these patients, < 5% of them subsequently experienced acute coronary syndrome. Second, the sample size of our study is relatively small for a retrospective design. As indicated in the methodology section, we did try to design our study to minimize potential biases. Lastly, this is a single center study and therefore future confirmation in a multicenter study in wider range of population, and larger sample size will be needed.
In conclusion, our study suggests potential usefulness of the newly developed SVEAT score as a risk stratification tool among low-risk patients admitted to clinical decision unit for evaluation of acute chest pain. We found that SVEAT score significantly outperforms the commonly used HEART score. Incorporating SVEAT score as part of a clinical assessment of these patients may help improve resource utilization while maintaining minimal risk of future cardiovascular events in low-risk patients presenting to emergency department with acute chest pain.
Cardiovascular disease is the leading cause of death worldwide. Early identification of patients at risk for major cardiovascular events can expedite treatment and significantly reduce morbidity and mortality.
Risk stratification scoring systems used to identify patients at risk of major cardiovascular events, including the History, Electrocardiography, Age, Risk factors and Troponin (HEART) score, are often ineffective and may exclude many patients who would benefit from urgent intervention.
We aimed to assess the value of a new risk stratification scoring system, the Symptoms, history of Vascular disease, Electrocardiography, Age, and Troponin (SVEAT), by comparing its performance to that of the HEART score among chest pain patients with low suspicion for acute coronary syndrome.
We retrospectively reviewed medical records of 330 consecutive patients admitted to our clinical decision unit for acute chest pain between January 1st to April 17th, 2019. To avoid potential biases, investigators assigned to calculate the SVEAT, and HEART scores were blinded to the results of 30-d combined endpoint of death, acute myocardial infarction or confirmed coronary artery disease required revascularization or medical therapy [30-d major adverse cardiovascular event (MACE)].
A 30-d MACE was observed in 11 patients (3.33% of the subjects). The area under receiving-operator characteristic curve (AUC) of SVEAT score (0.8876, 95%CI: 0.82-0.96) was significantly higher than the AUC of HEART score (0.7962, 95%CI: 0.71-0.88), P = 0.03. Using logistic model, SVEAT score with cut-off of 4 or less significantly predicts 30-d MACE (odd ratio 1.52, 95%CI: 1.19-1.95, P = 0.001) but not the HEART score (odd ratio 1.29, 95%CI: 0.78-2.14, P = 0.32).
The SVEAT score is superior to the HEART score as a risk stratification tool for acute chest pain in low to intermediate risk patients.
In our study, the SVEAT score was superior to the HEART score as a risk stratification tool for acute chest pain in low to intermediate risk patients. Future research is warranted to evaluate the SVEAT score among large, heterogeneous populations and among high-risk individuals presenting with chest pain.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Salahi S, Iran S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Ko DT, Dattani ND, Austin PC, Schull MJ, Ross JS, Wijeysundera HC, Tu JV, Eberg M, Koh M, Krumholz HM. Emergency Department Volume and Outcomes for Patients After Chest Pain Assessment. Circ Cardiovasc Qual Outcomes. 2018;11:e004683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008;1-38. [PubMed] |
| 3. | Bates ER. Review: In patients with chest pain, risk scores better predict high risk for ACS than individual risk factors. Ann Intern Med. 2016;164:JC34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Backus BE, Six AJ, Kelder JC, Bosschaert MA, Mast EG, Mosterd A, Veldkamp RF, Wardeh AJ, Tio R, Braam R, Monnink SH, van Tooren R, Mast TP, van den Akker F, Cramer MJ, Poldervaart JM, Hoes AW, Doevendans PA. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol. 2013;168:2153-2158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 398] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 5. | Backus BE, Six AJ, Kelder JC, Mast TP, van den Akker F, Mast EG, Monnink SH, van Tooren RM, Doevendans PA. Chest pain in the emergency room: a multicenter validation of the HEART Score. Crit Pathw Cardiol. 2010;9:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 246] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 6. | Poldervaart JM, Langedijk M, Backus BE, Dekker IMC, Six AJ, Doevendans PA, Hoes AW, Reitsma JB. Comparison of the GRACE, HEART and TIMI score to predict major adverse cardiac events in chest pain patients at the emergency department. Int J Cardiol. 2017;227:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 148] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 7. | Stopyra JP, Miller CD, Hiestand BC, Lefebvre CW, Nicks BA, Cline DM, Askew KL, Riley RF, Russell GB, Burke GL, Herrington D, Hoekstra JW, Mahler SA. Chest Pain Risk Stratification: A Comparison of the 2-Hour Accelerated Diagnostic Protocol (ADAPT) and the HEART Pathway. Crit Pathw Cardiol. 2016;15:46-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Roongsritong C, Taha ME, Pisipati S, Aung S, Latt H, Thomas J, Namballa L, Al-Hasnawi HJ, Taylor MK, Gullapalli N. SVEAT Score, a Potential New and Improved Tool for Acute Chest Pain Risk Stratification. Am J Cardiol. 2020;127:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Visser A, Wolthuis A, Breedveld R, ter Avest E. HEART score and clinical gestalt have similar diagnostic accuracy for diagnosing ACS in an unselected population of patients with chest pain presenting in the ED. Emerg Med J. 2015;32:595-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Gershon CA, Yagapen AN, Lin A, Yanez D, Sun BC. Inter-rater Reliability of the HEART Score. Acad Emerg Med. 2019;26:552-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Han JH, Lindsell CJ, Storrow AB, Luber S, Hoekstra JW, Hollander JE, Peacock WF 4th, Pollack CV, Gibler WB; EMCREG i*trACS Investigators. The role of cardiac risk factor burden in diagnosing acute coronary syndromes in the emergency department setting. Ann Emerg Med. 2007;49:145-152, 152.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, Gale CP, Gilard M, Jobs A, Jüni P, Lambrinou E, Lewis BS, Mehilli J, Meliga E, Merkely B, Mueller C, Roffi M, Rutten FH, Sibbing D, Siontis GCM; ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2569] [Cited by in RCA: 3138] [Article Influence: 784.5] [Reference Citation Analysis (0)] |
| 13. | Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64:e139-e228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1840] [Cited by in RCA: 2188] [Article Influence: 198.9] [Reference Citation Analysis (0)] |
| 14. | Van Den Berg P, Body R. The HEART score for early rule out of acute coronary syndromes in the emergency department: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. 2018;7:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Laureano-Phillips J, Robinson RD, Aryal S, Blair S, Wilson D, Boyd K, Schrader CD, Zenarosa NR, Wang H. HEART Score Risk Stratification of Low-Risk Chest Pain Patients in the Emergency Department: A Systematic Review and Meta-Analysis. Ann Emerg Med. 2019;74:187-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 16. | van Meerten KF, Haan RMA, Dekker IMC, van Zweden HJJ, van Zwet EW, Backus BE. The interobserver agreement of the HEART-score, a multicentre prospective study. Eur J Emerg Med. 2021;28:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Soares WE 3rd, Knee A, Gemme SR, Hambrecht R, Dybas S, Poronsky KE, Mader SC, Mader TJ. A Prospective Evaluation of Clinical HEART Score Agreement, Accuracy, and Adherence in Emergency Department Chest Pain Patients. Ann Emerg Med. 2021;78:231-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Wu WK, Yiadom MY, Collins SP, Self WH, Monahan K. Documentation of HEART score discordance between emergency physician and cardiologist evaluations of ED patients with chest pain. Am J Emerg Med. 2017;35:132-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Hollander JE, Than M, Mueller C. State-of-the-Art Evaluation of Emergency Department Patients Presenting With Potential Acute Coronary Syndromes. Circulation. 2016;134:547-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 20. | Raff GL, Hoffmann U, Udelson JE. Trials of Imaging Use in the Emergency Department for Acute Chest Pain. JACC Cardiovasc Imaging. 2017;10:338-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |