Peer-review started: December 8, 2017
First decision: December 11, 2017
Revised: December 25, 2017
Accepted: January 16, 2018
Article in press: January 16, 2018
Published online: January 26, 2018
Processing time: 48 Days and 15.7 Hours
We report a challenging case of a 81-year-old male with history of severe calcific aortic valve stenosis and aneurysmal membranous interventricular septum. The presence of anomalies in the sub-annular area can lead to valve malpositioning and its consequences. Transcatheter aortic valve implantation (TAVR) in patients with aneurysm of the perimembranous interventricular septum extending into the left ventricular outflow tract has not been previously reported. This case describes a successful transfemoral TAVR with an Edwards SAPIEN XT valve (Edwards Lifesciences, Irvine, CA, United States) with such anomaly.
Core tip: Congenital perimembranous ventricular septal aneurysm is reported to be rare and its co-occurrence with severe calcific aortic stenosis is even rarest. This unique case establishes that the transcatheter aortic valve replacement can be done in patients with aneurysmal perimembranous interventricular septum. This was achieved in our case by implanting the prosthetic valve more distally into the left ventricular outflow tract requiring apposition of the Edwards SAPIEN XT skirt at annulus with most of the valvular metallic frame in supra-annular position.
- Citation: Banga S, Barzallo MA, Nighswonger CL, Mungee S. Transcatheter aortic valve replacement in membranous interventricular septum aneurysm with left ventricular outflow tract extension. World J Cardiol 2018; 10(1): 1-5
- URL: https://www.wjgnet.com/1949-8462/full/v10/i1/1.htm
- DOI: https://dx.doi.org/10.4330/wjc.v10.i1.1
Extension of aneurysm in the left ventricular outflow tract (LVOT) from the perimembranous interventricular septum is a unique challenge with transcatheter aortic valve implantation (TAVR). The valve position in TAVR across the aortic annulus needs to be adequate for the proper deployment of the prosthetic valve. Presence of subvalvular aneurysm poses a challenge in effective valve deployment since there is always a possibility of serious negative outcome. The sub-annular, annular and supra-annular assessment of the landing zone is usually done using multi-imaging modality including transesophageal echocardiography (TEE) and multi-detector computer tomography (MDCT) .We describe a patient with perimembranous interventricular septum aneurysm extending into the LVOT requiring apposition of the Edwards SAPIEN XT skirt at annulus with most of the valvular metallic frame in supra-annular position.
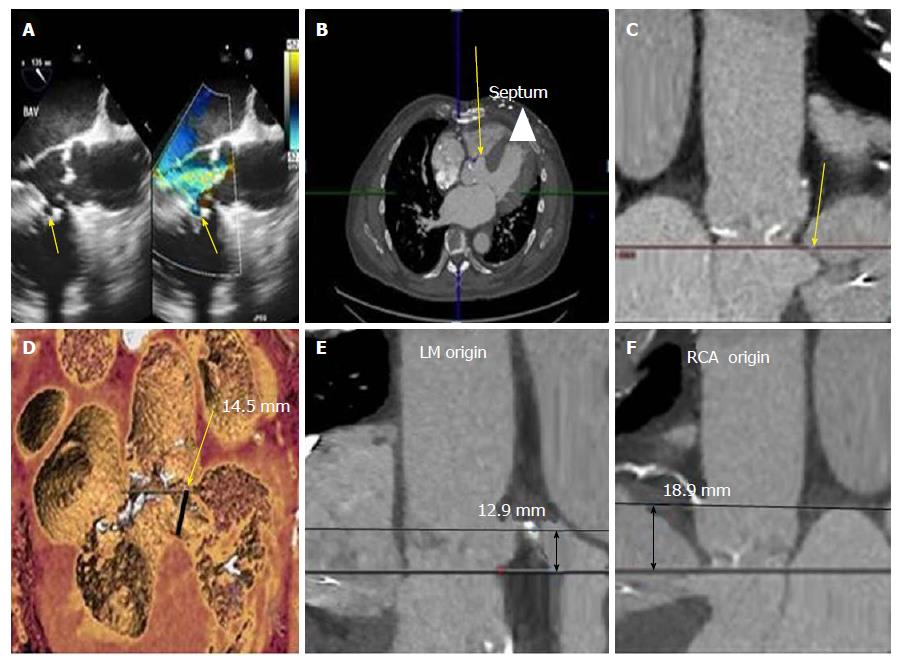
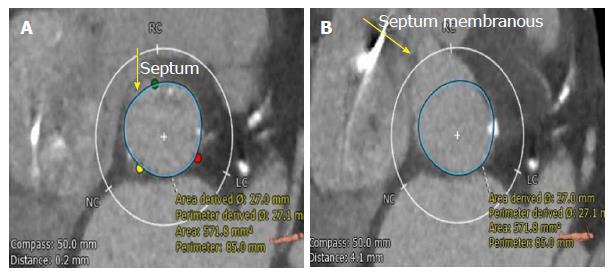
An 81-year-old male patient with post coronary artery bypass graft (CABG), pacemaker for 2:1 AV block and moderate chronic obstructive lung disease (COPD), history of TIA was planned for the TAVR for symptomatic severe aortic stenosis in view of high risk for open aortic valve replacement (Society of Thoracic Surgeons score of 8-12). He presented with recent worsening of shortness of breath. The high STS score in this patient was determined based on multiple factors which are part of the scoring criteria including presence of aortic insufficiency, previous CAD, Moderate COPD per PFT results, prior sternotomy/CABG. TEE showed a perimembranous ventricular septal aneurysm with LVOT extension and severe calcific stenotic aortic valve (AVA of 0.9 cm2) with moderate aortic regurgitation (Figure 1A). Pre-procedural CT findings confirmed the focal septal aneurysm below the aortic annulus in the transverse section (Figure 1B) and in the coronal section (Figure 1C). The aneurysm extended from 0.2 mm below the annulus to 14.5 mm along the septum on 3-D reconstructed CT image (Figure 1D). Distances from the aortic annulus to left main and right coronary ostium were 12.9 mm and 18.9 mm respectively (Figure 1E and F). The aortic annular measurements included: maximum and minimum diameter in the cross-sectional view of 29 mm and 25.5 mm respectively (average diameter of 27.3 mm); perimeter of 87.2 mm and annular area of 594.3 mm2. Figure 2A and B demonstrate the sub-annular area of 571.8 mm2 at the level of aneurysm in membranous septum. The aortic annular cross-sectional area on multi-planar reformatted en-face view was 602 mm2 (40% phase), suggesting a 29 mm Edwards SAPIEN XT valve.
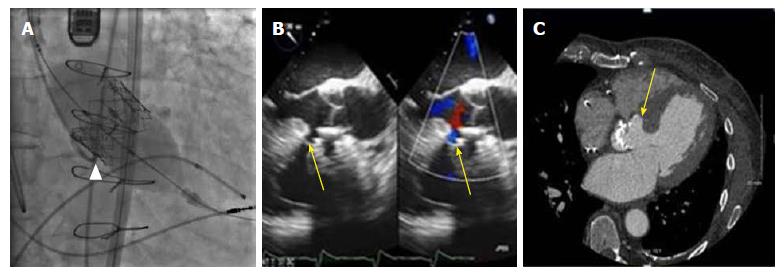
A 29 mm balloon-expandable transcatheter valve was positioned across the aortic annulus using the NovaFlex delivery system (Edwards Lifesciences, Irvine, CA, United States) after appropriate valve orientation by transfemoral approach. The Edwards SAPIEN XT prosthetic valve comes with the total frame height of 19.1 mm and skirt height of 12 mm. The valve was positioned at supra-annular position with 80% aortic and 20% ventricular ratio at the level of leaflet insertion of the native valve, given the presence of septal aneurysm with LVOT extension (Figure 3A). Appropriate valve deployment was achieved. No paravalvular aortic regurgitation with patent coronaries was noticed post-valve deployment (Figure 3B). The patient tolerated the procedure well and was discharged two days after procedure. At 8 week follow-up, patient had improved symptoms with repeat Cardiac CT scan showing stable prosthetic valve and no change in the perimembranous aneurysm (Figure 3C).
Congenital perimembranous ventricular septal aneurysms are not uncommon. Incidence of interventricular membranous septum aneurysm is reported to occur in 0.3 % of patients with congenital heart disease[1]. Etiology includes idiopathic or may be related to healed ventricular septal defect[1,2]. But there are few reports that relate the development to a previous episode of infection or trauma[3]. These aneurysms can be classified as true, false and pseudo-aneurysm[4]. Those with a wide base and regular contours are true while those with a narrow base and irregular shape are termed as false. A pseudo-aneurysm is complication of ischemic insults or transaortic septal myotomy[4]. Patients with interventricular septum aneurysm are often asymptomatic; if symptoms develop they are usually related to an associated complication. Like other aneurysms this anomaly predisposes patients to arrhythmogenic and thrombogenic events. Different modalities including conventional ventriculography, echocardiogram, cardiac MRI and MDCT are used for diagnosis. Morphological and functional assessment can be done with cardiac MRI or MDCT[4]. Both cardiac MRI and MDCT can also be used after surgery to determine the integrity of the patch and also to identify any residual defect but CT gives radiation exposure[4] .
Surgical intervention is rarely indicated except when concurrent heart diseases, hemodynamic abnormalities, and aneurysm-related complications are detected. Presence of thrombus may justify anticoagulation treatment[5]. Failure of anticoagulation therapy is an indication for surgical resection even in the absence of echocardiographic evidence of thrombus[5]. So periodic echocardiographic examination is recommended by some clinicians. Direct surgical ablation has shown satisfactory outcomes in patients with life threatening ventricular arrhythmias. Failure to precisely localize conduction system at the operation can lead to the development of complete heart block[6]. Although surgical option is available, most of them are left as such if they do not complicate. In our patient there was never a need to address it in the past. But as the patient was undergoing TAVR, the interventricular septum was assessed using imaging modalities.
Cardiac MDCT may be the optimal imaging modality to characterize not only the size and location of septal aneurysm[7,8], but also for pre-procedural TAVR planning. Proper assessment of the landing zone including the sub-valvular area below the aortic annulus and along the LVOT is essential. It has been seen that most favorable results are obtained during deployment when full coverage of the aortic leaflets is obtained with secure anchoring at and below the level of the insertion of the native valve leaflets. Based on these observations, the conventional recommendation is to implant the device with 50% above and 50% below native leaflet insertion[9]. But multiple positions have been documented in the literature showing variable ventricular device fractions below the anatomical annulus ranging from low to high[9]. Deployment of the Edwards SAPIEN XT prosthetic valve either getting positioned in a more sub-annular or more supra-annular location is quiet common. Most of the deployments are more supra-annular with varying aortic to ventricular ratio from 60:40 to 90:10.
The real-time imaging in the catheterization lab is inadequate for judgement of the level of leaflet insertion of the native valves. Therefore, the virtual basal ring, which is the anatomical annulus, is taken as the line of implantation during deployment. Malposition of valve can result in valve migration and resulting more severe para-valvular leak or embolization in high supra-annular placement vs more chances of AV conduction blocks in sub-annular placement[10]. Other complications including post TAVR shunts have also been reported[11]. Careful placement of the prosthetic valve in a more aortic position like in our case can be the solution despite the presence of aneurysm at the sub-aortic level. This placement does not affect the outcome provided the balloon-expandable valve is strategically placed more aortic than usual position, allowing the transcatheter valve skirt to completely cover the annulus reducing chances of paravalvular leak, as seen in our patient. Now Edward SAPIEN 3 is available which is a new fourth generation valve in the balloon-expandable Sapien series of devices and is easy to deploy due to its ultra-low delivery profile. At that time, the operators had good experience with Edward SAPIEN XT, and the new generation valve was under research. As per our knowledge, the present case is the first report of the utilization of TAVR procedure in a patient with interventricular septal aneurysm and need of higher aortic positioning with an Edward SAPIEN XT valve.
This case emphasizes the feasibility of doing TAVR in patients with interventricular septal aneurysm with LVOT extension. The present case also demonstrates the advantage of careful planning and strategic deployment of the TAVR prosthetic valve in patients with the above anomaly.
Patient with severe calcific aortic stenosis presented with worsening symptom of shortness of breath.
Patient was diagnosed as symptomatic severe aortic stenosis clinically.
Left ventricular outflow tract obstruction, sub-valvular aortic stenosis and supra-valvular aortic stenosis are the differentials.
ECG showed intermittent paced rhythm due to pacemaker and chest x-ray showed sternal wires due to previous coronary artery bypass graft.
Echocardiography and computer tomography showed severe calcific aortic stenosis with perimembranous interventricular septum aneurysm extending into left ventricular outflow tract.
Patient had congenital heart defect which included interventricular septum aneurysm extending into left ventricular outflow tract with acquired severe calcific stenosis of tri-leaflet aortic valve.
The patient was treated with transcatheter aortic valve replacement .This was achieved in our case by implanting the prosthetic valve more distally into the left ventricular outflow tract (LVOT) requiring apposition of the Edwards SAPIEN XT skirt at annulus with most of the valvular metallic frame in supra-annular position.
During transcatheter aortic valve replacement, normally the conventional recommendation is to implant the device with 50% above and 50% below native leaflet insertion .We had 80% aortic and 20% ventricular ratio of the device at the level of leaflet insertion of the native valve.
LVOT denotes left ventricular outflow tract obstruction and TAVR denotes transcatheter aortic valve replacement.
The transcatheter aortic valve replacement can be done in patients having high surgical risk with perimembranous interventricuar septum aneurysm by implanting the device more distally into the LVOT.
We acknowledge the valued contribution of Carmen Howard for editing the article.
Manuscript source: Unsolicited manuscript
Specialty type: Cardiac and cardiovascular systems
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Anan R, Chello M, Falconi M, Nunez-Gil IJJ, Sabate M, Said SAM, Teragawa H, Ueda H S- Editor: Cui LJ L- Editor: A E- Editor: Li RF
| 1. | Choi M, Jung JI, Lee BY, Kim HR. Ventricular septal aneurysms in adults: findings of cardiac CT images and correlation with clinical features. Acta Radiol. 2011;52:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Ramaciotti C, Keren A, Silverman NH. Importance of (perimembranous) ventricular septal aneurysm in the natural history of isolated perimembranous ventricular septal defect. Am J Cardiol. 1986;57:268-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Jain AC, Rosenthal R. Aneurysm of the membranous ventricular septum. Br Heart J. 1967;29:60-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Sharma M, Elmi F. Interventricular Membranous Septal Aneurysm Incidentally Diagnosed During Computed Tomographic Angiography in a Patient with Infrequent Supraventricular Tachycardia. Clin Pract. 2017;7:921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Salazar Mena J. [Echocardiographic detection of thrombus in an aneurysm of the interventricular membranous septum]. Rev Esp Cardiol. 2004;57:898; author reply 898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 6. | Yilmaz AT, Ozal E, Arslan M, Tatar H, Oztürk OY. Aneurysm of the membranous septum in adult patients with perimembranous ventricular septal defect. Eur J Cardiothorac Surg. 1997;11:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Komatsu S, Sato Y, Omori Y, Hirayama A, Okuyama Y, Kasiwase K, Fujisawa Y, Koshimune Y, Kiyomoto M, Shimizu T. Aneurysm of the membranous interventricular septum demonstrated by multislice computed tomography. Int J Cardiol. 2007;114:123-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Carcano C, Kanne JP, Kirsch J. Interventricular membranous septal aneurysm: CT and MR manifestations. Insights Imaging. 2016;7:111–117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Dvir D, Lavi I, Eltchaninoff H, Himbert D, Almagor Y, Descoutures F, Vahanian A, Tron C, Cribier A, Kornowski R. Multicenter evaluation of Edwards SAPIEN positioning during transcatheter aortic valve implantation with correlates for device movement during final deployment. JACC Cardiovasc Interv. 2012;5:563-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Masson JB, Kovac J, Schuler G, Ye J, Cheung A, Kapadia S, Tuzcu ME, Kodali S, Leon MB, Webb JG. Transcatheter aortic valve implantation: review of the nature, management, and avoidance of procedural complications. JACC Cardiovasc Interv. 2009;2:811-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 302] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 11. | Rojas P, Amat-Santos IJ, Cortés C, Castrodeza J, Tobar J, Puri R, Sevilla T, Vera S, Varela-Falcón LH, Zunzunegui JL. Acquired Aseptic Intracardiac Shunts Following Transcatheter Aortic Valve Replacement: A Systematic Review. JACC Cardiovasc Interv. 2016;9:2527-2538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |