Published online Jun 26, 2020. doi: 10.4330/wjc.v12.i6.262
Peer-review started: January 30, 2020
First decision: April 3, 2020
Revised: May 12, 2020
Accepted: May 14, 2020
Article in press: May 14, 2020
Published online: June 26, 2020
Processing time: 148 Days and 5.6 Hours
Echocardiograms are an incredibly useful diagnostic tool due to their lack of harmful radiation, the relative ease and speed with which they can be performed, and their almost ubiquitous availability. Unfortunately, the advantages that support the use of echocardiography can also lead to the overuse of this technology. We sought to evaluate the physician perceived impact echocardiography has on patient management.
To evaluate the physician perceived impact echocardiography has on patient management.
Surveys were distributed to the ordering physician for echocardiograms performed at our institution over a 10-wk period. Only transthoracic echocardiograms performed on the inpatient service were included. Surveys were distributed to either the attending physician or the resident physician listed on the echocardiogram order. The information requested in the survey focused on the indication for the study and the perceived importance and effect of the study. Observational statistical analysis was performed on all of the answers from the collected surveys.
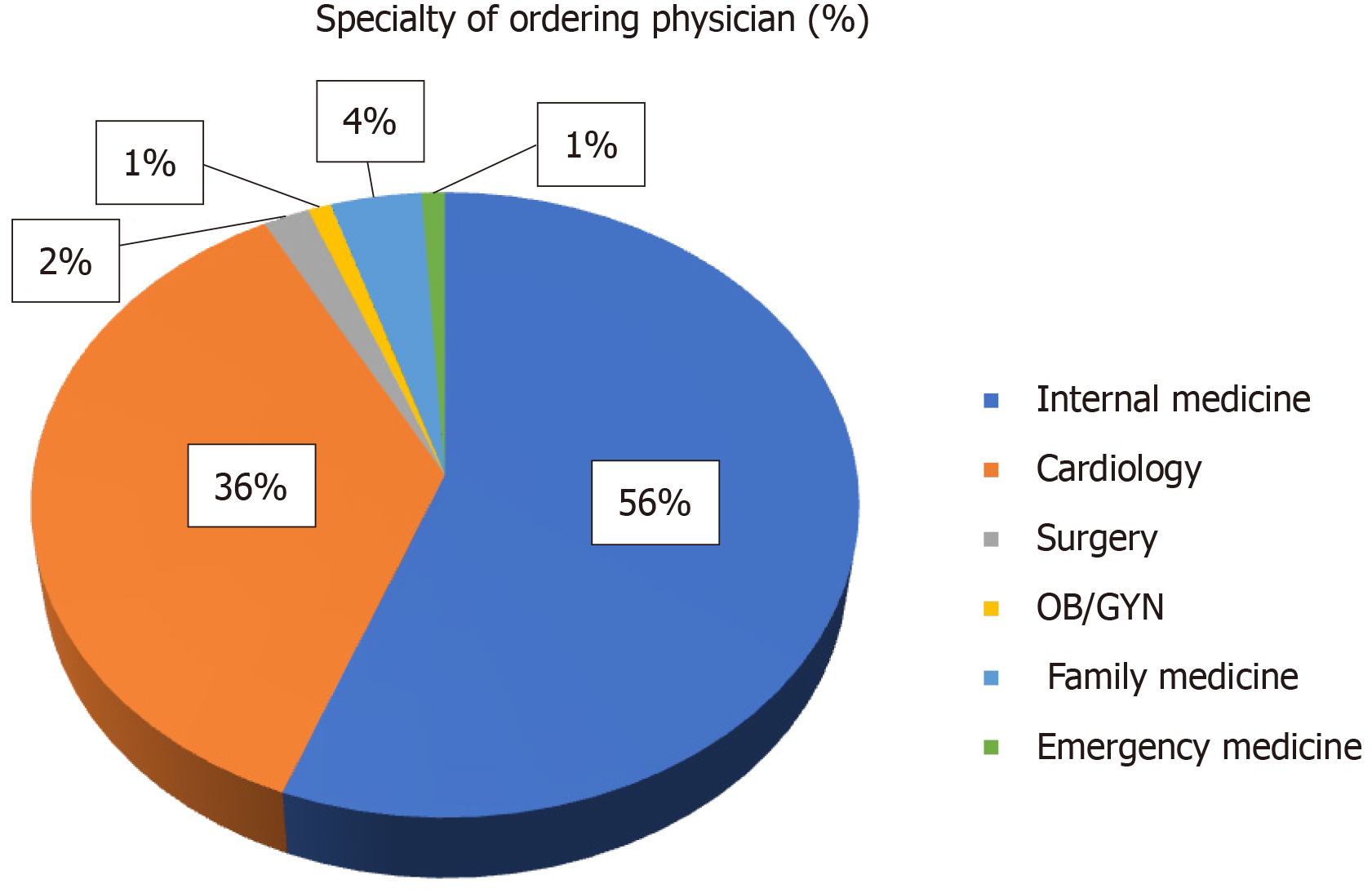
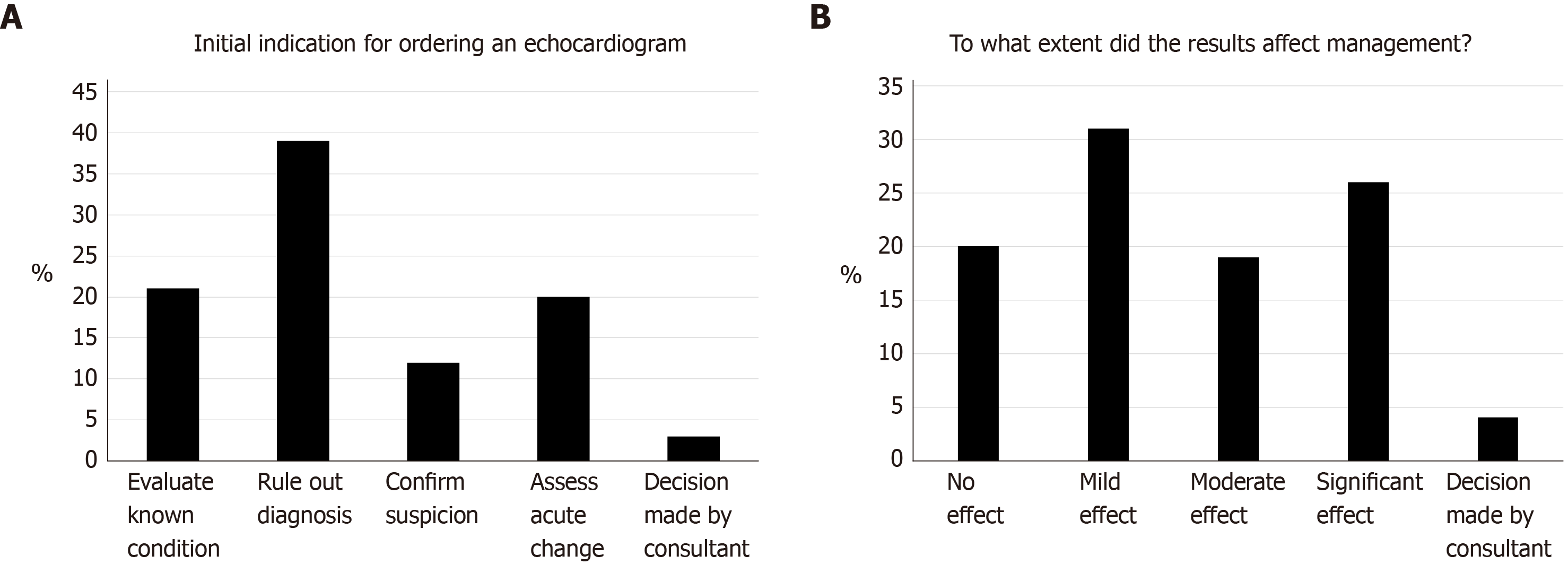
A total of 103 surveys were obtained and analyzed. The internal medicine (57%) and cardiology (37%) specialties ordered the most echocardiograms. The most common reason for ordering an echocardiogram was to rule out a diagnosis (38.2%). Only 27.5% of physicians reported that the echocardiogram significantly affected patient care, with 18.6% reporting a moderate effect, and 30.4% reporting a mild effect. A total of 19.6% of physicians stated that there was no effect on patient management. Additionally, 43.1% of physicians reported that they made changes in patient management due to no change having occurred in the disease, 11.8% reported that changes in management were based on the recommendation of a specialist, and only 9.8% reported that further imaging was ordered due to the results of the echocardiogram. The majority of physicians (67.6%) considered an echocardiogram to be “somewhat essential” in the management of adult inpatients, with only 15.7% considering it “essential”.
The majority of physicians surveyed report the echocardiogram had only a mild effect on management with only 27.5% reporting a significant effect. However, the majority of physicians (83.3%) perceived an echocardiogram to be somewhat or entirely essential for management. Only 9.8% reported the echo led to further imaging. These insights into ordering physician reasoning should help guide better definition of the optimal and ideal use of echocardiography.
Core tip: The echocardiogram is a useful tool used by cardiologists to manage patients. However, its practicality and availability may result in the overuse of echocardiography in situations where it is not warranted. Such overuse may result in exhaustion of resources and reduced efficiency. Our survey of physicians who ordered an echocardiogram sheds light on the true and perceived usefulness of the echocardiogram in an inpatient setting. The results illustrate physicians’ perception of echocardiography as somewhat or entirely essential for patient management, despite a proportion of reported mild or no effect on patient management.
- Citation: Khalili A, Drummond J, Ramjattan N, Zeltser R, Makaryus AN. Diagnostic and treatment utility of echocardiography in the management of the cardiac patient. World J Cardiol 2020; 12(6): 262-268
- URL: https://www.wjgnet.com/1949-8462/full/v12/i6/262.htm
- DOI: https://dx.doi.org/10.4330/wjc.v12.i6.262
A transthoracic echocardiogram (TTE) is a commonly utilized imaging modality in the inpatient setting. TTE is a useful and convenient tool to evaluate patients who have or are at risk of having cardiovascular disease. The lack of harmful radiation, the relative ease and speed with which they can be performed, and their almost ubiquitous availability make TTE central to the diagnostic armamentarium in cardiac patients. Unfortunately, the advantages that support the use of echocardiography can also lead to its overuse. Appropriate use guidelines have been developed by medical organizations to counteract this overuse, however, despite this, several studies have shown evidence that echocardiograms continue to be over-utilized[1,2].
A nationwide study of hospitals in the United States found that the use of inpatient echocardiography has been continually increasing at an average rate of 3% annually for over a decade. It was also noted that the use of TTE has approximately doubled between 1999 and 2008[1,2]. The trend has continued with TTE use increasing between 5% and 8% annually and this has led to the creation of the appropriate use criteria (AUC) for echocardiography in 2007, and their update in 2011 with subsequent criteria for echocardiography now included under the umbrella of the Multimodality Cardiac Imaging AUC[3,4]. The rapid increase of TTE utilization brings the question of whether TTE is being overused or possibly being applied in inappropriate situations. Multiple published reports have suggested that echocardiograms may be performed with decreased clinical utility and may not have a clinical effect on the management of a patient[5-8]. We sought to evaluate the TTE-ordering physician’s perceived impact echocardiography has on patient management.
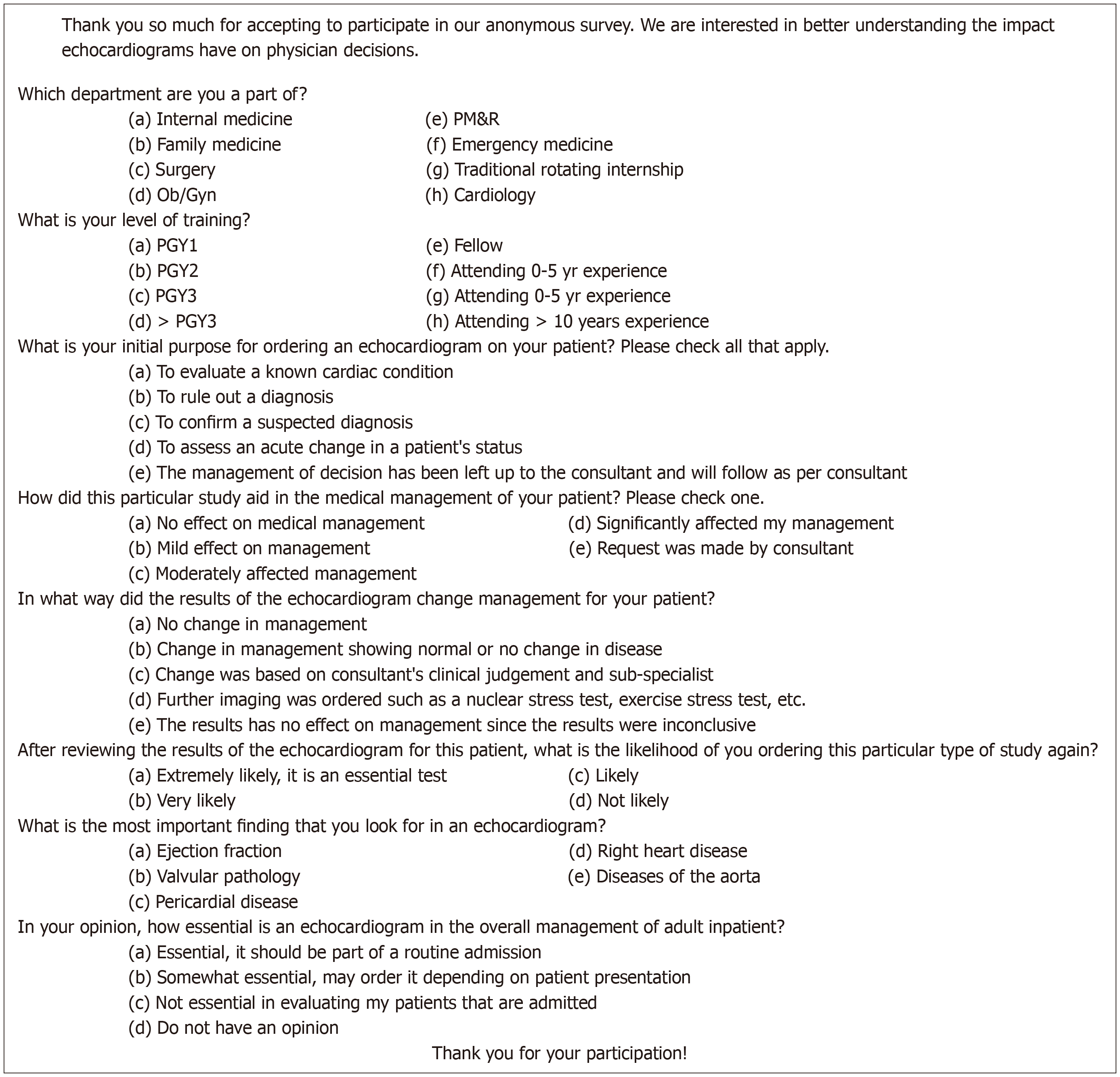
Data was collected by distributing surveys to physicians who ordered TTEs at our institution during a 10-wk period. Surveys were distributed to the ordering physician at our facility over a 2-month period. Surveys were distributed to either the attending physician or the resident physician listed on the echocardiogram order. Only echocardiograms ordered in an inpatient setting were included. Surveys were not distributed to the physician if the echocardiogram had been ordered more than ten days previously to assure recall of the patient circumstances by the ordering physician. The physician's perception of the utility of TTE in standard clinical practice was assessed by surveying physicians at all levels of training who ordered a TTE for their hospitalized patients. The information requested in the survey is summarized here and the full survey is shown in Figure 1: (1) Why the echocardiogram had been ordered; (2) Who had ordered the imaging study and their level of training; (3) The extent to which it affected the patient’s treatment; (4) The type of effect it had on the patient’s treatment (e.g., treatment was altered or remained the same due to the results of the echocardiogram); (5) How likely the ordering physician was to order an echocardiogram in the future; and (6) What the ordering physician considered the most important possible finding in an echocardiogram. Observational statistical analysis was performed on all of the answers from the collected surveys.
A total of 103 surveys were obtained and analyzed. Surveys were distributed to multiple hospital departments. The majority of the echocardiograms (57%) were ordered by the internal medicine physicians, followed by cardiologists (37%) (Figure 2). The most common reason for a physician ordering an echocardiogram was to rule out a diagnosis (38.2%) and to evaluate a known cardiac condition (22%) (Figure 3A). However, 19.6% of physicians stated that there was actually no effect on patient management (Figure 3B). Additionally, 30.4% of physicians reported a mild effect, 18.6% declared a moderate effect, and only 27.5% of physicians reported that the echocardiogram significantly affected patient care. Almost half (43.1%) of physicians reported that they altered their patient management due to no change having occurred in the disease based on echo findings, 11.8% reported that changes in management were based on the recommendation of a specialist, and only 9.8% reported that further imaging was ordered due to the results of the echocardiogram. The study also reveals that the majority of physicians (67.6%) considered an echocardiogram to be “somewhat essential” in the management of adult inpatients, with only 15.7% considering it “essential”, and 14.7% chose not to answer this question.
In response to the dilemma of echocardiography overuse, the AUC for echocardiography was developed in collaboration with The American College of Cardiology Foundation and the American Society of Echocardiography. The initial AUC for echocardiography[1,2] rated indications as: “appropriate”, “inappropriate”, or “uncertain”. The more recent statements include echocardiography evaluated under the multimodality imaging criteria[3,4] and rank indications as “appropriate”, “may be appropriate”, and “rarely appropriate”. Generally, inappropriate use for the echocardiogram is rated in clinical cases where routine testing provided no change in clinical status or did not change management. Appropriate use was identified in clinical scenarios when the echocardiography result provided a change in clinical management or when used for initial diagnosis when there is a change in clinical status[9].
Studies evaluating the correlation between TTE use, AUC, and its clinical impact have shown various findings. In a retrospective study conducted in an academic medical center, 535 consecutive TTEs were reviewed. The study reported that although 9 in 10 TTEs were appropriate by AUC, less than 1 in 3 TTEs actually resulted in an active change in patient care, with nearly half resulting in the continuation of the current clinical care plan[10]. Other studies[5-8] have shown similar results and this leads to the revelation that while AUC may be useful to guide the choice to pursue a TTE, physician perception of the possibility of the presence of indications supported by the AUC may not necessarily correlate to the change in management expected and therefore still lead to overutilization of TTE due to the various reasons that make TTE so easy to order.
This realization is supported by our study showing that the majority of physicians surveyed stated that the echocardiogram only had a mild effect on management. However, the majority of physicians perceived an echocardiogram to be somewhat or entirely essential to the management of adult inpatients. Echocardiography is a useful test which easily provides a plethora of useful data about the cardiac patient in the inpatient setting as assessed by the ordering physicians. Perhaps instead of trying to limit TTE use, more efforts should allow for the implementation of bedside point of care echocardiography which can be more easily learned and implemented and be performed in a more time and cost-efficient manner.
While the majority of physicians perceived that the TTE resulted in a change in patient management in some way, 19.6% of survey results reported no effect on patient management. This finding highlights the importance of increased optimization of proper echocardiography use. Improvement of the appropriate use of clinical resources will offer increased high-quality healthcare and better utilization of hospital resources for patients who appropriately need the test.
Similar findings have been supported by other studies. In the study by Matulevicius et al[10], out of their 535 consecutive TTEs, 31.8% resulted in an active change in care; 46.9% a continuation of current care; and 21.3% no change in care. By 2011 AUC, 91.8% of TTEs were appropriate; 4.3% inappropriate; and 3.9% uncertain. Although 9 in 10 TTEs were appropriate by 2011 AUC, fewer than 1 in 3 TTEs resulted in an active change in care, nearly half resulted in a continuation of current care, and slightly more than 1 in 5 resulted in no change in care. The low rate of active change in care (31.8%) among TTEs mostly classified as appropriate (91.8%) highlights the need for a better method to optimize TTE utilization to use limited healthcare resources efficiently while providing high-quality care[10].
The present study is limited by the relatively small number of patients and its population of a single hospital rather than a multi-facility population with a larger sample size. There are also the given limitations of the survey study type which may include factors such as dishonesty, skipped questions, difficult questions and lack of conscientious answers.
While the AUC may reduce inappropriate studies, it still may result in unnecessary studies since 19.6% of cases did not change management. With the increased aging of our population and the rising cost of healthcare, improper utilization of resources must be identified and addressed. Systems of review, assessment, and action to change based on review, can limit inappropriate and unnecessary TTE performance. The employment of structured referral systems for TTE and an easily accessible and comprehensive checklist of appropriate indications as well as the focus by medical societies and the bodies responsible for regulating training programs for physicians of different medical specialties, will likely improve appropriate use of echocardiograms. While this improvement will expectedly improve efficiency and allow for correct employment of the use of echocardiography, our study shows that the actual versus the perceived usefulness of the echocardiogram in an inpatient setting usually does not correlate. Our results highlight the discrepancy of physicians’ perception of echocardiography as somewhat or entirely essential for patient management, despite a proportion of reported mild or no effect on patient management. Because of this mismatch, it may therefore be better to allow for the implementation of bedside point of care echocardiography which can more easily be learned and implemented and be performed in a better time and cost-efficient manner while still providing essential patient information.
The transthoracic echocardiogram (TTE) is a cardiovascular imaging tool that is used by doctors and hospitals to evaluate patients in various settings. The TTE is an incredibly useful tool due to the ability to examine the heart non-invasively, as well as the efficiency and lack of risk. Due to its usefulness and ease, it has been known to be overused. This has been recognized by the appropriate use criteria (AUC) and therefore guidelines have been created to limit its overuse. However, it has been perceived that the echocardiogram is still being overused in many settings despite the guidelines.
The topic of this study is to evaluate the perceived impact the TTE has on inpatient management. The overuse of this tool is an example of inappropriate usage of healthcare resources and can lead to improper patient care. Improving utilization of this tool will optimize patient care.
The objective of this study is to better understand the perceived impact that the TTE has on patient management that leads to its continued overuse.
This observational study was conducted by distribution of surveys to physicians at an academic institution. The survey was completed by physicians of multiple hospital departments, who ordered a TTE within a 10 wk period in the inpatient setting. The survey requested information on the perceived importance and impact the TTE had on clinical management.
The most common reason for a physician ordering a TTE was to rule out a diagnosis and to evaluate a known cardiac condition. A total of 19.6% of physicians stated that there was no effect on patient management, 30.4% of physicians reported a mild effect, 18.6% declared a moderate effect, and only 27.5% of physicians reported that the echocardiogram significantly affected patient care. Almost half of physicians reported that they altered their patient management due to no change having occurred in the disease based on TTE findings, 11.8% reported that changes in management were based on the recommendation of a specialist, and only 9.8% reported that further imaging was ordered due to the results of the echocardiogram. The majority of physicians considered an echocardiogram to be “somewhat essential” in the management of adult inpatients, with only 15.7% considering it “essential”, and 14.7% chose not to answer this question.
This study reveals that there are a substantial number of physicians who order TTE without proper use despite the AUC guidelines. Many physicians stated in our study that the TTE had only a mild or no effect on patient management but is still perceived to be somewhat or entirely essential to patient care. While the AUC guidelines expectedly did limit an amount of inappropriate use of the TTE, this study better illustrates the actual utility of the TTE after the criteria is implemented. This lack of correlation calls for a new process of TTE utilization review of patient management for inpatient care.
This study revealed the importance of increased optimization of proper echocardiography use. Future research should explore bedside point of care echocardiography which can be performed more efficiently while still providing proper patient management.
Manuscript source: Invited manuscript
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bamoshmoosh M, Gulel O, Spiliopoulos S S-Editor: Dou Y L-Editor: A E-Editor: Qi LL
| 1. | Douglas PS, Khandheria B, Stainback RF, Weissman NJ, Brindis RG, Patel MR, Khandheria B, Alpert JS, Fitzgerald D, Heidenreich P, Martin ET, Messer JV, Miller AB, Picard MH, Raggi P, Reed KD, Rumsfeld JS, Steimle AE, Tonkovic R, Vijayaraghavan K, Weissman NJ, Yeon SB, Brindis RG, Douglas PS, Hendel RC, Patel MR, Peterson E, Wolk MJ, Allen JM; American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group; American Society of Echocardiography; American College of Emergency Physicians; American Society of Nuclear Cardiology; Society for Cardiovascular Angiography and Interventions; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; American College of Chest Physicians; Society of Critical Care Medicine. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Coll Cardiol. 2007;50:187-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 227] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 2. | American College of Cardiology Foundation Appropriate Use Criteria Task Force; American Society of Echocardiography; American Heart Association; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Critical Care Medicine; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; American College of Chest Physicians, Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR, Picard MH, Polk DM, Ragosta M, Parker Ward R, Weiner RB. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance American College of Chest Physicians. J Am Soc Echocardiogr. 2011;24:229-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 333] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 3. | Doherty JU, Kort S, Mehran R, Schoenhagen P, Soman P; Rating Panel Members; Appropriate Use Criteria Task Force. ACC/AATS/AHA/ASE/ASNC/HRS/SCAI/SCCT/SCMR/STS 2019 Appropriate Use Criteria for Multimodality Imaging in the Assessment of Cardiac Structure and Function in Nonvalvular Heart Disease : A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and the Society of Thoracic Surgeons. J Nucl Cardiol. 2019;26:1392-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Sachdeva R, Valente AM, Armstrong AK, Cook SC, Han BK, Lopez L, Lui GK, Pickard SS, Powell AJ, Bhave NM, Sachdeva R, Valente AM, Pickard SS, Baffa JM, Banka P, Cohen SB, Glickstein JS, Kanter JP, Kanter RJ, Kim YY, Kipps AK, Latson LA, Lin JP, Parra DA, Rodriguez FH, Saarel EV, Srivastava S, Stephenson EA, Stout KK, Zaidi AN. ACC/AHA/ASE/HRS/ISACHD/SCAI/SCCT/SCMR/SOPE 2020 Appropriate Use Criteria for Multimodality Imaging During the Follow-Up Care of Patients With Congenital Heart Disease: A Report of the American College of Cardiology Solution Set Oversight Committee and Appropriate Use Criteria Task Force, American Heart Association, American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Pediatric Echocardiography. J Am Coll Cardiol. 2020;75:657-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 5. | Tharmaratnam T, Bouck Z, Sivaswamy A, Wijeysundera HC, Chu C, Yin CX, Nesbitt GC, Edwards J, Yared K, Wong B, Weinerman A, Thavendiranathan P, Rakowski H, Dorian P, Anderson G, Austin PC, Dudzinski DM, Ko DT, Weiner RB, Bhatia RS. Low-Value Transthoracic Echocardiography, Healthcare Utilization, and Clinical Outcomes in Patients With Coronary Artery Disease. Circ Cardiovasc Qual Outcomes. 2019;12:e006123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Law TK, Bouck Z, Yin XC, Dudzinski D, Myers D, Nesbitt GC, Edwards J, Yared K, Wong B, Hansen M, Weinerman A, Shadowitz S, Farkouh M, Thavendiranathan P, Udell J, Johri A, Chow CM, Rakowski H, Picard MH, Weiner RB, Bhatia RS. Association Between Transthoracic Echocardiography Appropriateness and Echocardiographic Findings. J Am Soc Echocardiogr. 2019;32:667-673.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Gomes S, Freitas E, Pereira D. Appropriate use criteria for transthoracic echocardiography. Rev Port Cardiol. 2019;38:229-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Salik JR, Sen S, Picard MH, Weiner RB, Dudzinski DM. The application of appropriate use criteria for transthoracic echocardiography in a cardiac intensive care unit. Echocardiography. 2019;36:631-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999-2008. Circ Cardiovasc Qual Outcomes. 2012;5:31-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 10. | Matulevicius SA, Rohatgi A, Das SR, Price AL, DeLuna A, Reimold SC. Appropriate use and clinical impact of transthoracic echocardiography. JAMA Intern Med. 2013;173:1600-1607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |