Published online Oct 26, 2018. doi: 10.4330/wjc.v10.i10.187
Peer-review started: June 5, 2018
First decision: June 14, 2018
Revised: July 25, 2018
Accepted: July 22, 2018
Article in press: August 31, 2018
Published online: October 26, 2018
Processing time: 143 Days and 16.2 Hours
We report three cases of Takotsubo syndrome (TS) with atypical myocardial involvement. All three cases were triggered by physical or mental stress, resulting in transient myocardial compromise. However, the clinical presentation, localization and extent of myocardial damage varied in each case, ranging from low-risk acute chest pain to cardiogenic shock with low ejection fraction and dynamic obstruction of the left ventricular outflow tract. These cases outline the range of possible presentations of this rare entity and illustrate atypical forms of TS.
Core tip: Although less frequent, atypical presentations of Takotsubo syndrome - different from the classical apical ballooning - need prompt recognition by physicians. In addition to being a diagnostic challenge, this malady can present with severe complications, such as cardiogenic shock, arrhythmias and others. Herein, we show the presentation and management of atypical cases, with emphasis on their clinical recognition.
- Citation: Fuensalida A, Cortés M, Gabrielli L, Méndez M, Martínez A, Martínez G. Takotsubo syndrome - different presentations for a single disease: A case report and review of literature. World J Cardiol 2018; 10(10): 187-190
- URL: https://www.wjgnet.com/1949-8462/full/v10/i10/187.htm
- DOI: https://dx.doi.org/10.4330/wjc.v10.i10.187
Takotsubo syndrome (TS) was described almost 3 decades ago as an entity mainly affecting older women (post menopause), triggered by emotional stress, with ST-segment elevation on the electrocardiogram and with a characteristic pattern of apical ballooning of the left ventricle[1-3]. However, it is currently recognized that TS may have a more heterogeneous presentation, affecting also men, with different electrocardiographic alterations and diverse patterns of myocardial compromise[4,5]. These atypical TS cases may comprise up to 18% of cases[4,5].
We now describe three cases of atypical TS that presented at our institution and were managed by the authors between May 2014 and September 2016.
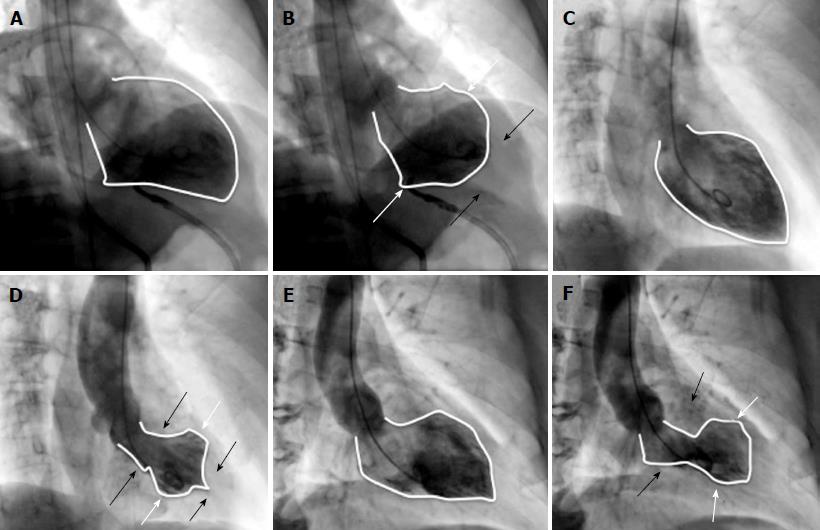
A 57-year-old man presented with irregular wide-complex tachyarrhythmia at 180 beats per minute during anaesthetic induction for elective pituitary macroadenoma surgery. He received intravenous (IV) propranolol and adenosine, after which he reverted to sinus rhythm. However, severe hemodynamic compromise ensued, requiring support with IV norepinephrine and pseudoephedrine. The electrocardiogram showed ST-segment depression from leads V1 to V5 and a transesophageal echocardiogram demonstrated diffuse left ventricular (LV) hypokinesis, with a left ventricular ejection fraction (LVEF) of 35%. Urgent coronary angiography showed absence of obstructive coronary artery disease in the epicardial arteries, whereas a LV angiogram confirmed an extensive area of akinesis involving the basal and middle segments of the anterior and inferior walls, with concomitant hyperkinesis of the apical segments (Figure 1A and 1B). An LVEF of 20% was estimated. Initial management included hemodynamic support with IV noradrenaline and dobutamine along with mechanical ventilation. Very rapid clinical improvement was evident and the patient was extubated 24 h after the event. High-sensitivity troponin peaked at 950 pg/mL. An echocardiogram performed 48 h later showed improvement in LVEF to 60%. Two months later, on beta-blockers, the macroadenoma was resected with no adverse events.
A 53-year-old woman with Parkinson’s disease arrived to the emergency department complaining of rest angina after suffering severe emotional stress while she was attending a trial in a police court, 4 h earlier. Electrocardiography showed sinus rhythm with antero-lateral ST-segment depression. Coronary angiography showed no obstructive disease in the epicardial coronary arteries and LV angiography revealed akinesis in the midventricular segments, with LVEF 60% (Figure 1C and D). High-sensitivity troponin peaked at 108 pg/mL. Trans-thoracic echocardiography at 24 h showed a normal size left ventricle with minimal infero-lateral hypokinesis and preserve global function. Three months later, echocardiography showed complete recovery of the infero-lateral defect.
A 70-year old female, with a prior history of hypertension and type-2 diabetes, presented to the emergency room with a 3-d history of intermittent oppressive chest pain, associated with dyspnoea and cough. On admission, she was tachycardic and hypotensive. The electrocardiogram showed sinus rhythm with ST-segment elevation in leads V1 to V4. Urgent coronary angiography revealed absence of obstructive coronary epicardial lesions and the left ventriculogram showed akinesis of the apex and anterior and inferior apical segments, associated with basal segment hypercontractility and severe mitral regurgitation (Figure 1D and F). The intraventricular pressure pullback showed a gradient at the level of the left ventricle outflow tract of 47 mmHg. She was urgently managed with intensive volume replacement with IV saline, resulting in a prompt recovery. Echocardiogram showed akinesis of the anterior and apical walls, with a LVEF of 45%. Peak high-sensitivity troponin was 240 pg/mL. Due to intense back pain and the presence of meningeal signs on physical examination, a magnetic resonance imaging of the spine was performed revealing spinal subarachnoid haemorrhage with a thrombosed aneurysm of the right posterior spinal artery at the T1-T2 level. She had uneventful neurological and cardiological recovery, and was discharged on beta-blockers, statins and acetylsalicylic acid. Follow-up echocardiogram at 1 mo showed complete recovery of the ventricular motion defect and a LVEF of 65%.
This case series highlights the heterogeneous clinical presentation of TS (Table 1). The affected myocardial segments were different in each case: (1) basal (or so called inverse TS); (2) midventricular and (3) apical with LV outflow tract obstruction and mitral regurgitation due to systolic anterior motion, secondary to hypercontractility of the basal segments. However, all three have in common the presence of a trigger factor (physical or emotional stress), dissociation between the magnitude of the myocardial damage extension and biomarker elevation, the absence of epicardial coronary disease on angiography and the complete or almost complete recovery of the defect during follow-up.
| Sex | Age | Trigger | Clinical presentation | ECG abnormalities | Type of motility defect | LVEF | Peak hsTroponin | Follow- up | Recurrence | |
| Case 1 | Male | 57 | Surgery / Anesthetic induction | Ventricular arrhythmia and cardiogenic shock | ST depression leads V1 to V5 QTc: 500 mseg | Basal | 35% | 950 pg/mL | 15 mo | No |
| Case 2 | Female | 53 | Emotional stress | Acute myocardial infarction without ST elevation | ST depression leads V4 to V6, DI and aVL | Midventricular | 60% | 108 pg/mL | 38 mo | No |
| QTc: 490 mseg | ||||||||||
| Case 3 | Female | 70 | Spinal aneurysm rupture | Acute myocardial infarction with ST elevation and shock | 2 mm ST elevation leads V1 to V4 | Apical ballooning, LV outflow tract obstruction | 45% | 240 pg/mL | 16 mo | No |
| QTc: 510 mseg |
The mechanisms resulting in TS are not yet fully understood, but the currently most accepted theories are transient myocardial dysfunction secondary to an exaggerated release of catecholamines, coronary vasospasm and transient microvascular dysfunction[3,6].
The management of acute heart failure is the mainstay of treatment, and in some patients it is necessary to provide support with vasoactive drugs and/or ventricular assistance to achieve hemodynamic stability[6,7]. Once the acute episode has been resolved, a favourable long-term prognosis is generally expected[3], although recent reports have challenged this notion[8]. Some series suggest that this entity can have an estimated annual rate of 9.9% major events and 5.6% mortality[5], in association with a recurrence risk of 5%-10%[6]. The magnitude of ventricular dysfunction is the main prognostic marker[4], although factors influencing late prognosis have not yet been clearly defined.
It has been reported that atypical TS has a better prognosis than the common form, which theoretically could be explained by the lesser amount of affected myocardium and better ventricular function[4], although information regarding such cases is scarce. Finally, we believe that clinicians caring for patients with myocardial infarction should be familiar with these less common presentations of TS, which should be considered in patients with acute coronary syndromes without obstructive coronary disease and with cardiac enzyme elevations lower than expected in relation to the degree of apparent myocardial damage, particularly when triggered by obvious emotional or physical stress.
Patients presenting as acute coronary syndrome with left ventricular (LV) dysfunction, shock or LV outflow tract obstruction, and in whom no stenosis were found in angiography and full recovery of LV abnormality was achieved.
Acute Coronary Syndrome, cardiogenic shock.
Acute coronary syndrome due to plaque rupture, spontaneous coronary artery dissection.
Eleveted highsensitive troponin, electrocardiogram with different abnormalities such as ST depression and elevation, as well as ventricular arrhythmias.
Coronary angiography with no coronary arteries stenosis. LV dysfunction with distinctive wall motion abnormalities not correlated to specific arterial segments. LV function recovery in follow-up echocardiogram.
Beta blockers, volume replacement.
Several reports of atypical cases with wall motion abnormalities different from apical ballooning. Retrospective study, InterTAK Registry, shows incidence about 10% to 18% of atypical cases.
Takotsubo syndrome (TS) is a cardiomyopathy that simulate acute coronary syndrome, but no coronary abnormalities are present in angiography. Wall motion abnormality typically presents as apical ballooning, however, in some cases (as presented in this report) different LV segments might be affected.
Myocardial compromise in TS is not limited to the classical apical involvement and clinical presentations can range from life-threatening hemodynamic compromise to low-risk chest pain. A normal coronary angiogram and discordant LV involvement are key diagnostic features. Prompt recognition of complications and subsequent treatment allow for a favourable prognosis.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: Chile
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Korosoglou G, Bagur R, Nurzynska D S- Editor: Dou Y L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Sato H, Tateishi H, Uchida T. Takotsubo-type cardiomyopathy due to multi- vessel spasm. Clinical aspect of myocardial injury: from ischemia to heart failure. Tokyo: Kagakuhyouronsya; 1990; 56–64. |
| 2. | Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155:408-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1193] [Cited by in RCA: 1297] [Article Influence: 76.3] [Reference Citation Analysis (0)] |
| 3. | Núñez Gil IJ, Andrés M, Almendro Delia M, Sionis A, Martín A, Bastante T, Córdoba Soriano JG, Linares Vicente JA, González Sucarrats S, Sánchez-Grande Flecha A; RETAKO investigators. Characterization of Tako-tsubo Cardiomyopathy in Spain: Results from the RETAKO National Registry. Rev Esp Cardiol (Engl Ed). 2015;68:505-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Ghadri JR, Cammann VL, Napp LC, Jurisic S, Diekmann J, Bataiosu DR, Seifert B, Jaguszewski M, Sarcon A, Neumann CA, Geyer V, Prasad A, Bax JJ, Ruschitzka F, Lüscher TF, Templin C; International Takotsubo (InterTAK) Registry. Differences in the Clinical Profile and Outcomes of Typical and Atypical Takotsubo Syndrome: Data From the International Takotsubo Registry. JAMA Cardiol. 2016;1:335-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 190] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 5. | Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Cammann VL, Sarcon A, Geyer V, Neumann CA. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373:929-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1401] [Cited by in RCA: 1717] [Article Influence: 171.7] [Reference Citation Analysis (1)] |
| 6. | Bybee KA, Prasad A. Stress-related cardiomyopathy syndromes. Circulation. 2008;118:397-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 395] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 7. | De Backer O, Debonnaire P, Gevaert S, Missault L, Gheeraert P, Muyldermans L. Prevalence, associated factors and management implications of left ventricular outflow tract obstruction in takotsubo cardiomyopathy: a two-year, two-center experience. BMC Cardiovasc Disord. 2014;14:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 8. | Scally C, Rudd A, Mezincescu A, Wilson H, Srivanasan J, Horgan G, Broadhurst P, Newby DE, Henning A, Dawson DK. Persistent Long-Term Structural, Functional, and Metabolic Changes After Stress-Induced (Takotsubo) Cardiomyopathy. Circulation. 2018;137:1039-1048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 201] [Article Influence: 25.1] [Reference Citation Analysis (0)] |