Published online Nov 26, 2021. doi: 10.4330/wjc.v13.i11.599
Peer-review started: March 23, 2021
First decision: July 30, 2021
Revised: August 6, 2021
Accepted: October 25, 2021
Article in press: October 25, 2021
Published online: November 26, 2021
Processing time: 246 Days and 10.5 Hours
The prevalence of coronary artery disease (CAD) increases in patients with end-stage liver disease, with part of them receiving the percutaneous coronary intervention (PCI) as a treatment option. Dual antiplatelet therapy (DAPT), a standard of care after PCI, could result in catastrophic consequences in this population. Before PCI and the start of DAPT, it is recommended to assess patient bleeding risk. Based on novel findings, liver cirrhosis does not necessarily lead to a significant increase in bleeding complications. Furthermore, conventional methods, such as the international normalized ratio, might not be appropriate in assessing individual bleeding risk. The highest bleeding risk among cirrhotic patients has a subgroup with severe thrombocytopenia (< 50 × 109/L) and elevated portal pressure. Therefore, every effort should be made to maintain thrombocyte count above > 50 × 109/L and prevent variceal bleeding. There is no solid evidence for DAPT in patients with cirrhosis. However, randomized trials investigating short (one month) DAPT duration after PCI with new drug-eluting stents (DES) in a high bleeding risk patient population can be implemented in patients with cirrhosis. Based on retrospective studies (with older stents and protocols), PCI and DAPT appear to be safe but with a higher risk of bleeding complications with longer DAPT usage. Finally, novel methods in assessing CAD severity should be performed to avoid unnecessary PCI and potential risks associated with DAPT. When indicated, PCI should be performed over radial artery using contemporary DES. Complementary medical therapy, such as proton pump inhibitors and beta-blockers, should be prescribed for lower bleeding risk patients. Novel approaches, such as thromboelastography and “preventive” upper endoscopies in PCI circumstances, warn clinical confirmation.
Core Tip: Dual antiplatelet therapy (DAPT) is necessary after a percutaneous coronary intervention (PCI). However, it could result in severe consequences in patients with liver cirrhosis. Based on novel findings, liver cirrhosis does not necessarily lead to a significant increase in bleeding complications. Patients with cirrhosis who have the highest bleeding risk are those with severe thrombocytopenia and elevated portal pressure. Despite the lack of solid evidence for DAPT in patients with cirrhosis, trials investigating one month of DAPT duration after PCI can be implemented in cirrhotic patients. Before PCI, functional assessment of coronary artery disease severity should be performed to avoid unnecessary interventions.
- Citation: Ostojic Z, Ostojic A, Bulum J, Mrzljak A. Safety and efficacy of dual antiplatelet therapy after percutaneous coronary interventions in patients with end-stage liver disease. World J Cardiol 2021; 13(11): 599-607
- URL: https://www.wjgnet.com/1949-8462/full/v13/i11/599.htm
- DOI: https://dx.doi.org/10.4330/wjc.v13.i11.599
The prevalence of coronary artery disease (CAD) in patients with liver cirrhosis is estimated from 20% to 26%[1-3]. Furthermore, due to the growing incidence of cirrhosis caused by non-alcoholic fatty liver disease, which has overlapping risk factors with the CAD, an even higher prevalence of CAD in patients with cirrhosis can be expected[4,5]. The presence of both comorbidities can limit treatment options for each. For example, a patient can be rejected for surgical heart revascularization due to high operative risk or for the potential liver transplantation (LT) due to unresolved CAD. Percutaneous coronary intervention (PCI) with stent implantation represents a valid treatment option for CAD[6]. Data from the United States report that 1.2% of patients undergoing PCI have cirrhosis[7]. However, dual antiplatelet therapy (DAPT), a standard of care after stent implantation, can have severe consequences in cirrhotic patients with cirrhosis due to elevated bleeding risk.
This article aims to define; do all patients with liver cirrhosis have the same bleeding risk, the evidence behind DAPT in patients with cirrhosis, and what can be done to lower bleeding risk in such patients.
In the past, all patients with liver cirrhosis were classified as having high bleeding risk (HBR) due to coagulation abnormalities, thrombocytopenia, and elevated portal pressure-related complications. However, these presumptions are changing with growing evidence that, at least, part of patients with cirrhosis might have a high thrombotic risk[8,9]. Complex alterations in the hemostatic system cause so-called rebalanced hemostasis, meaning that impaired protein synthesis leads to a decreased level of procoagulant factors and anticoagulant factors[10,11]. The international normalized ratio (INR) is often used as a parameter for coagulation cascade competence in cirrhosis, although primarily invented for the warfarin dosing and not for the above mentioned[9]. The potential problem arises from the fact that it measures procoagulant factors but not anticoagulant factors such as protein C and S, which are also depleted in patients with liver cirrhosis[9,12]. Furthermore, it does not measure Factor VIII, whose levels are elevated in cirrhosis patients due to its endothelial production[13]. Finally, studies that tried to "correct" INR using fresh frozen plasma or activated Factor VII, failed to reduce bleeding events[14-17]. Additionally, fibrinogen measurement has been proposed as a potential alternative to INR for assessing bleeding risk, although its clinical usefulness is yet to be confirmed[9].
The second risk factor for bleeding in patients with cirrhosis is thrombocytopenia, occurring in 64%-84% of patients with cirrhosis or fibrosis[18]. Its cause is multi
The third risk factor for bleeding in patients with cirrhosis are complications arising from portal hypertension, primarily esophageal varices[26,27]. The risk of variceal hemorrhage is related to variceal size, the severity of liver dysfunction (Child-Pugh B/C), and the presence of red wale marks on varices[28]. This issue had been recognized in a consensus document from Academic Research Consortium for High Bleeding Risk, in which they defined patients with cirrhosis and portal hypertension as having HBR after PCI[29]. Of note, in the same document, patients with thrombocytopenia (defined as < 100 × 109/L), irrespective of etiology, and those with chronic bleeding diathesis are likewise defined as having HBR. Finally, it is essential to emphasize there is no valid bleeding risk score for patients with liver cirrhosis. Most used Child-Pugh and Mayo End-Stage Liver Disease criteria are developed for predicting mortality and not bleeding events, despite having INR as an integrative part of both[30-32]. In summary, based on presented data, patients with the highest bleeding risk are those with severe thrombocytopenia (< 50 × 109/L) and those with portal hypertension.
Historically, due to the concerns for late stent thrombosis after drug-eluting stent (DES) implantation, DAPT was recommended for 12 mo after such procedures. Thus, patients with HBR, including those with liver disease, were excluded from most modern DES trials[29]. Therefore, implantation of a bare-metal stent (BMS) followed by one month of DAPT was recommended in those cases[29]. However, with DES technology advancements and stent thrombosis reduction, randomized trials in HBR patients have been performed. In the LEADERS FREE trial, almost 2500 patients were allocated to modern DES or BMS, followed by one month of DAPT. After one year of follow-up, DES implantation was superior to BMS concerning primary safety endpoint [a composite of cardiac death, myocardial infarction (MI), or stent thrombosis] [9.4% vs 12.9%; hazard ratio, 0.71; 95% confidence interval (CI): 0.56-0.91; P < 0.001 for noninferiority and P = 0.005 for superiority] with the lower incidence of clinically driven target lesion revascularization (5.1% vs 9.8%; hazard ratio, 0.50; 95%CI: 0.37-0.69; P < 0.001)[33]. Similarly, in ONYX ONE trial, which included 1996 patients, DES implantation was non-inferior to BMS (both with one month of DAPT) after one year of follow-up[34]. Even though both trials investigated patients with HBR, the prevalence of patients with liver disease/cirrhosis was < 1%, too small to extract conclusions in this patient population[33,34].
Several retrospective studies described and investigated outcomes after PCI in patients with liver cirrhosis compared to different patient populations, with only one of them more focused on antiplatelet management[4,7,35-38]. The largest of them was conducted by Wu et al[35], which included 914 cirrhotic patients who underwent PCI due to MI and compared them to a four times larger propensity-matched group of patients without cirrhosis. The cirrhosis group had significantly higher 1-year mortality (32.7% vs 23.7%, 95%CI: 1.28-1.74) but less recurrent MIs (6.0% vs 8.7%, 95%CI: 0.54-0.92). Importantly, cirrhosis group had non-significant increase in major bleeding (3.7% vs 2.9%, 95%CI: 0.87-1.23) and significantly increased gastrointestinal bleeding (28.0% vs 20.2%, 95%CI: 1.31-1.70). A sub-analysis showed significantly lower mortality and non-significant decreases in recurrent MI in the DAPT subgroup (duration of DAPT had to be > 3 mo) compared to cirrhotic patients on a single antiplatelet agent. However, patients with a single antiplatelet agent were significantly older with significantly more severe comorbidities (such as heart failure and history of gastrointestinal bleeding), so direct comparison is questionable[35]. After PCI in patients with cirrhosis, worse in-hospital mortality than a historic non-cirrhotic group has also been described by Singh et al[7]. In the same study, patients with cirrhosis had worse outcomes if they received BMS instead of DES[7].
The two studies comparing PCI and medical therapy in CAD patients with cirrhosis found no difference in 1-year mortality and a higher bleeding rate[36,37]. Importantly, Krill et al[36] described a temporal change in bleeding events. The difference in bleeding was non-significantly different at 30- and 90-d follow-up (although higher in the PCI group) but become significant after 1 and 2 years. That might be associated with higher and extended use of DAPT in the PCI group (63% of patients had DAPT 1 year after PCI)[36]. Similarly, Russo et al[4] and Azarbal et al[38] described no significant difference in bleeding after PCI than medical therapy, although higher in the PCI group, in shorter follow up of 11 and 1 mo, respectively.
Finally, it is essential to emphasize that the studies mentioned above-included patients up to 2015, with consequent high use of BMS or old generation DES without new DAPT duration protocols.
In conclusion, "hard" evidence for DAPT in patients with liver cirrhosis is scarce. Based on retrospective studies (with older stents and protocols), PCI and DAPT appear to be safe but with a higher risk of bleeding complications with longer DAPT usage.
Based on the aforementioned retrospective studies, PCI's usefulness in patients with liver cirrhosis regarding mortality is questionable due to high non-cardiovascular related mortality[36,37,39]. Therefore, appropriate triage of such patients before PCI, and consequent DAPT related bleeding risk, is mandatory. Based on data in the general population, PCI affects prognosis in patients presenting with MI and selected scenarios of a chronic coronary syndrome such as left main or proximal left anterior descending artery disease, a multi-vessel disease with impaired left ventricular systolic function, and a large area of myocardium at risk[6]. In our opinion, PCI is indicated in a patient with cirrhosis who presents with one of the mentioned scenarios if life expectancy, from the hepatological point of view, is reasonably long (one year) or other treatment modalities, such as LT are available. Except for the scenarios mentioned above, PCI of all significant coronary artery stenosis might be indicated before LT. This conclusion is based on retrospective studies that showed worse outcomes after LT in patients with CAD and increased mortality in multi-vessel CAD cases[40-42]. On the other hand, data from several studies indicate no impact of CAD on post-LT survival if CAD is treated appropriately, including PCI when indicated[43,44]. All presented studies described CAD using plain angiography as the percentage of coronary artery stenosis (usually over 50%). Although this method is valid for CAD definition, more novel and precise methods, such as functional assessment of stenosis, should be done before PCI, especially in borderline stenosis and HBR patients[6]. Therefore, we advise the usage of instantaneous wave-free ratio or a similar method for confirmation of stenosis significance for all coronary artery stenosis estimated to be between 50%-90% as it not only affects prognosis but reduces the number of stents implanted compared to angiogram alone[6,45-47]. In the cases where PCI is indicated, it should be done with third generation DES, preferably with one tested for the short need for DAPT of only one month[6,33,34,48]. Another off-label option would be PCI using drug-coated balloons which has comparable results with modern DES primarily in small CAD (diameter ≤ 2.8 mm) and in HBR patients due to theoretical shorter usage of DAPT and lower risk for thrombosis as no foreign material remains in the artery[49-52]. We advise using the radial artery approach as default vascular access for all left heart catheterization due to better outcomes and lower bleeding risk than transfemoral access[6,53,54]. It also appears to be a safe option in patients with end-stage liver disease based on a single available study[55].
After the PCI, DAPT duration should be shortened in HBR patients, as advised by the guidelines, to three months after elective PCI or six months after PCI in acute coronary syndrome[56]. We also encourage clopidogrel usage compared to more potent P2Y12 inhibitors due to its lower bleeding risk[24,57,58]. A potential drawback of clopidogrel is that it requires activation in the liver[59]. However, a recent study described appropriately reduced platelet function after clopidogrel using thromboelastography (TEG), TEG-based platelet mapping, and impedance platelet aggregometry in patients with decompensated cirrhosis[60]. Importantly, no platelet function test has been studied for guiding DAPT in a patient with cirrhosis. On the other hand, TEG has been used to guide blood product use in various scenarios in patients with cirrhosis and impaired coagulation assessed using conventional methods (INR and platelet count)[61]. In randomized trials, TEG compared to conventional methods led to lower blood products use without an increase in bleeding complications in patients with bleeding varices and before invasive procedures[62,63]. Based on mentioned, TEG can theoretically be used to assess hemostatic pathways before administration of DAPT, with more freely DAPT usage in case of preserved hemostasis. However, these presumptions are supposed to be tested in clinical studies before widespread utilization.
Regarding medical therapy for preventing bleeding complications during DAPT, a proton pump inhibitor should be prescribed as it reduces upper gastrointestinal bleeding in patients with cirrhosis[36,64]. It is also most important to administer a maximally tolerated dose of beta-adrenergic blocking agents due to their positive effect on portal hypertension and CAD[28,65]. Lastly, we encourage repeat upper endoscopy in patients with liver cirrhosis before elective PCI or early after urgent PCI to manage varices according to recommendations for primary and secondary prophylaxis of variceal bleeding, as previously proposed[4,28].
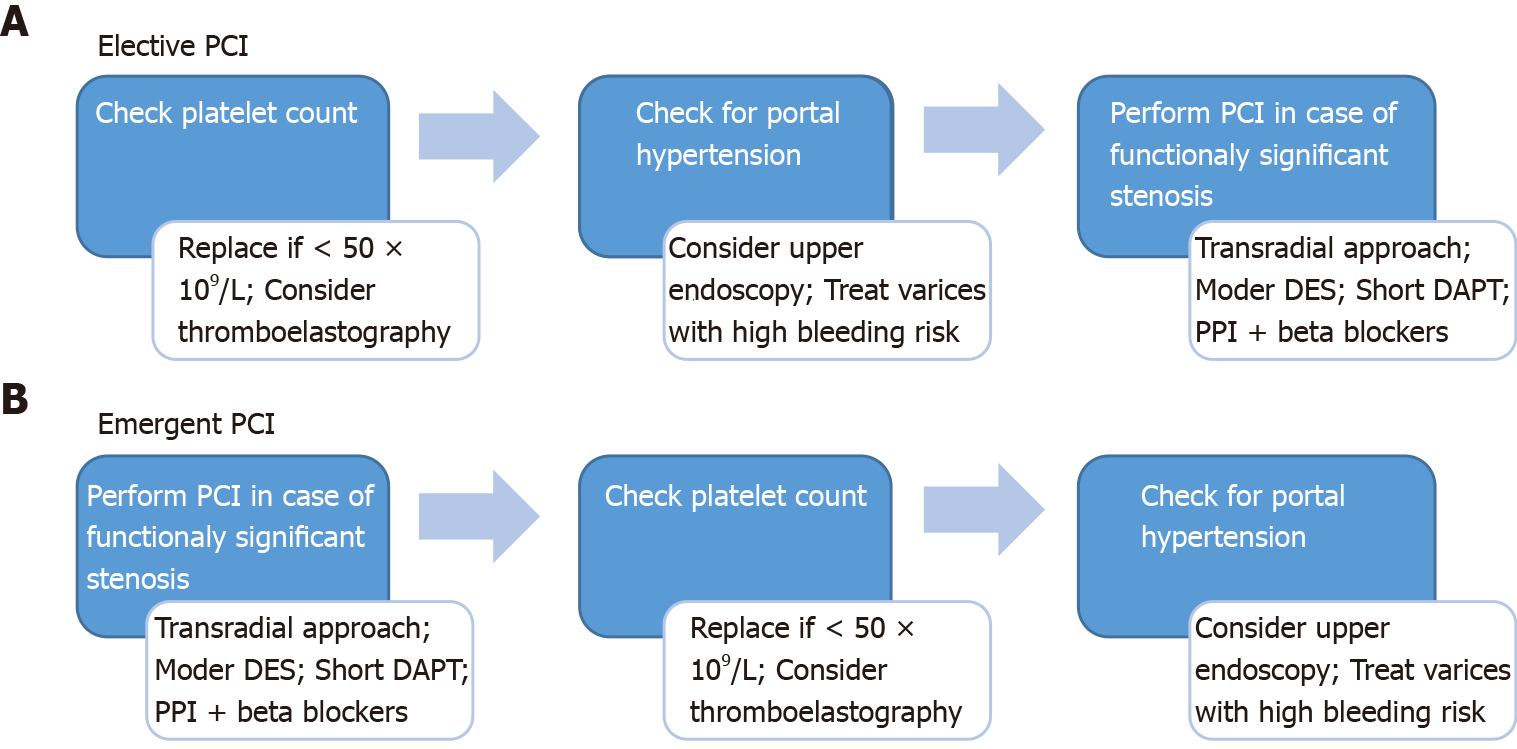
In summary, PCI in patients with cirrhosis should be done over trans-radial artery access, using novel DES (with proved safety in short DAPT protocols), in cases when PCI is proved to affect patient prognosis. Along with DAPT, concomitant medical therapy that reduces the risk of bleeding should be administered. Novel approaches, such as TEG or "preventive" upper endoscopies, although promising, warn clinical conformation. Proposed scheme with the main recommendations of how to approach a patient with cirrhosis undergoing percutaneous coronary intervention in elective and emergent settings is presented in Figure 1.
The highest bleeding risk among patients with liver cirrhosis is present in a subgroup of patients with severe thrombocytopenia and elevated portal pressure. Therefore, every effort should be made to maintain thrombocyte count above > 50 × 109/L and prevent variceal bleeding. Despite the lack of solid evidence for DAPT in patients with cirrhosis, results from trials investigating shorter DAPT duration after PCI in HBR patient population can be implemented in patients with cirrhosis. Finally, novel methods in the assessment of CAD severity should be performed to avoid unnecessary PCI.
Provenance and peer review: Invited article; Externally peer reviewed
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gadour E S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Kalaitzakis E, Rosengren A, Skommevik T, Björnsson E. Coronary artery disease in patients with liver cirrhosis. Dig Dis Sci. 2010;55:467-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 2. | An J, Shim JH, Kim SO, Lee D, Kim KM, Lim YS, Lee HC, Chung YH, Lee YS. Prevalence and prediction of coronary artery disease in patients with liver cirrhosis: a registry-based matched case-control study. Circulation. 2014;130:1353-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 3. | Raval Z, Harinstein ME, Skaro AI, Erdogan A, DeWolf AM, Shah SJ, Fix OK, Kay N, Abecassis MI, Gheorghiade M, Flaherty JD. Cardiovascular risk assessment of the liver transplant candidate. J Am Coll Cardiol. 2011;58:223-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 178] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 4. | Russo MW, Pierson J, Narang T, Montegudo A, Eskind L, Gulati S. Coronary artery stents and antiplatelet therapy in patients with cirrhosis. J Clin Gastroenterol. 2012;46:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Patel SS, Nabi E, Guzman L, Abbate A, Bhati C, Stravitz RT, Reichman T, Matherly SC, Driscoll C, Lee H, Luketic VA, Sterling RK, Sanyal AJ, Patel V, Levy M, Siddiqui MS. Coronary artery disease in decompensated patients undergoing liver transplantation evaluation. Liver Transpl. 2018;24:333-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 6. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2722] [Cited by in RCA: 4491] [Article Influence: 898.2] [Reference Citation Analysis (0)] |
| 7. | Singh V, Patel NJ, Rodriguez AP, Shantha G, Arora S, Deshmukh A, Cohen MG, Grines C, De Marchena E, Badheka A, Ghatak A. Percutaneous Coronary Intervention in Patients With End-Stage Liver Disease. Am J Cardiol. 2016;117:1729-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Vetrovec G, Stravitz RT. Bleeding in Patients With Cirrhosis Undergoing Invasive Cardiovascular Procedures: Do We Overestimate Risk? Circulation. 2020;141:1279-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | O'Leary JG, Greenberg CS, Patton HM, Caldwell SH. AGA Clinical Practice Update: Coagulation in Cirrhosis. Gastroenterology. 2019;157:34-43.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 282] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 10. | Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383:1749-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1139] [Cited by in RCA: 1311] [Article Influence: 119.2] [Reference Citation Analysis (0)] |
| 11. | Tripodi A. Hemostasis abnormalities in cirrhosis. Curr Opin Hematol. 2015;22:406-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 12. | Tripodi A, Primignani M, Lemma L, Chantarangkul V, Mannucci PM. Evidence that low protein C contributes to the procoagulant imbalance in cirrhosis. J Hepatol. 2013;59:265-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 13. | Sinegre T, Duron C, Lecompte T, Pereira B, Massoulier S, Lamblin G, Abergel A, Lebreton A. Increased factor VIII plays a significant role in plasma hypercoagulability phenotype of patients with cirrhosis. J Thromb Haemost. 2018;16:1132-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Qi X, Ye C, Guo X. Recombinant factor VIIa for variceal bleeding in liver cirrhosis: still only a hope. Arch Med Sci. 2017;13:496-499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Bosch J, Thabut D, Bendtsen F, D'Amico G, Albillos A, González Abraldes J, Fabricius S, Erhardtsen E, de Franchis R; European Study Group on rFVIIa in UGI Haemorrhage. Recombinant factor VIIa for upper gastrointestinal bleeding in patients with cirrhosis: a randomized, double-blind trial. Gastroenterology. 2004;127:1123-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 260] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 16. | Tripodi A, Chantarangkul V, Primignani M, Clerici M, Dell'era A, Aghemo A, Mannucci PM. Thrombin generation in plasma from patients with cirrhosis supplemented with normal plasma: considerations on the efficacy of treatment with fresh-frozen plasma. Intern Emerg Med. 2012;7:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Giannini EG, Stravitz RT, Caldwell SH. Correction of hemostatic abnormalities and portal pressure variations in patients with cirrhosis. Hepatology. 2014;60:1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Qamar AA, Grace ND, Groszmann RJ, Garcia-Tsao G, Bosch J, Burroughs AK, Ripoll C, Maurer R, Planas R, Escorsell A, Garcia-Pagan JC, Patch D, Matloff DS, Makuch R, Rendon G; Portal Hypertension Collaborative Group. Incidence, prevalence, and clinical significance of abnormal hematologic indices in compensated cirrhosis. Clin Gastroenterol Hepatol. 2009;7:689-695. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 209] [Cited by in RCA: 195] [Article Influence: 12.2] [Reference Citation Analysis (1)] |
| 19. | Daly ME. Determinants of platelet count in humans. Haematologica. 2011;96:10-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Cesar JM, Vecino AM. Survival and function of transfused platelets. Studies in two patients with congenital deficiencies of platelet membrane glycoproteins. Platelets. 2009;20:158-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Intagliata NM, Argo CK, Stine JG, Lisman T, Caldwell SH, Violi F; faculty of the 7th International Coagulation in Liver Disease. Concepts and Controversies in Haemostasis and Thrombosis Associated with Liver Disease: Proceedings of the 7th International Coagulation in Liver Disease Conference. Thromb Haemost. 2018;118:1491-1506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 130] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 22. | Joist JH. AICF and DIC in liver cirrhosis: expressions of a hypercoagulable state. Am J Gastroenterol. 1999;94:2801-2803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | Giannini EG, Greco A, Marenco S, Andorno E, Valente U, Savarino V. Incidence of bleeding following invasive procedures in patients with thrombocytopenia and advanced liver disease. Clin Gastroenterol Hepatol. 2010;8:899-902; quiz e109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 131] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 24. | McCarthy CP, Steg G, Bhatt DL. The management of antiplatelet therapy in acute coronary syndrome patients with thrombocytopenia: a clinical conundrum. Eur Heart J. 2017;38:3488-3492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (61)] |
| 25. | Scharf RE. Thrombocytopenia and Hemostatic Changes in Acute and Chronic Liver Disease: Pathophysiology, Clinical and Laboratory Features, and Management. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 26. | Garcia-Tsao G. Current Management of the Complications of Cirrhosis and Portal Hypertension: Variceal Hemorrhage, Ascites, and Spontaneous Bacterial Peritonitis. Dig Dis. 2016;34:382-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 27. | Ripoll C, Groszmann R, Garcia-Tsao G, Grace N, Burroughs A, Planas R, Escorsell A, Garcia-Pagan JC, Makuch R, Patch D, Matloff DS, Bosch J; Portal Hypertension Collaborative Group. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology. 2007;133:481-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 747] [Cited by in RCA: 810] [Article Influence: 45.0] [Reference Citation Analysis (1)] |
| 28. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1777] [Cited by in RCA: 1812] [Article Influence: 258.9] [Reference Citation Analysis (2)] |
| 29. | Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, Cuisset T, Cutlip D, Eerdmans P, Eikelboom J, Farb A, Gibson CM, Gregson J, Haude M, James SK, Kim HS, Kimura T, Konishi A, Laschinger J, Leon MB, Magee PFA, Mitsutake Y, Mylotte D, Pocock S, Price MJ, Rao SV, Spitzer E, Stockbridge N, Valgimigli M, Varenne O, Windhoevel U, Yeh RW, Krucoff MW, Morice MC. Defining High Bleeding Risk in Patients Undergoing Percutaneous Coronary Intervention. Circulation. 2019;140:240-261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 443] [Cited by in RCA: 529] [Article Influence: 88.2] [Reference Citation Analysis (0)] |
| 30. | Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D'Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3462] [Cited by in RCA: 3676] [Article Influence: 153.2] [Reference Citation Analysis (0)] |
| 31. | Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1-85. [PubMed] |
| 32. | Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5490] [Cited by in RCA: 5733] [Article Influence: 110.3] [Reference Citation Analysis (2)] |
| 33. | Urban P, Meredith IT, Abizaid A, Pocock SJ, Carrié D, Naber C, Lipiecki J, Richardt G, Iñiguez A, Brunel P, Valdes-Chavarri M, Garot P, Talwar S, Berland J, Abdellaoui M, Eberli F, Oldroyd K, Zambahari R, Gregson J, Greene S, Stoll HP, Morice MC; LEADERS FREE Investigators. Polymer-free Drug-Coated Coronary Stents in Patients at High Bleeding Risk. N Engl J Med. 2015;373:2038-2047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 590] [Cited by in RCA: 638] [Article Influence: 63.8] [Reference Citation Analysis (0)] |
| 34. | Windecker S, Latib A, Kedhi E, Kirtane AJ, Kandzari DE, Mehran R, Price MJ, Abizaid A, Simon DI, Worthley SG, Zaman A, Hudec M, Poliacikova P, Abdul Ghapar AKB, Selvaraj K, Petrov I, Mylotte D, Pinar E, Moreno R, Fabbiocchi F, Pasupati S, Kim HS, Aminian A, Tie C, Wlodarczak A, Hur SH, Marx SO, Jankovic I, Brar S, Bousquette L, Liu M, Stone GW; ONYX ONE Investigators. Polymer-based or Polymer-free Stents in Patients at High Bleeding Risk. N Engl J Med. 2020;382:1208-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 225] [Article Influence: 45.0] [Reference Citation Analysis (0)] |
| 35. | Wu VC, Chen SW, Chou AH, Ting PC, Chang CH, Wu M, Hsieh MJ, Wang CY, Chang SH, Lin MS, Hung KC, Hsieh IC, Chu PH, Wu CS, Lin YS. Dual antiplatelet therapy in patients with cirrhosis and acute myocardial infarction - A 13-year nationwide cohort study. PLoS One. 2019;14:e0223380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 36. | Krill T, Brown G, Weideman RA, Cipher DJ, Spechler SJ, Brilakis E, Feagins LA. Patients with cirrhosis who have coronary artery disease treated with cardiac stents have high rates of gastrointestinal bleeding, but no increased mortality. Aliment Pharmacol Ther. 2017;46:183-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 37. | Lu DY, Saybolt MD, Kiss DH, Matthai WH, Forde KA, Giri J, Wilensky RL. One-Year Outcomes of Percutaneous Coronary Intervention in Patients with End-Stage Liver Disease. Clin Med Insights Cardiol. 2020;14:1179546820901491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 38. | Azarbal B, Poommipanit P, Arbit B, Hage A, Patel J, Kittleson M, Kar S, Kaldas FM, Busuttil RW. Feasibility and safety of percutaneous coronary intervention in patients with end-stage liver disease referred for liver transplantation. Liver Transpl. 2011;17:809-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Marui A, Kimura T, Tanaka S, Miwa S, Yamazaki K, Minakata K, Nakata T, Ikeda T, Furukawa Y, Kita T, Sakata R; CREDO-Kyoto Investigators. Coronary revascularization in patients with liver cirrhosis. Ann Thorac Surg. 2011;91:1393-1399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 40. | Diedrich DA, Findlay JY, Harrison BA, Rosen CB. Influence of coronary artery disease on outcomes after liver transplantation. Transplant Proc. 2008;40:3554-3557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 41. | Plotkin JS, Scott VL, Pinna A, Dobsch BP, De Wolf AM, Kang Y. Morbidity and mortality in patients with coronary artery disease undergoing orthotopic liver transplantation. Liver Transpl Surg. 1996;2:426-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 197] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 42. | Yong CM, Sharma M, Ochoa V, Abnousi F, Roberts J, Bass NM, Niemann CU, Shiboski S, Prasad M, Tavakol M, Ports TA, Gregoratos G, Yeghiazarians Y, Boyle AJ. Multivessel coronary artery disease predicts mortality, length of stay, and pressor requirements after liver transplantation. Liver Transpl. 2010;16:1242-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 43. | Satapathy SK, Vanatta JM, Helmick RA, Flowers A, Kedia SK, Jiang Y, Ali B, Eason J, Nair SP, Ibebuogu UN. Outcome of Liver Transplant Recipients With Revascularized Coronary Artery Disease: A Comparative Analysis With and Without Cardiovascular Risk Factors. Transplantation. 2017;101:793-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 44. | Wray C, Scovotti JC, Tobis J, Niemann CU, Planinsic R, Walia A, Findlay J, Wagener G, Cywinski JB, Markovic D, Hughes C, Humar A, Olmos A, Sierra R, Busuttil R, Steadman RH. Liver transplantation outcome in patients with angiographically proven coronary artery disease: a multi-institutional study. Am J Transplant. 2013;13:184-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 45. | Wolfrum M, Fahrni G, de Maria GL, Knapp G, Curzen N, Kharbanda RK, Fröhlich GM, Banning AP. Impact of impaired fractional flow reserve after coronary interventions on outcomes: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2016;16:177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 46. | Park SJ, Ahn JM. Should we be using fractional flow reserve more routinely to select stable coronary patients for percutaneous coronary intervention? Curr Opin Cardiol. 2012;27:675-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Götberg M, Christiansen EH, Gudmundsdottir IJ, Sandhall L, Danielewicz M, Jakobsen L, Olsson SE, Öhagen P, Olsson H, Omerovic E, Calais F, Lindroos P, Maeng M, Tödt T, Venetsanos D, James SK, Kåregren A, Nilsson M, Carlsson J, Hauer D, Jensen J, Karlsson AC, Panayi G, Erlinge D, Fröbert O; iFR-SWEDEHEART Investigators. Instantaneous Wave-free Ratio vs Fractional Flow Reserve to Guide PCI. N Engl J Med. 2017;376:1813-1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 581] [Cited by in RCA: 703] [Article Influence: 87.9] [Reference Citation Analysis (1)] |
| 48. | Ariotti S, Adamo M, Costa F, Patialiakas A, Briguori C, Thury A, Colangelo S, Campo G, Tebaldi M, Ungi I, Tondi S, Roffi M, Menozzi A, de Cesare N, Garbo R, Meliga E, Testa L, Gabriel HM, Ferlini M, Vranckx P, Valgimigli M; ZEUS Investigators. Is Bare-Metal Stent Implantation Still Justifiable in High Bleeding Risk Patients Undergoing Percutaneous Coronary Intervention? JACC Cardiovasc Interv. 2016;9:426-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 131] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 49. | Latib A, Colombo A, Castriota F, Micari A, Cremonesi A, De Felice F, Marchese A, Tespili M, Presbitero P, Sgueglia GA, Buffoli F, Tamburino C, Varbella F, Menozzi A. A randomized multicenter study comparing a paclitaxel drug-eluting balloon with a paclitaxel-eluting stent in small coronary vessels: the BELLO (Balloon Elution and Late Loss Optimization) study. J Am Coll Cardiol. 2012;60:2473-2480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 276] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 50. | Jeger RV, Farah A, Ohlow MA, Mangner N, Möbius-Winkler S, Leibundgut G, Weilenmann D, Wöhrle J, Richter S, Schreiber M, Mahfoud F, Linke A, Stephan FP, Mueller C, Rickenbacher P, Coslovsky M, Gilgen N, Osswald S, Kaiser C, Scheller B; BASKET-SMALL 2 Investigators. Drug-coated balloons for small coronary artery disease (BASKET-SMALL 2): an open-label randomised non-inferiority trial. Lancet. 2018;392:849-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 306] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 51. | Liu W, Zhang M, Chen G, Li Z, Wei F. Drug-Coated Balloon for De Novo Coronary Artery Lesions: A Systematic Review and Trial Sequential Meta-analysis of Randomized Controlled Trials. Cardiovasc Ther. 2020;2020:4158363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 52. | Merinopoulos I, Gunawardena T, Wickramarachchi U, Richardson P, Maart C, Sreekumar S, Sawh C, Wistow T, Sarev T, Ryding A, Gilbert T, Perperoglou A, Vassiliou VS, Eccleshall SC. Long-term safety of paclitaxel drug-coated balloon-only angioplasty for de novo coronary artery disease: the SPARTAN DCB study. Clin Res Cardiol. 2021;110:220-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 53. | Lee MS, Wolfe M, Stone GW. Transradial vs transfemoral percutaneous coronary intervention in acute coronary syndromes: re-evaluation of the current body of evidence. JACC Cardiovasc Interv. 2013;6:1149-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 54. | Valgimigli M, Frigoli E, Leonardi S, Vranckx P, Rothenbühler M, Tebaldi M, Varbella F, Calabrò P, Garducci S, Rubartelli P, Briguori C, Andó G, Ferrario M, Limbruno U, Garbo R, Sganzerla P, Russo F, Nazzaro M, Lupi A, Cortese B, Ausiello A, Ierna S, Esposito G, Ferrante G, Santarelli A, Sardella G, de Cesare N, Tosi P, van 't Hof A, Omerovic E, Brugaletta S, Windecker S, Heg D, Jüni P; MATRIX Investigators. Radial vs femoral access and bivalirudin vs unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): final 1-year results of a multicentre, randomised controlled trial. Lancet. 2018;392:835-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 216] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 55. | Jacobs E, Singh V, Damluji A, Shah NR, Warsch JL, Ghanta R, Martin P, Alfonso CE, Martinez CA, Moscucci M, Cohen MG. Safety of transradial cardiac catheterization in patients with end-stage liver disease. Catheter Cardiovasc Interv. 2014;83:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 56. | Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, Jüni P, Kastrati A, Kolh P, Mauri L, Montalescot G, Neumann FJ, Petricevic M, Roffi M, Steg PG, Windecker S, Zamorano JL, Levine GN; ESC Scientific Document Group; ESC Committee for Practice Guidelines (CPG); ESC National Cardiac Societies. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2018;39:213-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1582] [Cited by in RCA: 1697] [Article Influence: 212.1] [Reference Citation Analysis (0)] |
| 57. | Bhatt DL, Hulot JS, Moliterno DJ, Harrington RA. Antiplatelet and anticoagulation therapy for acute coronary syndromes. Circ Res. 2014;114:1929-1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 58. | Bavishi C, Panwar S, Messerli FH, Bangalore S. Meta-Analysis of Comparison of the Newer Oral P2Y12 Inhibitors (Prasugrel or Ticagrelor) to Clopidogrel in Patients With Non-ST-Elevation Acute Coronary Syndrome. Am J Cardiol. 2015;116:809-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 59. | Jiang XL, Samant S, Lesko LJ, Schmidt S. Clinical pharmacokinetics and pharmacodynamics of clopidogrel. Clin Pharmacokinet. 2015;54:147-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 139] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 60. | Trankle CR, Vo C, Martin E, Puckett L, Siddiqui MS, Brophy DF, Stravitz T, Guzman LA. Clopidogrel Responsiveness in Patients With Decompensated Cirrhosis of the Liver Undergoing Pre-Transplant PCI. JACC Cardiovasc Interv. 2020;13:661-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 61. | Wei H, Child LJ. Clinical utility of viscoelastic testing in chronic liver disease: A systematic review. World J Hepatol. 2020;12:1115-1127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (2)] |
| 62. | Rout G, Shalimar, Gunjan D, Mahapatra SJ, Kedia S, Garg PK, Nayak B. Thromboelastography-guided blood product transfusion in cirrhosis patients with variceal bleeding: a randomized controlled trial. J Clin Gastroenterol. 2020;54:255-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 88] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 63. | De Pietri L, Bianchini M, Montalti R, De Maria N, Di Maira T, Begliomini B, Gerunda GE, di Benedetto F, Garcia-Tsao G, Villa E. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: A randomized, controlled trial. Hepatology. 2016;63:566-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 310] [Article Influence: 34.4] [Reference Citation Analysis (0)] |
| 64. | Khan SU, Lone AN, Asad ZUA, Rahman H, Khan MS, Saleem MA, Arshad A, Nawaz N, Sattur S, Kaluski E. Meta-Analysis of Efficacy and Safety of Proton Pump Inhibitors with Dual Antiplatelet Therapy for Coronary Artery Disease. Cardiovasc Revasc Med. 2019;20:1125-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 65. | Verma S, Peterson EL, Liu B, Sabbah HN, Williams LK, Lanfear DE. Effectiveness of beta blockers in patients with and without a history of myocardial infarction. Eur J Clin Pharmacol. 2020;76:1161-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |