Peer-review started: May 10, 2019
First decision: August 16, 2019
Revised: August 27, 2019
Accepted: October 14, 2019
Article in press: October 15, 2019
Published online: January 26, 2020
Processing time: 232 Days and 18.6 Hours
Coronary angiography and eventual revascularization have become the most common approaches for patients with acute coronary syndromes. Ischemia detection in this scenario is usually regarded as unnecessary for most of the patients. In fact, current guidelines recommend complete revascularization for patients with multivessel disease in the context of ST-elevation myocardial infarction, although it is in contrast with previous recommendations. However, some recent data suggested that ischemia could have a role for the decision of revascularization in these patients. The CROSS-AMI study randomized patients with ST-elevation myocardial infarction treated with primary angioplasty and who also had multivessel disease to a complete anatomic revascularization of the non-infarct related artery lesions vs subsequent revascularization of the non-infarct related artery lesions only if ischemia was demonstrated by stress echocardiography. The main findings were that only 30% of the patients in the ischemia arm needed a second revascularization and that the outcome was similar in both arms. Regarding non-ST-elevation acute coronary syndrome, coronary angiography is in general warranted for most of the patients. However, recent long-term published studies on patients randomized to an invasive or less aggressive approach based on ischemia detection have found no differences in outcome. The ultimate study in non-ST-elevation acute coronary syndrome comparing ischemia detection with an invasive approach is pending. Therefore, ischemia detection might have a role for stratifying these subjects. This is particularly true in the current era of imaging of high quality and sensitivity, last generation stents, radial access and modern antithrombotic therapy.
Core tip: Coronary angiography and eventual revascularization have become the most common approaches for patients with acute coronary syndromes. Ischemia detection in this scenario is usually regarded as unnecessary for most of the patients. However, some recent data suggested that it could have a role in the decision-making process, particularly after ST-elevation acute myocardial infarction in the presence of multivessel disease but also after non-ST-elevation acute coronary syndrome.
- Citation: Peteiro J, Bouzas-Mosquera A. Is there a role for ischemia detection after an acute myocardial infarction? World J Cardiol 2020; 12(1): 1-6
- URL: https://www.wjgnet.com/1949-8462/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.4330/wjc.v12.i1.1
Coronary angiography and eventual revascularization have become the most common approaches for patients with acute coronary syndromes. Although ischemia detection is usually regarded as unnecessary for most of these patients, some recent data suggested that it could have a role in the decision-making process.
The best treatment for STEMI is to rapidly open the infarct-related artery (IRA), which is better achieved by angioplasty[1]. However, having done this, patients may still have significant coronary stenoses in up to 40% to 60% of the cases. These patients likely have higher atherosclerotic burden with increased risk, and it is not clear how to prevent their risk. Also, these patients may have worse left ventricular function.
In the last years several studies have dealt with the issue of multivessel disease (MVD) after STEMI treated with primary angioplasty, and these studies have been changing the guidelines ever since. Thus, guidelines in 2013 recommended exclusive treatment of the IRA[2] reserving treatment of MVD just in cases of cardiogenic shock or persistent ischemia (indication IIa-class B), whereas the last guidelines recommend routine revascularization of MVD before hospital discharge (indication IIa-class A)[3].
The PRAMI[4] and CvLPRIT[5] studies randomized patients with STEMI and MVD disease to an IRA-only strategy vs complete revascularization and reported better outcome with the complete revascularization strategy.
Further studies like the PRIMULTI[6] and the ACUTE-COMPARE[7] randomized STEMI and MVD disease patients to an IRA-only revascularization strategy vs a complete revascularization strategy based on ischemia, as detected by flow reserve-guided (FFR) < 0.80. Both studies demonstrated that the functional strategy was better than the mere revascularization of the IRA.
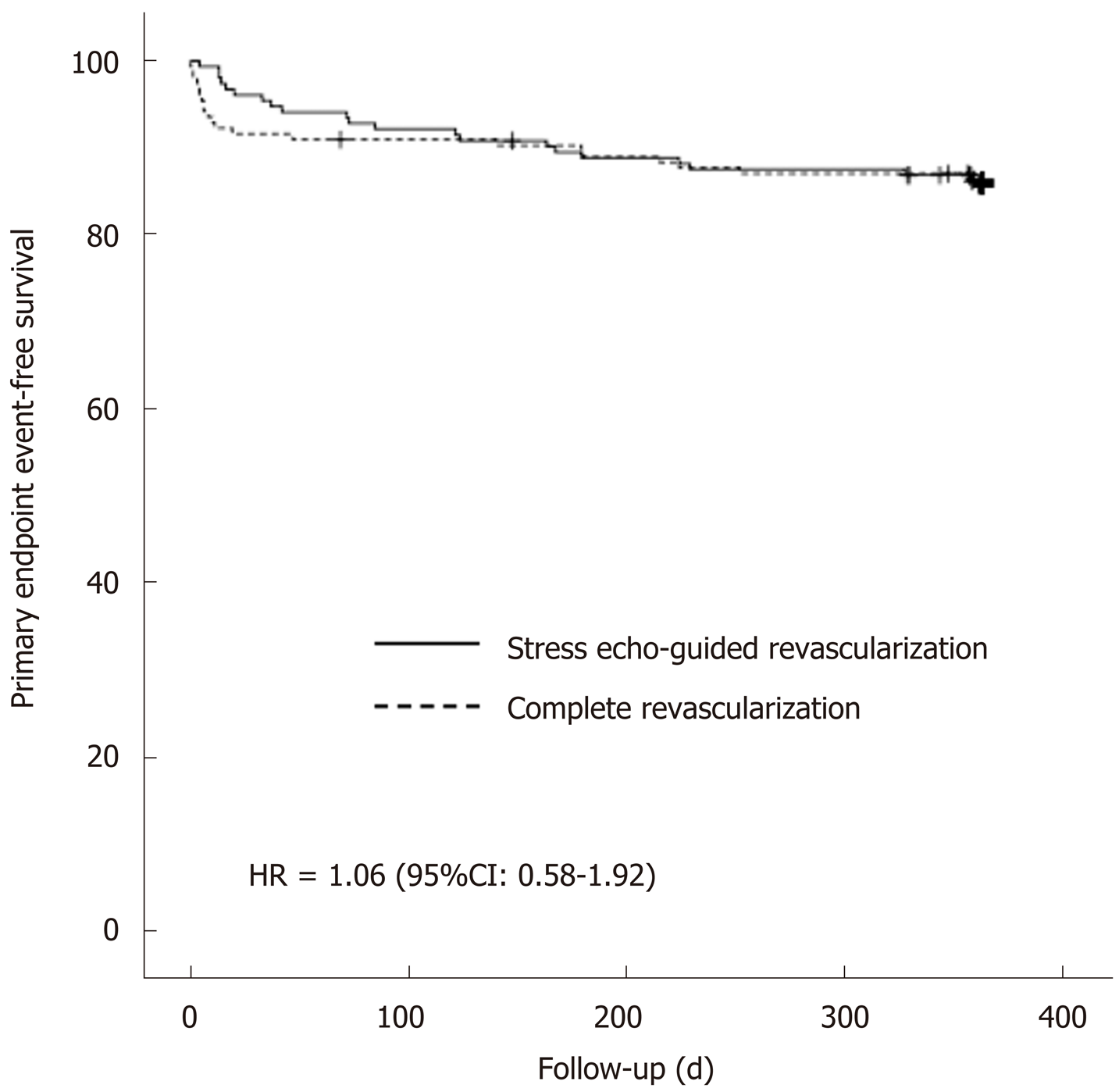
Recently, the CROSS-AMI study, using a completely different design, randomized patients with STEMI treated with primary angioplasty and who also had MVD to a complete anatomic revascularization of the non-infarct related artery (non-IRA) lesions vs subsequent revascularization of the non-IRA lesions only if ischemia was demonstrated by stress echocardiography[8,9]. The main findings of this study were that only 30% of the patients in the ischemia arm needed a second revascularization and that the outcome was similar in both arms. In fact, there were 22 events in the complete revascularization arm and 21 in the ischemia-guided arm [14.3% vs 13.8%; hazard ratio (HR) = 1.06, 95% confidence interval (CI): 0.58-1.92, P = not significant]. Figure 1 shows the Kaplan-Meier event-free survival curves for both arms and Video 1 to 3 are examples of two patients randomized to the stress-guided strategy. Of note, most of the stress echocardiography studies were performed using peak treadmill exercise, a very sensitive modality[10,11]. This study therefore showed that ischemia detection has indeed a role for avoiding procedures and saving costs in this scenario.
These results are not completely surprising because revascularization based on ischemia has led to better prognosis than revascularization based on anatomy as reported in the FAME study, where ischemia was investigated by FFR[12]. The investigators found that measurement of FFR in patients with multivessel coronary artery disease who were undergoing percutaneous coronary intervention with drug-eluting stents significantly reduced the rate of the composite end point of death, nonfatal myocardial infarction, and repeat revascularization. Also, Escaned et al[13] recently reported similar results, such that the use of functional assessment based on FFR/iFR led to a 25% reduction in the use of stents.
Additional studies on this subject are ongoing. For instance, the FULL-REVASC study will randomize patients with STEMI and MVD to an initial conservative management of non-IRA lesions vs FFR-guided revascularization of non-culprit lesions during hospitalization (https://www.ucr.uu.se/fullrevasc/).
However, as it is clear from above, the optimum study would be one with three arms comparing conservative management of non-IRA stenoses, complete anatomic revascularization and ischemia/FFR-guided revascularization. Meanwhile, it is worth stating that the current approach in our center for patients with STEMI and multivessel coronary artery disease is based on ischemia.
In patients with non-ST-elevation acute coronary syndrome who do not have recurrence of chest pain, signs of heart failure or abnormalities in the initial or subsequent electrocardiography and increase in (preferably high-sensitivity) cardiac troponin level, a non-invasive stress test (preferably with imaging) for inducible ischemia is recommended before deciding on an invasive strategy. This recommendation has been clearly stated in the last guidelines on the issue[14].
Therefore, when there is troponin elevation, a coronary angiography is currently warranted. However, in the last decades there has been a lot of discussion on this matter, and several studies have focused on the comparison between an invasive and functional strategy for patients with non-STEMI or unstable angina. A Cochrane review[15] joining all studies published between 2001 and 2012 and including almost 9000 patients found that there was no significant differences in mortality [risk ratio (RR) = 0.87; CI: 0.64-1.18] or in the composite of mortality and non-fatal myocardial infarction (RR = 0.93; CI: 0.71-1.2). Less hard end-points like myocardial infarction (RR = 0.79; CI: 0.63-1), refractory angina (RR = 0.64; CI: 0.52-0.79) and rehospitalization (RR = 0.77; CI: 0.63-0.94) were lower with the invasive strategy. In contrast, complications of angiography or revascularization like bleeding or procedure-related myocardial infarction were higher in the invasive arms (RR = 1.73, CI: 1.2-2.31; and RR = 1.87, CI: 1.47-2.37). Therefore, the conclusion of this meta-analysis was that in patients with non-ST-elevation acute coronary syndrome, a conservative strategy based on clinical risk for recurrent events is the preferred management strategy. However, it is worth stating that the use of stents was lower (50% to 88% of the patients), and the use of coronary artery by-pass was higher (up to 10% to 41% of revascularizations). Also, antiplatelet therapy was less developed. On the other hand, functional testing consisted of just exercise electrocardiography for most of the patients.
In this regard, the only old study that clearly observed a superiority of a functional approach in patients with non-STEMI was the VANQUISH trial[16]. Unlike other conceptually similar studies, the conservative strategy of the VANQUISH was in fact a “conservative aggressive strategy” as almost half of the patients in this arm underwent coronary angiography. Another key point was that almost all patients in the conservative arm were studied by treadmill exercise with myocardial perfusion imaging, which is a very sensitive technique, or by dypiridamole myocardial perfusion imaging in case of the inability to exercise. Although the VANQUISH trial was a pre-stent study, these aspects may explain the superiority of the conservative strategy over the invasive strategy regarding both the primary end-point (P = 0.007) and all-cause death (P = 0.004).
Some of these studies comparing invasive and conservative approaches have long term follow-up. Fox et al[17] published the joint results of the fast revascularization during instability in coronary artery disease (FRISC-II), randomized intervention trial of unstable angina 3 (RITA-3) and invasive vs conservative treatment in unstable coronary syndromes (ICTUS) at 5 years, demonstrating superiority of an invasive strategy for the combination of cardiovascular death and myocardial infarction (HR = 0.8, CI: 0.71-0.93, P = 0.002), which was driven for myocardial infarction occurrence (HR = 0.77; CI: 0.65-0.90, P = 0.001); the difference in cardiovascular mortality did not reach statistical significance (HR = 0.83, CI: 0.68-1.01, P = 0.068). However, these differences were at expense of the results of the FRISC-II and RITA-3 studies, as in the ICTUS study there were no significant differences between arms.
We were curious what the differences between the ICTUS study and the other studies were. Crucial differences were that the percentage of angiographies in the conservative arm of ICTUS reached up to 53% of the patients, and all patients in the conservative arm were studied by a sensitive imaging technique (both characteristics similar to the older VANQUISH study). Table 1 depicts these differences between studies. In fact, the ICTUS trial at 10 years demonstrated an excess of the combined event (death or myocardial infarction) in the invasive arm as compared to the conservative arm (HR = 1.30, CI: 1.07-1.58, P = 0.009)[18]. In addition, both the RITA-3 at 10 years and the FRISC-II at 15 years, which were studies that had shown better performance of an invasive strategy in the first years, found no significant differences in mortality between arms at longer-term follow-up[19,20]. Therefore, given these results, it is not surprising that some experts have advocated for a fair study comparing the two strategies in a current era of imaging of high quality and sensitivity, last generation stents, radial access and modern antithrombotic therapy[21].
| FRISC-II | RITA-3 | ICTUS | |
| Year | 1999 | 2002 | 2005 |
| Inclusion criteria: Raised troponin | No | No | Yes |
| Functional imaging in the conservative arm | - | No (exercise ECG testing) | Yes (exercise with MIBI-SPECT) |
| Interventionism in the conservative arm | 7% | 16% | 53% |
| Stents, invasive arm | 61% | 88% | 88% |
The use of exercise electrocardiography testing in most of the conservative arms of the above-mentioned studies (if performed) should be considered as an important limitation. The superiority of modern techniques of imaging like stress echocardiography[10,11], magnetic resonance or myocardial perfusion imaging would likely make a difference for stratification of these patients.
In patients with acute myocardial infarction and MVD, ischemia detection may be useful for clinical decisions. In non-ST elevation myocardial infarction or acute coronary syndrome, the ultimate role of ischemia detection for clinical decision making process in the current era of modern imaging and new drugs and stents is pending.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Micheu MM, Sato A, Sicari R, Ueda H S-Editor: Tang JZ L-Editor: Filipodia E-Editor: Zhang YL
| 1. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2722] [Cited by in RCA: 4498] [Article Influence: 899.6] [Reference Citation Analysis (0)] |
| 2. | Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC); Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van 't Hof A, Widimsky P, Zahger D. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3540] [Cited by in RCA: 3705] [Article Influence: 285.0] [Reference Citation Analysis (0)] |
| 3. | Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7073] [Cited by in RCA: 6650] [Article Influence: 950.0] [Reference Citation Analysis (0)] |
| 4. | Wald DS, Morris JK, Wald NJ, Chase AJ, Edwards RJ, Hughes LO, Berry C, Oldroyd KG; PRAMI Investigators. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013;369:1115-1123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 727] [Cited by in RCA: 810] [Article Influence: 67.5] [Reference Citation Analysis (0)] |
| 5. | Gershlick AH, Khan JN, Kelly DJ, Greenwood JP, Sasikaran T, Curzen N, Blackman DJ, Dalby M, Fairbrother KL, Banya W, Wang D, Flather M, Hetherington SL, Kelion AD, Talwar S, Gunning M, Hall R, Swanton H, McCann GP. Randomized trial of complete vs lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. 2015;65:963-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 652] [Article Influence: 72.4] [Reference Citation Analysis (0)] |
| 6. | Engstrøm T, Kelbæk H, Helqvist S, Høfsten DE, Kløvgaard L, Holmvang L, Jørgensen E, Pedersen F, Saunamäki K, Clemmensen P, De Backer O, Ravkilde J, Tilsted HH, Villadsen AB, Aarøe J, Jensen SE, Raungaard B, Køber L; DANAMI-3—PRIMULTI Investigators. Complete revascularisation vs treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015;386:665-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 605] [Cited by in RCA: 742] [Article Influence: 74.2] [Reference Citation Analysis (0)] |
| 7. | Smits PC, Abdel-Wahab M, Neumann FJ, Boxma-de Klerk BM, Lunde K, Schotborgh CE, Piroth Z, Horak D, Wlodarczak A, Ong PJ, Hambrecht R, Angerås O, Richardt G, Omerovic E; Compare-Acute Investigators. Fractional Flow Reserve-Guided Multivessel Angioplasty in Myocardial Infarction. N Engl J Med. 2017;376:1234-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 572] [Article Influence: 71.5] [Reference Citation Analysis (0)] |
| 8. | Calviño-Santos R, Estevez-Loureiro R, Bouzas-Mosqeura A, Peteiro J, Salgado-Fernández J, Rodríguez-Vilela A, Franco-Gutiérrez R, Rodríguez-Fernández JA, Mesías-Prego A, González-Juanatey C, Aldama-López G, Piñón-Esteban P, Flores-Ríos X, Soler-Martín R, Seoane-Pillado T, Vázquez-González N, Muñiz J, Vázquez-Rodríguez JM. Complete revascularisation vs stress echocardiography-guided revascularisation in patients with ST-segment elevation myocardial infarction and multivessel disease (CROSS-AMI): a clinical trial. Eur Heart J. 2017;38:436. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Calviño-Santos R, Estévez-Loureiro R, Peteiro J, Salgado-Fernández J, Rodríguez-Vilela A, Franco-Gutiérrez R, Bouzas-Mosquera A, Rodríguez-Fernández JA, Mesías-Prego A, González-Juanatey C, Aldama-López G, Piñón-Esteban P, Flores-Ríos X, Soler-Martín R, Seoane-Pillado T, Vázquez-González N, Muñiz J, Vázquez-Rodríguez JM. Angiographically-guided Complete revascularization vs selective stress echocardiography-guided revascularization in patients with ST-segment elevation myocardial infarction and multivessel disease: The CROSS-AMI Randomized Clinical Trial. Circ Cardiovasc Interv. 2019;12:e007924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Bouzas-Mosquera A, Peteiro J, Alvarez-García N, Broullón FJ, Mosquera VX, García-Bueno L, Ferro L, Castro-Beiras A. Prediction of mortality and major cardiac events by exercise echocardiography in patients with normal exercise electrocardiographic testing. J Am Coll Cardiol. 2009;53:1981-1990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 11. | Peteiro J, Bouzas-Mosquera A, Broullón FJ, Garcia-Campos A, Pazos P, Castro-Beiras A. Prognostic value of peak and post-exercise treadmill exercise echocardiography in patients with known or suspected coronary artery disease. Eur Heart J. 2010;31:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van' t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF; FAME Study Investigators. Fractional flow reserve vs angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2974] [Cited by in RCA: 3058] [Article Influence: 191.1] [Reference Citation Analysis (0)] |
| 13. | Escaned J, Collet C, Ryan N, De Maria GL, Walsh S, Sabate M, Davies J, Lesiak M, Moreno R, Cruz-Gonzalez I, Hoole SP, Ej West N, Piek JJ, Zaman A, Fath-Ordoubadi F, Stables RH, Appleby C, van Mieghem N, van Geuns RJ, Uren N, Zueco J, Buszman P, Iñiguez A, Goicolea J, Hildick-Smith D, Ochala A, Dudek D, Hanratty C, Cavalcante R, Kappetein AP, Taggart DP, van Es GA, Morel MA, de Vries T, Onuma Y, Farooq V, Serruys PW, Banning AP. Clinical outcomes of state-of-the-art percutaneous coronary revascularization in patients with de novo three vessel disease: 1-year results of the SYNTAX II study. Eur Heart J. 2017;38:3124-3134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 243] [Article Influence: 34.7] [Reference Citation Analysis (0)] |
| 14. | Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF, Windecker S; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:267-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4045] [Cited by in RCA: 4396] [Article Influence: 439.6] [Reference Citation Analysis (0)] |
| 15. | Fanning JP, Nyong J, Scott IA, Aroney CN, Walters DL. Routine invasive strategies vs selective invasive strategies for unstable angina and non-ST elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2016;CD004815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Boden WE, O'Rourke RA, Crawford MH, Blaustein AS, Deedwania PC, Zoble RG, Wexler LF, Kleiger RE, Pepine CJ, Ferry DR, Chow BK, Lavori PW. Outcomes in patients with acute non-Q-wave myocardial infarction randomly assigned to an invasive as compared with a conservative management strategy. Veterans Affairs Non-Q-Wave Infarction Strategies in Hospital (VANQWISH) Trial Investigators. N Engl J Med. 1998;338:1785-1792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 486] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 17. | Fox KA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, Tijssen JG, Lagerqvist B, Wallentin L; FIR Collaboration. Long-term outcome of a routine vs selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol. 2010;55:2435-2445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 412] [Cited by in RCA: 424] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 18. | Hoedemaker NPG, Damman P, Woudstra P, Hirsch A, Windhausen F, Tijssen JGP, de Winter RJ; ICTUS Investigators. Early Invasive Vs Selective Strategy for Non-ST-Segment Elevation Acute Coronary Syndrome: The ICTUS Trial. J Am Coll Cardiol. 2017;69:1883-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Henderson RA, Jarvis C, Clayton T, Pocock SJ, Fox KA. 10-Year Mortality Outcome of a Routine Invasive Strategy Vs a Selective Invasive Strategy in Non-ST-Segment Elevation Acute Coronary Syndrome: The British Heart Foundation RITA-3 Randomized Trial. J Am Coll Cardiol. 2015;66:511-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 20. | Wallentin L, Lindhagen L, Ärnström E, Husted S, Janzon M, Johnsen SP, Kontny F, Kempf T, Levin LÅ, Lindahl B, Stridsberg M, Ståhle E, Venge P, Wollert KC, Swahn E, Lagerqvist B; FRISC-II study group. Early invasive vs non-invasive treatment in patients with non-ST-elevation acute coronary syndrome (FRISC-II): 15 year follow-up of a prospective, randomised, multicentre study. Lancet. 2016;388:1903-1911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 21. | Hoedemaker NPG, Damman P, de Winter RJ. Reply: Early Revascularization in NSTE-ACS: Insights From the ICTUS Long-Term Follow-Up. J Am Coll Cardiol. 2017;70:1424-1425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |