Published online Jul 26, 2022. doi: 10.4330/wjc.v14.i7.438
Peer-review started: March 11, 2022
First decision: May 31, 2022
Revised: June 9, 2022
Accepted: July 8, 2022
Article in press: July 8, 2022
Published online: July 26, 2022
Processing time: 130 Days and 19.5 Hours
Left ventricular (LV) ejection fraction (LVEF), defined as LV stroke volume divided by end-diastolic volume, has been systematically used for the diagnosis, classification, and management of heart failure (HF) over the last three decades. HF is classified as HF with reduced LVEF, HF with midrange or mildly reduced LVEF, and HF with preserved LVEF using arbitrary, continuously changing LVEF cutoffs. A prerequisite for using this LVEF-based terminology is knowledge of the LVEF normal range, which is lacking and may lead to erroneous conclusions in HF, especially at the higher end of the LVEF spectrum.
Core Tip: Left ventricular ejection fraction (LVEF) has been consistently used for the diagnosis, classification, and management of heart failure (HF) over the last three decades. HF is classified as HF with reduced LVEF, HF with midrange or mildly reduced LVEF, and HF with preserved LVEF using arbitrary, continuously changing LVEF cutoffs. A prerequisite for using this terminology is knowledge of the LVEF normal range, which is lacking and may lead to erroneous conclusions, especially at the higher end of the LVEF spectrum.
- Citation: Xanthopoulos A, Giamouzis G, Skoularigis J, Triposkiadis F. Heart failure with reduced, mildly reduced, or preserved left ventricular ejection fraction: Has reasoning been lost? World J Cardiol 2022; 14(7): 438-445
- URL: https://www.wjgnet.com/1949-8462/full/v14/i7/438.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i7.438
Left ventricular (LV) ejection fraction (LVEF), defined as LV stroke volume divided by LV end-diastolic volume, is the only biomarker that has been systematically used for the diagnosis, classification, and management of heart failure (HF) over the last three decades[1]. Accordingly, HF has been classified into HF with reduced LVEF (HFrEF), HF with midrange or mildly reduced LVEF (HFmrEF), and HF with preserved LVEF (HFpEF) using various, continuously changing LVEF cutoffs. A mandatory prerequisite for the use of this LVEF-based terminology is the definition of the normal LVEF range, which is lacking. From this perspective, we discuss the limitations related to the current LVEF-based classification of HF and provide examples of erroneous conclusions that can be drawn, especially in HF patients at the higher end of the HF spectrum.
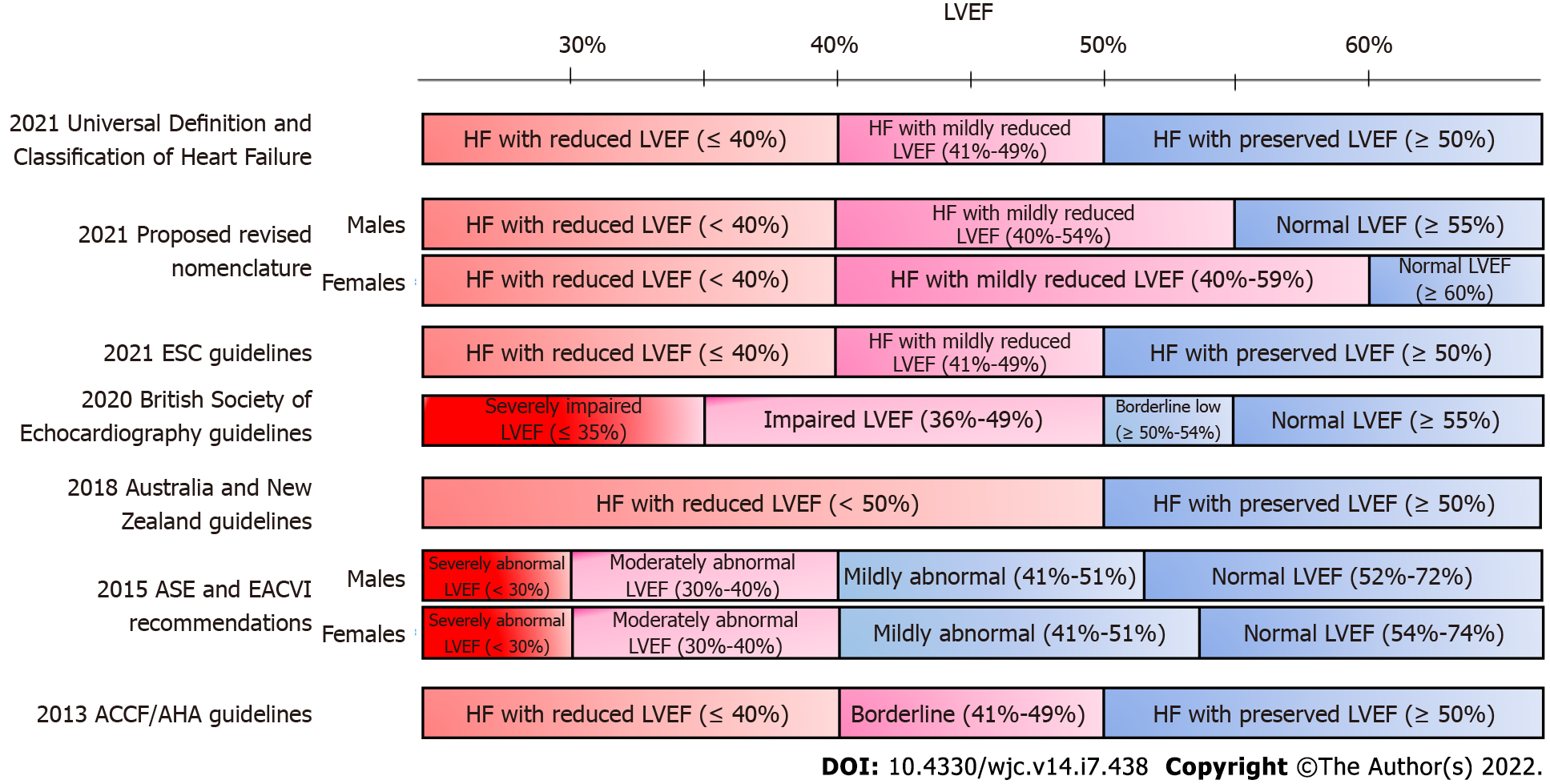
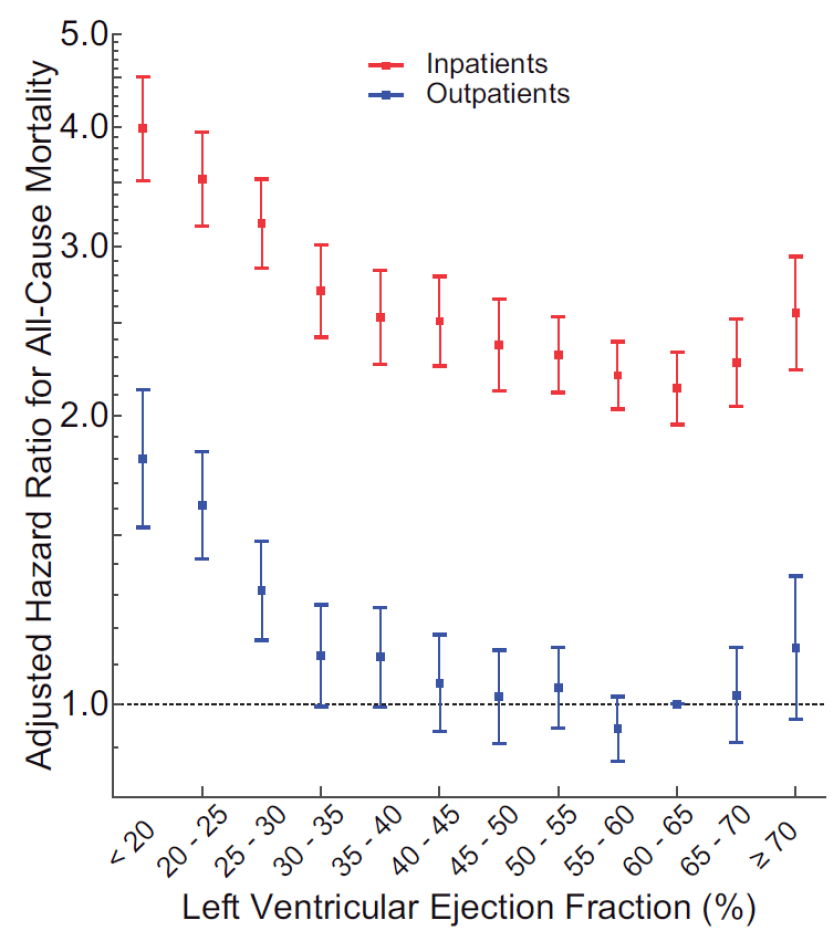
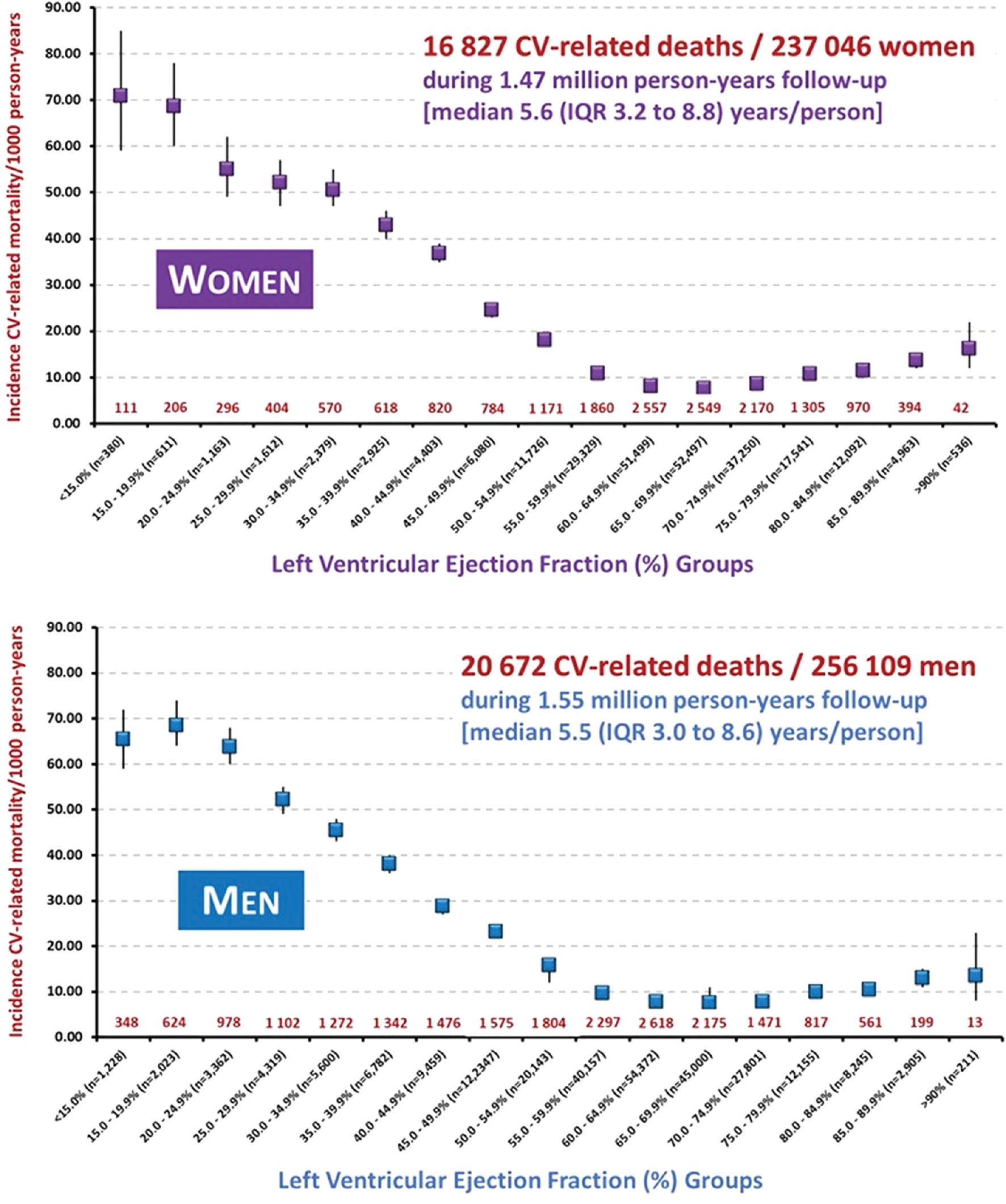
The LVEF-based classification of HF was initially applied several decades ago in the clinical trials of neurohormonal inhibitors in which LVEF cutoffs of < 35% or 40% were chosen arbitrarily to define patients with HF perceived to be at greatest risk (HFrEF). Several years later, clinical trials with similar agents and endpoints were conducted in patients with HF with an LVEF of ≥ 40%-50% (HFpEF), but they were considered unsuccessful for various reasons[2,3]. Recently, another HF phenotype (HFmrEF) was added based on the underrepresentation of patients with HF with an LVEF of 40%-50% in clinical trials. The LVEF cutoffs used for HF classification have varied continuously in the guidelines issued by scientific societies (Figure 1)[4]. The 2013 American College of Cardiology Foundation/American Heart Association guidelines defined HFrEF by an LVEF of ≤ 40%, borderline HFpEF by an LVEF of 41%-49%, and HFpEF by an LVEF of ≥ 50%[5]. By contrast, the National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand guidelines defined HFrEF and HFpEF by an LVEF of < 50% and ≥ 50%, respectively, and did not recognize borderline HFpEF or HFmrEF as a distinct entity[6]. Furthermore, in the recent Universal Definition and Classification of Heart Failure[7], which was adopted by the European Society of Cardiology[8], HF classification includes HFrEF with an LVEF of ≤ 40%, HFmrEF with an LVEF of 41%-49%, and HFpEF with an LVEF of ≥ 50%. Subsequently, another classification of HF was proposed, which defines HFrEF by an LVEF of < 40%, HFmrEF by 40% ≤ LVEF < normal, and HF with normal EF by an LVEF of ≥ 55% in men and ≥ 60% in women[9]. LVEF can be reduced, mildly reduced, preserved, or normal; however, what is the normal LVEF range? According to the 2015 recommendations of the American Society of Echocardiography and the European Association of Cardiovascular Imaging, the normal reference range for LVEF is 52%-72% for males and 54%-74% for females[10]. The latest guidelines from the British Society of Echocardiography define LVEF ≥ 55% as normal (preserved)[11]. However, several recent studies have raised serious concerns regarding the normal LVEF range as proposed by echocardiographic societies. Wehner et al[12] investigated the relationship between LVEF and survival by linking physician-reported LVEF on 403977 echocardiograms obtained from 203135 patients to all-cause mortality in the United States, and validated their findings in a dataset including 45531 echocardiograms and 35976 patients from New Zealand. During follow-up, unadjusted hazard ratios for mortality showed a U-shaped relationship for LVEF with a nadir of risk at an LVEF of 60%-65% in both datasets. The results were similar after adjusting for conditions associated with an elevated LVEF, including mitral regurgitation, increased wall thickness, and anemia and when restricted to patients reported to have HF at the time of the echocardiogram (Figure 2). Slightly different but trending in the same direction were the findings of another study including approximately 500000 participants, which reported that in both women and men, mortality was lowest at an LVEF of 65.0%–69.9%[13]. However, in the same study, sex-dependent differences in the relationship between LVEF and mortality were observed. In women, an increased risk of cardiovascular-related mortality persisted to an LVEF of 60.0%–64.9%, whereas in men, the equivalent LVEF was lower (55.0%–59.9%) (Figure 3)[13]. Sex-related differences were also reported in 4632 patients from coronary computed tomography angiography evaluation for clinical outcomes, namely, an international multicenter registry in which LVEF was measured by cardiac computed tomography and participants were categorized according to LVEF (low < 55%, normal 55%–65%, and high > 65%)[14]. After 6 years of follow-up, no difference in mortality was observed in patients with high LVEF in the overall cohort. However, when data were stratified by sex, women with high LVEF died more often from any cause compared to women with normal LVEF, while an opposite trend was observed in men[14]. Thus, the LVEF-based terminology for HF classification is challenged based on recent evidence.
Therefore, it is not surprising that the LVEF-based classification might lead to erroneous conclusions when interpreting the results of various studies enrolling HF patients at the upper end of the LVEF spectrum (Table 1). A typical example is the recently published Empagliflozin outcome trial in patients with chronic HF with preserved EF (EMPEROR-preserved trial), which reported a benefit with empagliflozin (compared with placebo) in HFpEF defined by an LVEF > 40%[15,16] which is different from the 50% cutoff recommended in the Universal Definition and Classification of Heart Failure[7]. It is noteworthy that in the EMPEROR-preserved trial, ~90% of the patients suffered from hypertension, ~49% from diabetes, and ~51% from atrial fibrillation. By contrast, in a study by Lupon et al[17], which was used as evidence supporting phenotypic persistence in HFpEF[18], an LVEF cutoff of 50% was used and the patient characteristics were entirely different from those in the EMPEROR-preserved trial with approximately 12% of the participants suffering from hypertrophic cardiomyopathy and 36% from valvular heart disease. Thus, when interpreting these two HFpEF studies, it would be challenging to extrapolate the findings of one to the other. Therefore, no firm conclusions can be drawn regarding the effectiveness of empagliflozin or phenotypic persistence in HFpEF.
| Ref. | Drug | LVEF cut off | |
| Registries | |||
| Yancy et al[22] | ADHERE | - | ≥ 40 |
| Fonarow et al[23] | OPTIMIZE-HF | - | ≥ 40%; ≥ 50% |
| Steinberg et al[24] | GWTG-HF | - | ≥ 50%; 40%-50% |
| Randomized controlled trials | |||
| Yusuf et al[25] | CHARM-PRESERVED | Candesartan | > 40% |
| Cleland et al[26] | PEP-CHF | Perindopril | > 40% |
| Massie et al[27] | I-PRESERVE | Irbesartan | ≥ 45% |
| van Veldhuisen et al[28] | SENIORS | Nebivolol | > 35% |
| Redfield et al[29] | RELAX Trial | Phosphodiesterase-5 inhibitors | ≥ 50 |
| Yamamoto et al[30] | J-DHF | Carvedilol | > 40% |
| Ahmed et al[31] | DIG-PEF | Digitalis | > 45% |
| Pitt et al[32] | TOPCAT | Spironolactone | ≥ 45% |
| Solomon et al[33] | PARAMOUNT | Sacubitril/Valsartan | ≥ 45% |
| Solomon et al[34] | PARAGON HF | Sacubitril/Valsartan | ≥ 45% |
| Pieske et al[35] | SOCRATES-PRESERVED | Vericiguat | ≥ 45% |
| Armstrong et al[36] | VITALITY-HFpEF | Vericiguat | ≥ 45% |
| Anker et al[15] | EMPEROR-PRESERVED | Empagliflozin | > 40% |
| Solomon et al[37] | DELIVER trial | Dapagliflozin | > 40% |
| Meta-analysis | |||
| Meta-analysis Global Group in Chronic Heart Failure[38] | MAGGIC | - | ≥ 50 |
| Zheng et al[39] | Systematic review and meta-analysis | Neurohormonal inhibitors | ≥ 40% |
LVEF-based classification of HF phenotypes has served well over the years. However, HF is such a complex syndrome that no single marker can be used to classify those patients. Accumulating data from recent studies show that markers of contractility such as longitudinal strain[19] and cardiac power[20] outperform the LVEF. The incorporation of artificial intelligence (AI) in diagnostic modalities, outcome predictions, and management of HF (individualized precision medicine) constitutes a major development in the field of cardiovascular medicine. In this regard, developing and validating universally accepted scoring systems based on AI would be a fruitful area of research. The LVEF has been considered the holy grail for HF classification treatment guidance for years. The time for change has come, unless one wants to justify those claiming that most published research findings are false[21].
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta P, United States; Hong X, China; Kharlamov AN, Netherlands; Patel L, United States; Wang T, China S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang H
| 1. | Katz AM, Rolett EL. Heart failure: when form fails to follow function. Eur Heart J. 2016;37:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 90] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | Henning RJ. Diagnosis and treatment of heart failure with preserved left ventricular ejection fraction. World J Cardiol. 2020;12:7-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 3. | Becher PM, Fluschnik N, Blankenberg S, Westermann D. Challenging aspects of treatment strategies in heart failure with preserved ejection fraction: "Why did recent clinical trials fail? World J Cardiol. 2015;7:544-554. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Hudson S, Pettit S. What is 'normal' left ventricular ejection fraction? Heart. 2020;106:1445-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147-e239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4116] [Cited by in RCA: 4656] [Article Influence: 388.0] [Reference Citation Analysis (1)] |
| 6. | NHFA CSANZ Heart Failure Guidelines Working Group; Atherton JJ, Sindone A, De Pasquale CG, Driscoll A, MacDonald PS, Hopper I, Kistler PM, Briffa T, Wong J, Abhayaratna W, Thomas L, Audehm R, Newton P, O'Loughlin J, Branagan M, Connell C. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Guidelines for the Prevention, Detection, and Management of Heart Failure in Australia 2018. Heart Lung Circ. 2018;27:1123-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 293] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 7. | Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, Anker SD, Atherton J, Böhm M, Butler J, Drazner MH, Felker GM, Filippatos G, Fonarow GC, Fiuzat M, Gomez-Mesa JE, Heidenreich P, Imamura T, Januzzi J, Jankowska EA, Khazanie P, Kinugawa K, Lam CSP, Matsue Y, Metra M, Ohtani T, Francesco Piepoli M, Ponikowski P, Rosano GMC, Sakata Y, SeferoviĆ P, Starling RC, Teerlink JR, Vardeny O, Yamamoto K, Yancy C, Zhang J, Zieroth S. Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 600] [Cited by in RCA: 475] [Article Influence: 118.8] [Reference Citation Analysis (0)] |
| 8. | McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599-3726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8225] [Cited by in RCA: 7289] [Article Influence: 1822.3] [Reference Citation Analysis (0)] |
| 9. | Lam CSP, Solomon SD. Classification of Heart Failure According to Ejection Fraction: JACC Review Topic of the Week. J Am Coll Cardiol. 2021;77:3217-3225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 10. | Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1-39.e14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6446] [Cited by in RCA: 9343] [Article Influence: 934.3] [Reference Citation Analysis (0)] |
| 11. | Harkness A, Ring L, Augustine DX, Oxborough D, Robinson S, Sharma V. Normal reference intervals for cardiac dimensions and function for use in echocardiographic practice: a guideline from the British Society of Echocardiography. Echo Res Pract. 2020;7:X1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 12. | Wehner GJ, Jing L, Haggerty CM, Suever JD, Leader JB, Hartzel DN, Kirchner HL, Manus JNA, James N, Ayar Z, Gladding P, Good CW, Cleland JGF, Fornwalt BK. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur Heart J. 2020;41:1249-1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 197] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 13. | Stewart S, Playford D, Scalia GM, Currie P, Celermajer DS, Prior D, Codde J, Strange G; NEDA Investigators. Ejection fraction and mortality: a nationwide register-based cohort study of 499 153 women and men. Eur J Heart Fail. 2021;23:406-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 88] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 14. | Gebhard C, Maredziak M, Messerli M, Buechel RR, Lin F, Gransar H, Achenbach S, Al-Mallah MH, Andreini D, Bax JJ, Berman DS, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Chinnaiyan K, Chow BJW, Cury RC, DeLago A, Feuchtner G, Hadamitzky M, Hausleiter J, Kim YJ, Leipsic J, Maffei E, Marques H, Gonçalves PA, Pontone G, Raff GL, Rubinshtein R, Shaw LJ, Villines TC, Lu Y, Jones EC, Peña JM, Min JK, Kaufmann PA. Increased long-term mortality in women with high left ventricular ejection fraction: data from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) long-term registry. Eur Heart J Cardiovasc Imaging. 2020;21:363-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 15. | Anker SD, Butler J, Filippatos G, Ferreira JP, Bocchi E, Böhm M, Brunner-La Rocca HP, Choi DJ, Chopra V, Chuquiure-Valenzuela E, Giannetti N, Gomez-Mesa JE, Janssens S, Januzzi JL, Gonzalez-Juanatey JR, Merkely B, Nicholls SJ, Perrone SV, Piña IL, Ponikowski P, Senni M, Sim D, Spinar J, Squire I, Taddei S, Tsutsui H, Verma S, Vinereanu D, Zhang J, Carson P, Lam CSP, Marx N, Zeller C, Sattar N, Jamal W, Schnaidt S, Schnee JM, Brueckmann M, Pocock SJ, Zannad F, Packer M; EMPEROR-Preserved Trial Investigators. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021;385:1451-1461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3009] [Cited by in RCA: 2785] [Article Influence: 696.3] [Reference Citation Analysis (0)] |
| 16. | Naito R, Kasai T. Sodium glucose cotransporter 2 inhibitors: New horizon of the heart failure pharmacotherapy. World J Cardiol. 2021;13:464-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lupón J, Gavidia-Bovadilla G, Ferrer E, de Antonio M, Perera-Lluna A, López-Ayerbe J, Domingo M, Núñez J, Zamora E, Moliner P, Santiago-Vacas E, Santesmases J, Bayés-Genis A. Heart Failure With Preserved Ejection Fraction Infrequently Evolves Toward a Reduced Phenotype in Long-Term Survivors. Circ Heart Fail. 2019;12:e005652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 64] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 18. | Paulus WJ. Phenotypic Persistence in Heart Failure With Preserved Ejection Fraction. Circ Heart Fail. 2019;12:e005956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Carrasco-Ruiz MF, Ruiz-Rivera A, Soriano-Ursúa MA, Martinez-Hernandez C, Manuel-Apolinar L, Castillo-Hernandez C, Guevara-Balcazar G, Farfán-García ED, Mejia-Ruiz A, Rubio-Gayosso I, Perez-Capistran T. Global longitudinal strain is superior to ejection fraction for detecting myocardial dysfunction in end-stage renal disease with hyperparathyroidism. World J Cardiol. 2022;14:239-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Smiseth OA, Aalen JM, Skulstad H. Heart failure and systolic function: time to leave diagnostics based on ejection fraction? Eur Heart J. 2021;42:786-788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2:e124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6269] [Cited by in RCA: 4998] [Article Influence: 249.9] [Reference Citation Analysis (0)] |
| 22. | Yancy CW, Lopatin M, Stevenson LW, De Marco T, Fonarow GC; ADHERE Scientific Advisory Committee and Investigators. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol. 2006;47:76-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 688] [Cited by in RCA: 733] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 23. | Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, O'Connor CM, Sun JL, Yancy CW, Young JB; OPTIMIZE-HF Investigators and Hospitals. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF Registry. J Am Coll Cardiol. 2007;50:768-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 743] [Cited by in RCA: 852] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 24. | Steinberg BA, Zhao X, Heidenreich PA, Peterson ED, Bhatt DL, Cannon CP, Hernandez AF, Fonarow GC; Get With the Guidelines Scientific Advisory Committee and Investigators. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126:65-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 657] [Article Influence: 50.5] [Reference Citation Analysis (0)] |
| 25. | Yusuf S, Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J; CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362:777-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2143] [Cited by in RCA: 2105] [Article Influence: 95.7] [Reference Citation Analysis (0)] |
| 26. | Cleland JG, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J; PEP-CHF Investigators. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J. 2006;27:2338-2345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1024] [Cited by in RCA: 1050] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 27. | Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, Anderson S, Donovan M, Iverson E, Staiger C, Ptaszynska A; I-PRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359:2456-2467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1395] [Cited by in RCA: 1442] [Article Influence: 84.8] [Reference Citation Analysis (0)] |
| 28. | van Veldhuisen DJ, Cohen-Solal A, Böhm M, Anker SD, Babalis D, Roughton M, Coats AJ, Poole-Wilson PA, Flather MD; SENIORS Investigators. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol. 2009;53:2150-2158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 393] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 29. | Redfield MM, Chen HH, Borlaug BA, Semigran MJ, Lee KL, Lewis G, LeWinter MM, Rouleau JL, Bull DA, Mann DL, Deswal A, Stevenson LW, Givertz MM, Ofili EO, O'Connor CM, Felker GM, Goldsmith SR, Bart BA, McNulty SE, Ibarra JC, Lin G, Oh JK, Patel MR, Kim RJ, Tracy RP, Velazquez EJ, Anstrom KJ, Hernandez AF, Mascette AM, Braunwald E; RELAX Trial. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2013;309:1268-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 856] [Cited by in RCA: 937] [Article Influence: 78.1] [Reference Citation Analysis (0)] |
| 30. | Yamamoto K, Origasa H, Hori M; J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (J-DHF). Eur J Heart Fail. 2013;15:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 273] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 31. | Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, Love TE, Aronow WS, Adams KF Jr, Gheorghiade M. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. 2006;114:397-403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 482] [Cited by in RCA: 443] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 32. | Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Harty B, Heitner JF, Kenwood CT, Lewis EF, O'Meara E, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, Yang S, McKinlay SM; TOPCAT Investigators. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1656] [Cited by in RCA: 1956] [Article Influence: 177.8] [Reference Citation Analysis (0)] |
| 33. | Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, Shi V, Bransford T, Takeuchi M, Gong J, Lefkowitz M, Packer M, McMurray JJ; Prospective comparison of ARNI with ARB on Management Of heart failUre with preserved ejectioN fracTion (PARAMOUNT) Investigators. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet. 2012;380:1387-1395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 831] [Cited by in RCA: 894] [Article Influence: 68.8] [Reference Citation Analysis (0)] |
| 34. | Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Claggett B, Jhund PS, Boytsov SA, Comin-Colet J, Cleland J, Düngen HD, Goncalvesova E, Katova T, Kerr Saraiva JF, Lelonek M, Merkely B, Senni M, Shah SJ, Zhou J, Rizkala AR, Gong J, Shi VC, Lefkowitz MP; PARAGON-HF Investigators and Committees. Angiotensin-Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N Engl J Med. 2019;381:1609-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1097] [Cited by in RCA: 1611] [Article Influence: 268.5] [Reference Citation Analysis (0)] |
| 35. | Pieske B, Maggioni AP, Lam CSP, Pieske-Kraigher E, Filippatos G, Butler J, Ponikowski P, Shah SJ, Solomon SD, Scalise AV, Mueller K, Roessig L, Gheorghiade M. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur Heart J. 2017;38:1119-1127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 216] [Cited by in RCA: 275] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 36. | Armstrong PW, Lam CSP, Anstrom KJ, Ezekowitz J, Hernandez AF, O'Connor CM, Pieske B, Ponikowski P, Shah SJ, Solomon SD, Voors AA, She L, Vlajnic V, Carvalho F, Bamber L, Blaustein RO, Roessig L, Butler J; VITALITY-HFpEF Study Group. Effect of Vericiguat vs Placebo on Quality of Life in Patients With Heart Failure and Preserved Ejection Fraction: The VITALITY-HFpEF Randomized Clinical Trial. JAMA. 2020;324:1512-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 208] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 37. | Solomon SD, de Boer RA, DeMets D, Hernandez AF, Inzucchi SE, Kosiborod MN, Lam CSP, Martinez F, Shah SJ, Lindholm D, Wilderäng U, Öhrn F, Claggett B, Langkilde AM, Petersson M, McMurray JJV. Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial. Eur J Heart Fail. 2021;23:1217-1225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 213] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 38. | Meta-analysis Global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;33:1750-1757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 548] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 39. | Zheng SL, Chan FT, Nabeebaccus AA, Shah AM, McDonagh T, Okonko DO, Ayis S. Drug treatment effects on outcomes in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Heart. 2018;104:407-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 102] [Article Influence: 12.8] [Reference Citation Analysis (0)] |