Published online Jun 26, 2022. doi: 10.4330/wjc.v14.i6.363
Peer-review started: December 9, 2021
First decision: January 25, 2022
Revised: March 18, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: June 26, 2022
Processing time: 193 Days and 2.6 Hours
Hypertension, hyperglycemia and hypertriglyceridemia are chronic conditions associated with cardiometabolic diseases. Certain anthropometric indices are known to predict them.
To investigate the association of anthropometric indices with these chronic diseases and which anthropometric index predicts them best.
In this study, 221 apparently healthy individuals who never received treatments for cardiovascular disease (CVD), diabetes or other chronic diseases participated. The age of the participants ranged from 20-75 years with mean age of 36.9 ± 11.4 years. The risk factors of these diseases namely systolic blood pressures (SBP) and diastolic blood pressures (DBP), fasting blood glucose (FBG) and triglycerides (TG) were determined for all the participants using standard clinical procedures. The obesity anthropometric indices, waist circumference, waist-to-height ratio, waist-to-hip ratio and body mass index as well as abdominal height (AH) and body surface index were determined. The association between each of them with the risk factors were determined by the Pearson correlation method.
From the results, it was found that AH showed superiority over the rest for SBP (r = 0.301, P < 0.01), DBP (r = 0.370, P < 0.01), FBG (r = 0.297, P < 0.01) and TG (r = 0.380, P < 0.01). Using the receiver operating characteristic curves, cut-off values of AH for SBP, DBP, FBG and TG were determined to be 24.75 cm, 24.75 cm, 25.25 cm and 24.75 cm respectively.
The indices of anthropometry used in this study correlated significantly with the studied CVD risk factors, with AH emerging as the most predictive.
Core Tip: In this work, we used common anthropometric indices and some novel ones to correlate with cardiometabolic diseases in an attempt to identify the best anthropometric index that accurately predicts risk of cardiometabolic diseases in apparently normal individuals.
- Citation: Sirisena A, Okeahialam B. Association of obesity anthropometric indices with hypertension, diabetes mellitus and hypertriglyceridemia in apparently healthy adult Nigerian population. World J Cardiol 2022; 14(6): 363-371
- URL: https://www.wjgnet.com/1949-8462/full/v14/i6/363.htm
- DOI: https://dx.doi.org/10.4330/wjc.v14.i6.363
It has been identified that chronic disease conditions such as hypertension, hyperglycemia and hypertriglyceridemia are important public health challenges often encountered in Sub-Saharan Africa and worldwide with hypertension considered a major risk factor leading to stroke, myocardial infarction, heart failure and even ultimate death[1,2]. Metabolic conditions associated with abdominal obesity such as elevated blood pressure, impaired glucose tolerance, insulin resistance and elevated triglycerides (TG) are all contributing factors of metabolic syndrome (MetS) and cardio-metabolic diseases (CMD)[3-5]. For a long time, excess adiposity, especially the visceral fat is identified as one of the major risk factors of these chronic diseases[6]. Moreover, visceral fat has a more significant impact on diabetes and other related conditions than subcutaneous fat[7]. The fundamental cause of obesity and overweight is an energy imbalance between calories consumed and calories expended. An increased intake of energy-dense food high in fat; and an increase in physical inactivity due to the increasingly sedentary lifestyle is responsible for this energy imbalance[8]. In most population based cardiovascular risk evaluation studies found in the literature, researchers have chosen two or more of traditional obesity anthropometric indices among waist circumference (WC), waist-to-height ratio (WHtR), waist-to-hip ratio (WHR) and body mass index (BMI) to establish the risk level of car
After signing the consent form, the participants were given a questionnaire to fill indicating their sex, age, state of origin, smoking status (Yes or No), alcohol use (Yes or No), physical inactivity (Yes or No) and the family history of CVD (Yes or No). For the measurements to determine the anthropometric indices, Hana bathroom scale, a stadiometer, a non-flexible measuring tape and an abdominometer were used. The blood pressures were measured with an Omron M2 basic automatic digital blood pressure monitor while fasting blood glucose (FBG) and TG were determined with an SD lipidocare dual analyzer.
Study design: A cross-section of apparently healthy adult Nigerians of multiple ethnicity participated in this study. All participants recruited for this study reside in Jos, which is the capital of Plateau State of Nigeria. By “apparently healthy” we meant people who assume themselves to be healthy because they feel no symptoms although they had never done routine medical check-ups or taken any type of medications for chronic diseases such as hypertension, DM and MetS in their life time. They may well be in some form of cardiometabolic disease incubation depending on their age, physical attributes and lifestyle. The minimum sample population size was determined statistically by using the formula, N = (Z2 p q)/X2 to be 196. The prevalence of cardiometabolic diseases in Nigeria as reported in a previous literature was taken to be 15%[21]. This study was carried out at the Jos University Teaching Hospital, Jos, Nigeria after obtaining the ethical clearance from the hospital’s ethical committee. Informed and written consents were obtained from each of the participants of this study. Demographic, behavioral and other risk factor information needed in this study were obtained by administering a questionnaire.
Inclusion criteria: Only the apparently healthy staff and students in Jos University Teaching Hospital who never received treatments for CVD, Diabetes or other chronic diseases were included in this study. The minimum age to qualify for this study was 18 years.
Exclusion criteria: Pregnant women and children were excluded from this study.
Ethical consideration: The study design and protocols were duly approved by the Ethical Committee of the Jos University Teaching Hospital, Jos; and the study lasted between August 2015 to January 2016.
Measurements of anthropometric indices: The body mass was measured using a Hana bathroom scale to the nearest 0.5 kg with subjects wearing light clothes as much as possible with empty pockets standing erect on the scale with both legs well placed on it without shoes. The height measurement was taken as the subject stands erect without shoes on a stadiometer in centimeters. Waist and hip circumferences were measured using a non-flexible tape in centimeters to the nearest 0.1 cm. WC was measured at the end of a normal expiration with arms relaxed at the sides over the light clothing in standing position at the mid-point between the lower margin of the last palpable rib and the top of the iliac crest. Hip circumference was measured with tape wrapped around the maximum circumference of the buttocks with the subjects standing with their feet together with body weight evenly distributed over the feet. WHR was determined by the ratio between the waist and the hip circumferences. Similarly, WHtR was determined by the ratio between the WC and height. The BMI and BSI were computed by dividing the body mass (kg) by the square of height (m2) and dividing the body mass (kg) by the body surface area (m2)[20]. The AH was measured using a locally constructed wooden instrument ‘abdominometer’ in centimeters with an accuracy of 0.5 cm by placing the instrument at the level of iliac crest which corresponds to the space between 4th and 5th lumber vertebrate and the anterior abdominal wall at the level of umbilicus as the subject stands erect[19].
Measurements of blood pressures: Both systolic and diastolic blood pressures (DBP) were measured using an Omron M2 Basic automatic digital blood pressure monitor. The subjects were asked to sit without crossing legs on a chair quietly and place his/her hands on the table after resting in a sitting position for about 15 min. The inflating cuff was fixed tightly on the upper left arm making sure that the lower edge of the cuff was placed about 2 cm above the inner side of the elbow joint. The measurements were taken 3 times within a 5-min interval and the average of both systolic and DBP of the last two measurements were recorded according to WHO guidelines[22].
Measurements of TG and FBG: SD lipidocare dual analyzer was used to determine the TG and FBG levels.
High risk cut-off values of risk factors: In clinical practice, hypertension is diagnosed when systolic blood pressure (SBP) ≥ 140 mmHg and DBP ≥ 90 mmHg[21]. Hyperglycemia which is also known as DM is clinically established when FBG level ≥ 7.0 mmol/L[23]. Hypertriglyceridemia is also diagnosed from the fasting blood serum when the level of TG ≥ 1.7 mmol/L[24].
Statistical analysis: In this study, all statistical analysis were carried out with IBM SPSS Version 22 software package. Correlations between risk parameters (SBP, DBP, FBG and TG) and obesity anthropometric indices (AH, WC, WHR, BSI, WHtR and BMI) were carried out using Pearson correlation method. Also, the correlation between AH and the rest of the anthropometric indices was determined. The receiver operating characteristic (ROC) curve analysis was used to determine the cut-off values of AH for all the risk parameters including obesity.
In this study, 221 consenting subjects (82 males and 139 females) of aged between 18-75 years with a mean age of 36.9 ± 11.4 years participated. Out of this, 67% were indigenes of Plateau state (Central Nigeria) while the rest of the 33% were from 18 other different states representing the North, South, East and West geographical regions of Nigeria.
From the questionnaires, the percentages of traditional risk factors such as status of smoking, alcohol use, physical inactivity and family history of CVD were found to be 2.3%, 17.2%, 31.7% and 24.4% respectively.
Table 1 shows the number of subjects from the study population and the percentage risk for each of the risk parameters considered in this study including the risk of obesity (BMI ≥ 30.0 kg/m2).
| Risk cut-off of parameter | Number of subjects | Percentage risk |
| SBP ≥ 140 mmHg | 36/221 | 16.3 |
| DBP ≥ 90 mmHg | 22/221 | 10.0 |
| FBG ≥ 7.0 mmol/L | 06/221 | 2.7 |
| TG ≥ 1.7 mmol/L | 42/221 | 19.0 |
| BMI ≥ 30.0 kg/m2 | 62/221 | 28.1 |
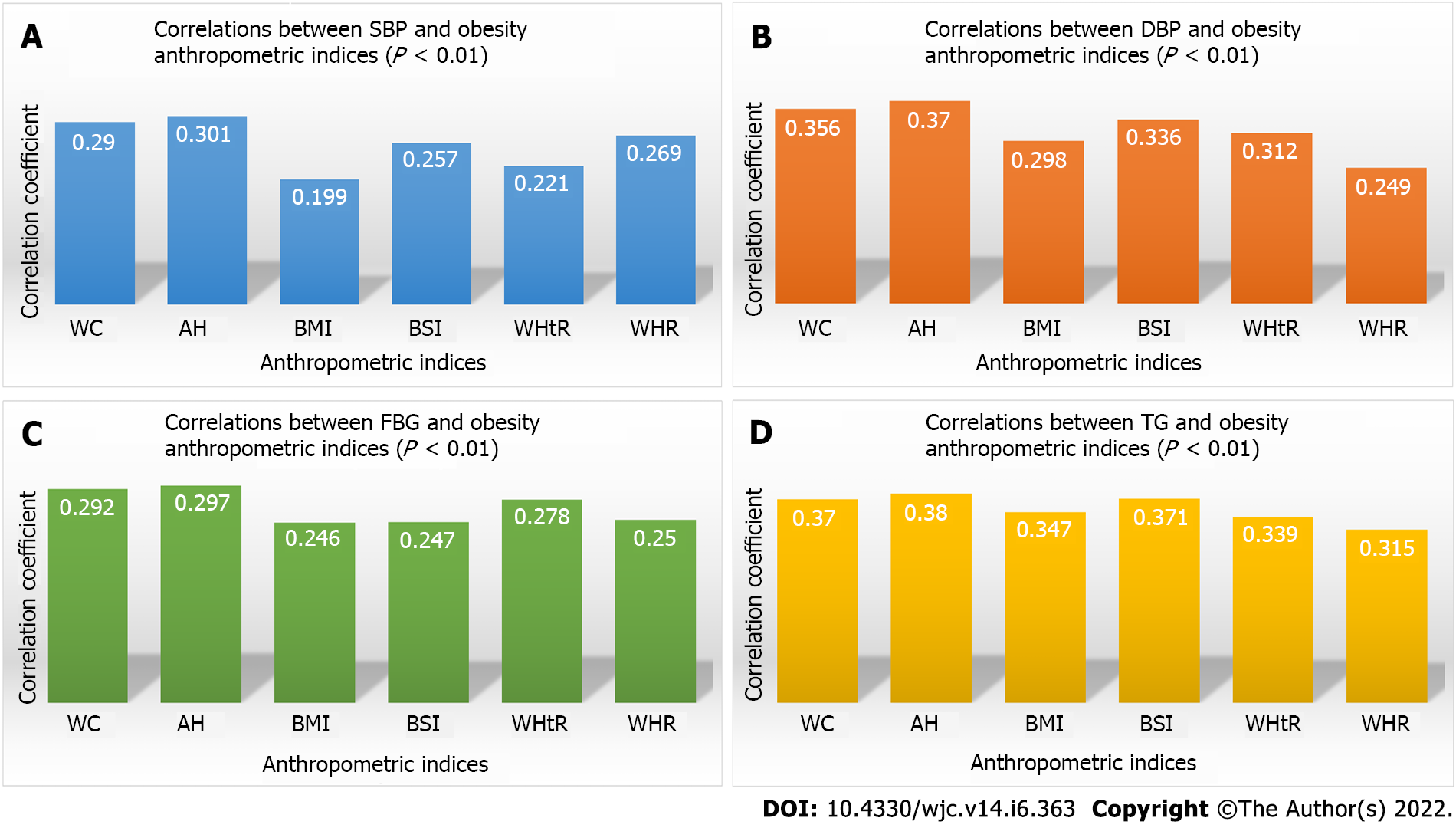
Figure 1 shows the correlations between SBP, DBP, FBG and TG respectively with the selected obesity anthropometric indices.
Table 2 shows the order of correlation coefficients of the anthropometric indices from the highest to the lowest for each of the four risk parameters SBP, DBP, FBG and TG.
| Risk-parameter | Order of correlation with anthropometric indices, highest (1) to lowest (6) | |||||
| 1 | 2 | 3 | 4 | 5 | 6 | |
| SBP | AH | WC | WHR | BSI | WHtR | BMI |
| DBP | AH | WC | BSI | WHtR | BMI | WHR |
| FBG | AH | WC | WHtR | WHR | BSI | BMI |
| Triglycerides | AH | BSI | WC | BMI | WHtR | WHR |
Table 3 shows the Pearson Correlation coefficients and P values between AH and other anthropometric indices used in this study.
| WC | BMI | WHtR | WHR | BSI | |
| AH | 0.944 | 0.872 | 0.905 | 0.682 | 0.892 |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
Table 4 shows the ROC curve analysis with cut-off values of AH for all the risk parameters including obesity.
| Disease condition | Risk value | AH cut-off (cm) | Sensitivity, % | Specificity, % | AUC | 95%CI |
| Hypertension (SBP) | ≥ 140 mmHg | 24.75 | 66.7 | 56.8 | 0.638 | 0.544-0.730 |
| Hypertension (DBP) | ≥ 90 mmHg | 24.75 | 77.3 | 56.3 | 0.664 | 0.551-0.778 |
| Hyperglycemia (FBG) | ≥ 7.0 mmol/L | 25.25 | 66.7 | 58.6 | 0.621 | 0.344-0.899 |
| Hypertriglyceridemia (TG) | ≥ 1.7 mmol/L | 24.75 | 83.3 | 61.5 | 0.751 | 0.675-0.827 |
| Obesity (BMI) | ≥ 30.0 kg/m2 | 25.75 | 85.5 | 79.2 | 0.923 | 0.889-0.957 |
Table 1 shows the summary of the prevalence of risk levels of chronic diseases among the apparently healthy cross section of adult Nigerians chosen in this study. Unknown to them, a significant percentage of these participants were at high risk for CMD. We found that 16.3% of the participants had SBP greater or equal to 140 mmHg while 10.0% had DBP greater or equal to 90 mmHg. However, only 2.7% had hyperglycemia but 19.0% had hypertriglyceridemia. Interestingly, 28.1% of these participants who claimed to be healthy were obese. Correlation coefficients of anthropometric indices WC, AH, BMI, BSI, WHtR and WHR with risk parameters SBP, DBP, FBG and TG were illustrated in Figure 1 and all the correlations were significant at P < 0.01 and showed a positive association between the anthropometric indices and risk parameters. Table 2 shows the order of correlation with each risk parameter from highest to lowest values. It was found that AH is superior to all the other obesity anthropometric indices considered in this study to discriminate hypertension (SBP and DBP), hyperglycemia (FBG) and hypertriglyceridemia (TG). This confirms the findings of an earlier pilot study by Okeahialam et al[25] that AH was superior to BMI in predicting hypertension and diabetes. This present study shows that even for hypertriglyceridemia AH is a better predictive anthropometric index. Although both WHO and American Heart Association recommend the use of WC in screening for cardiometabolic risk[26], in our study WC is positioned as the second best discriminator for SBP, DBP and FBG except for TG where BSI proved to be better. Previous studies also showed that AH, also known as sagittal abdominal diameter (SAD) correlates better with cardiovascular risk factors than WC and BMI[27-29]. However, in these studies SAD was measured with a subject lying in a supine position to allow loose subcutaneous fat to fall to the sides of the subject on the couch and more rigid visceral fat to remain in place to be measured using a caliper instrument. They also reported that the ability of SAD to index abdominal fat and high risk obesity more accurately is greater than that of the WC and BMI. We also noticed that BSI is superior to BMI in discriminating all the risk parameters considered in this study. The other two anthropometric indices WHtR and WHR can also be used as good discriminators of CMD. However, some inaccuracies can occur especially in finding the best anatomical site for WHR measurement[30]. Although all these six anthropometric indices are statistically found suitable for the risk evaluation studies of adult Nigerians, some uncertainties involved in differentiating of visceral fat from subcutaneous fat and abdominal obesity from general obesity can hinder the accuracy of these traditional anthropometric indices in diagnosing cardiometabolic diseases. Therefore, we propose AH to be the best discriminator of CMD for adult Nigerians in this locality taking into consideration both statistical superiority and clinical acceptability due to its ability to measure visceral fat more accurately. Table 3 shows the association of AH with the other five anthropometric indices. Incidentally, AH also shows very strong and positive correlations with all the other indices: WC (0.944), WHtR (0.905), BSI (0.892), BMI (0.872) and WHR (0.682). This shows the strong relationship of AH over the other anthropometric indices considered in this study for risk evaluations of CMD. From the ROC curve analysis, we found the cut-off values, area under the curve, 95% confidence interval of AH for all the risk parameters SBP, DBP, FBG, TG and obesity (using the BMI scale) as shown in Table 4. We established that the risk cut-off value of AH ≥ 24.75 cm for both hypertension and hypertriglyceridemia and AH ≥ 25.25 cm for hyperglycemia. Using BMI ≥ 30.0 kg/m2 as the risk value of obesity, the cut-off value of obesity is found to be AH ≥ 25.75 cm. This means that, going by our findings, cardiometabolic disease risk can occur without a person being classified as obese going by WHO BMI values.
From this study, we have attempted to establish the clinical and statistical significance of the AH measured when a subject is standing in erect position at ease with our abdominometer in risk evaluation of cardiometabolic diseases over the other existing traditional obesity anthropometric indices such as WC, WHtR, WHR and BMI. Moreover, we also found that the BSI can be a better index than the BMI for cardiometabolic risk evaluations as a general obesity anthropometric index.
Using this simple AH measurements, large scale community based population studies were recommended to predict and separate high risk individuals for possible life style modification procedures, clinical interventions and treatments to minimize the mortality and morbidity rates of cardiometabolic diseases as preventive measures. This is necessary given the relatively small size of our sample and the convenience approach to sampling; in order to improve external validity.
For decades, body mass index (BMI) has been the most widely accepted index of adiposity and most commonly used for defining obesity recommended by the WHO but it can be affected by age, gender, and ethnicity.
In most population-based cardiovascular risk assessment studies found in the literature, researchers selected two or more of traditional obesity among waist circumference, waist-to-height ratio, waist-to-hip ratio, and body mass index. Anthropometric measures (BMI) to determine the level of card
We sought to identify the best anthropometric index predictive of each of the disease conditions; hypertension, diabetes mellitus and hypertriglyceridemia for our chosen cross-sectional population study group and to determine their respective cut-off values.
This was a cross-sectional study that included 221 consenting apparently healthy adult Nigerians 18 years and above who were not pregnant at enrolment. After signing the consent form, the participants were given a questionnaire to fill indicating their sex, age, state of origin, smoking status (Yes or No), alcohol use (Yes or No), physical inactivity (Yes or No) and the family history of CVD (Yes or No). Height and weight were measured as well as the other anthropometric indices using a measuring tape and an abdominometer. The blood pressures were measured with an Omron M2 basic automatic digital blood pressure monitor while fasting blood glucose and triglycerides were determined with an SD lipidocare dual analyzer.
In this study, 221 consenting subjects (82 males and 139 females) of aged between 18-75 years with a mean age of 36.9 ± 11.4 years participated. From the questionnaires, the percentages of traditional risk factors such as status of smoking, alcohol use, physical inactivity and family history of CVD were found to be 2.3%, 17.2%, 31.7% and 24.4% respectively.
Anthropometric measures used in this study were significantly associated with the CVD risk factors studied, with abdominal height (AH) emerging as the most predictive measure.
Using this simple measure of AH, large-scale community population studies are recommended to predict and differentiate high-risk individuals for possible lifestyle modification procedures, clinical interventions, and treatments to minimize cardiometabolic mortality and mortality. Morbidity as a preventive measure. This is necessary given our relatively small sample size and convenient sampling method.
The input of Professors Emeka Ike and Nestor Chagok in the course of this work is hereby acknowledged.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Nigeria Cardiac Society; Panafrican Society of Cardiology; American Heart Association.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Nigeria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: He Z, China; Wang T, China A-Editor: Ma YJ, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Huang XB, Zhang Y, Wang TD, Liu JX, Yi YJ, Liu Y, Xu RH, Hu YM, Chen M. Prevalence, awareness, treatment, and control of hypertension in southwestern China. Sci Rep. 2019;9:19098. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Udenze IC, Amadi CE. Cardiovascular disease risk assessment in Nigerian adults with type 2 diabetes and metabolic syndrome using the Framingham's risk score. Int J Noncommun Dis. 2018;3:15-20. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Papakonstantinou E, Lambadiari V, Dimitriadis G, Zampelas A. Metabolic syndrome and cardiometabolic risk factors. Curr Vasc Pharmacol. 2013;11:858-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Amirabdollahian F, Haghighatdoost F. Anthropometric Indicators of Adiposity Related to Body Weight and Body Shape as Cardiometabolic Risk Predictors in British Young Adults: Superiority of Waist-to-Height Ratio. J Obes. 2018;2018:8370304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 5. | Aghakhanian F, Wong C, Tan JSY, Yeo LF, Ramadas A, Edo J, Hoh BP, Khalid BAK, Phipps ME. Metabolic syndrome and cardiometabolic risk factors among indigenous Malaysians. Public Health. 2019;176:106-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Wang F, Chen Y, Chang Y, Sun G, Sun Y. New anthropometric indices or old ones: which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc Disord. 2018;18:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 7. | Lee JJ, Beretvas SN, Freeland-Graves JH. Abdominal adiposity distribution in diabetic/prediabetic and nondiabetic populations: a meta-analysis. J Obes. 2014;2014:697264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Regi M, Sharma N. Body Adiposity Index vs Body Mass Index and Other Anthropometric Traits as Correlates of Cardiovascular Disease. Int J Noncommun Dis. 2016;3:110-131. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 9. | Obesity in Asia Collaboration. Is central obesity a better discriminator of the risk of hypertension than body mass index in ethnically diverse populations? J Hypertens. 2008;26:169-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1-452. [PubMed] |
| 11. | Beydoun MA, Wang Y. Gender-ethnic disparity in BMI and waist circumference distribution shifts in US adults. Obesity (Silver Spring). 2009;17:169-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol. 2008;61:646-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 680] [Cited by in RCA: 767] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 13. | Zimmet P, Magliano D, Matsuzawa Y, Alberti G, Shaw J. The metabolic syndrome: a global public health problem and a new definition. J Atheroscler Thromb. 2005;12:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 577] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 14. | Frankenfield DC, Rowe WA, Cooney RN, Smith JS, Becker D. Limits of body mass index to detect obesity and predict body composition. Nutrition. 2001;17:26-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 320] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 15. | Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012;13:275-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1439] [Cited by in RCA: 1306] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 16. | Wang Z, Hao G, Wang X, Chen Z, Zhang L, Guo M, Tian Y, Shao L, Zhu M. [Current prevalence rates of overweight, obesity, central obesity, and related cardiovascular risk factors that clustered among middle-aged population of China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:354-358. [PubMed] |
| 17. | Manson JE, Bassuk SS. Obesity in the United States: a fresh look at its high toll. JAMA. 2003;289:229-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 104] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Faramarzi E, Ostadrahimi A, Nikniaz Z, Jafarabadi MA, Fakhari A, Somi M. Determination of the Best Anthropometric Index of Obesity for Prediction of Prehypertension and Hypertension in a Large Population - Based - Study; the Azar- Cohort. Iran Red Crescent Med J. 2018;20:e59911, 1-8. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Okeahialam BN, Diala UM, Uwakwe J, Ejeh I, Ozoilo U. Utility of the Abdominometer: A Novel Contribution to Cardiovascular Anthropometry. Food Sci Nutr. 2015;6:1202-1207. [DOI] [Full Text] |
| 20. | Ferreira F, Duarte JA. Accuracy of body mass index, waist circumference and body surface index to characterize overweight and obesity in adolescents. Arc Exercise Heal Dis. 2014;4:299-306. [DOI] [Full Text] |
| 21. | Supiyev A, Kossumov A, Utepova L, Nurgozhin T, Zhumadilov Z, Bobak M. Prevalence, awareness, treatment and control of arterial hypertension in Astana, Kazakhstan. A cross-sectional study. Public Health. 2015;129:948-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 22. | World Health Organization. World Health Statistics, WHO, Geneva. [cited 10 December 2021]. Available from: https://apps.who.int/iris/handle/10665/43890. |
| 23. | Supiyev A, Kossumov A, Kassenova A, Nurgozhin T, Zhumadilov Z, Peasey A, Bobak M. Diabetic prevalence, awareness and treatment and their correlation in older persons in urban and rural population in the Astana region, Kazakhistan. Diabtes Res Clin Pract. 2016;112:6-12. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Parhofer KG, Laufs U. The Diagnosis and Treatment of Hypertriglyceridemia. Dtsch Arztebl Int. 2019;116:825-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 25. | Okeahialam BN, Diala UM, Uwakwe J, Ejeh I, Ozoilo U. Abdominal height measures cardiometabolic risk better than body mass index: result of a preliminary study. JMR. 2016;2:149-151. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Fan H, Li X, Zheng L, Chen X, Lan Q, Wu H, Ding X, Qian D, Shen Y, Yu Z, Fan L, Chen M, Tomlinson B, Chan P, Zhang Y, Liu Z. Abdominal obesity is strongly associated with Cardiovascular Disease and its Risk Factors in Elderly and very Elderly Community-dwelling Chinese. Sci Rep. 2016;6:21521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 27. | Firouzi SA, Tucker LA, LeCheminant JD, Bailey BW. Sagittal Abdominal Diameter, Waist Circumference, and BMI as Predictors of Multiple Measures of Glucose Metabolism: An NHANES Investigation of US Adults. J Diabetes Res. 2018;2018:3604108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | de Souza NC, de Oliveira EP. Sagittal abdominal diameter shows better correlation with cardiovascular risk factors than waist circumference and BMI. J Diabetes Metab Disord. 2013;12:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Pajunen P, Rissanen H, Laaksonen MA, Heliövaara M, Reunanen A, Knekt P. Sagittal abdominal diameter as a new predictor for incident diabetes. Diabetes Care. 2013;36:283-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Macek P, Biskup M, Terek-Derszniak M, Krol H, Smok-Kalwat J, Gozdz S, Zak M. Optimal cut-off values for anthropometric measures of obesity in screening for cardiometabolic disorders in adults. Sci Rep. 2020;10:11253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |