Published online Nov 27, 2016. doi: 10.4240/wjgs.v8.i11.761
Peer-review started: June 26, 2016
First decision: August 5, 2016
Revised: August 19, 2016
Accepted: September 7, 2016
Article in press: September 8, 2016
Published online: November 27, 2016
Processing time: 149 Days and 17.9 Hours
Sclerosing mesenteritis is a rare pathology with only a few described cases in the literature. The etiology is unclear; however, several potential triggers, including abdominal surgery and abdominal trauma, have been discussed. The pathology includes a benign acute or chronic inflammatory process affecting the adipose tissue of the mesenterium. Despite it being a rare disease, sclerosing mesenteritis is an important differential diagnosis in patients after abdominal surgery or patients presenting spontaneously with signs of acute inflammation and abdominal pain. We present here three cases with sclerosing mesenteritis. In two cases, sclerosing mesenteritis occurred postoperatively after abdominal surgery. One patient was treated because of abdominal pain and specific radiological signs revealing spontaneous manifestation of sclerosing mesenteritis. So far there are no distinct treatment algorithms, so the patients were treated differently, including steroids, antibiotics and watchful waiting. In addition, we reviewed the current literature on treatment options for this rare disease.
Core tip: Sclerosing mesenteritis is a rare pathology including a benign acute or chronic inflammatory process affecting the adipose tissue of the mesenterium. The etiology is unclear; however, several potential triggers, including abdominal surgery and abdominal trauma, have been discussed. So far there is no evidence in the treatment of these patients. But, in the case of a non-resolving bowel obstruction, surgery is needed.
- Citation: Klasen J, Güller U, Muff B, Candinas D, Seiler CA, Fahrner R. Treatment options for spontaneous and postoperative sclerosing mesenteritis. World J Gastrointest Surg 2016; 8(11): 761-765
- URL: https://www.wjgnet.com/1948-9366/full/v8/i11/761.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v8.i11.761
Sclerosing mesenteritis is a rare, benign pathology of the abdominal adipose tissue[1]. It was first described by Jura[2] in 1924. Sclerosing mesenteritis, mesenteric or omental panniculitis, mesenteric lipodystrophy, or mesenteric manifestation of Weber-Christian disease are often used as synonymous terms[1,3]. The etiology is unclear and often remains idiopathic, but abdominal surgical procedures, abdominal trauma, infections, autoimmune processes, drugs, vasculitis, avitaminosis and hypersensitivity have been discussed as potential triggers[1,3,4]. The symptoms of sclerosing mesenteritis are mostly unspecific. Hence, it is crucial to rule out other pathologies such as lymphoma, sarcoma, peritoneal mesothelioma, infectious diseases (tuberculosis or histoplasmosis) or amyloidosis[3].
The objective of these case presentations and the summary of the literature is to raise awareness regarding this rare, yet important, differential diagnosis in a patient presenting with signs of acute inflammation and abdominal pain. Furthermore, the current literature regarding possible treatment regimens will be discussed.
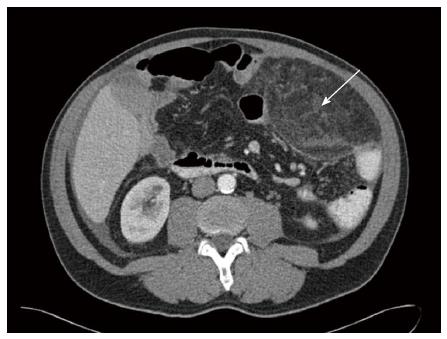
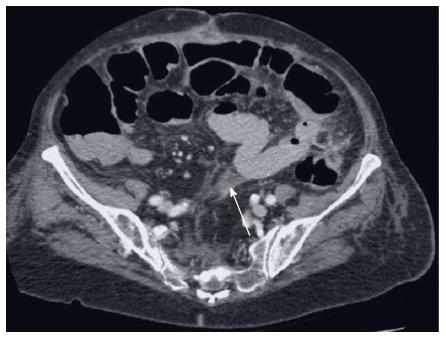
A 64 years old male patient with attenuated familial polyposis coli was electively admitted for laparoscopic subtotal colectomy. His previous surgical history consisted of inguinal hernia repair. Comorbidities included coronary artery disease, status post percutaneous transluminal coronary angiography and stenting two years earlier. Laparoscopic subtotal colectomy, including an ileo-rectal anastomosis and preservation of the greater omentum, was performed without any intraoperative complications. After an uneventful initial course, the patient developed symptoms of incomplete intestinal obstruction with vomiting and diarrhea on the third postoperative day. Moreover, the temperature rose to 101.3 degrees Fahrenheit. On clinical examination, the patient was very tender over his left hemiabdomen. The blood work revealed a dramatic elevation of the C-reactive protein (CRP) to 478 mg/L (normal: Less than 3 mg/L) and a white blood cell count of 16.1 G/l (normal: Less than 10.0 G/L). An abdominal computed tomography (CT) showed an unclear mass of 15 cm × 8.8 cm × 7.8 cm in the left hemiabdomen (Figures 1 and 2), consisting of omental fat and causing a partial intestinal obstruction. After administration of intravenous antibiotics (tazobactum/piperacillinum) and conservative treatment of the bowel obstruction with insertion of a naso-gastric tube and rectal catheter, the patient’s general condition improved and the bowel function normalized over the following days. The abdominal tenderness disappeared and the blood values returned to within normal limits. The patient was discharged with oral antibiotics (amoxicillinum/acidum clavulanicum) on postoperative day 20 in good general condition. The patient, who was seen in the outpatient clinic 4 wk later, remained asymptomatic.
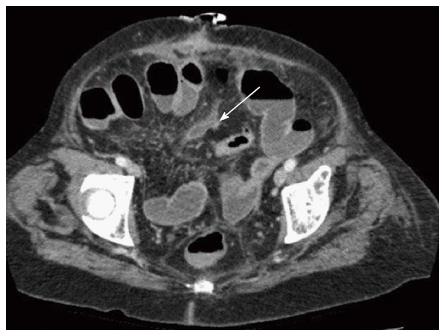
An 84 years old female patient was referred to the hospital with upper abdominal pain associated with diarrhea and vomiting for one week. The CT scan confirmed the diagnosis of an intestinal obstruction. An explorative laparotomy with adhesiolysis and a partial resection of the small bowel with an end-end-anastomosis of the small bowel was performed because of an ischemic perforation. During the postoperative course, the patient complained of progressive and vague abdominal pain. In addition to elevated inflammatory parameters (CRP, white blood cell count), no surgical complication or infection was detected. The repeated CT scans showed signs of mesenteritis without signs of leakage or abscess (Figures 3 and 4). There was no improvement with antibiotic treatment, but empirical therapy with prednisolone reduced the pain and the inflammatory parameters decreased. In the follow-up 40 d after surgery, the patient was asymptomatic.
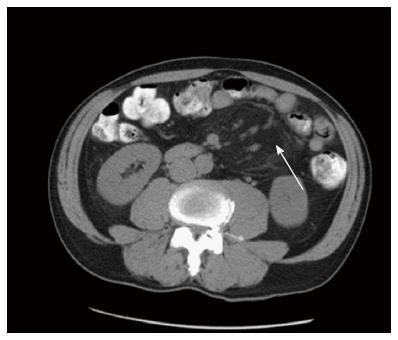
A healthy 56-year old male patient presented with history of pain in the lower abdominal quadrant for 3 to 4 mo, provoked by exercise. The patient’s past medical history was uneventful, with no weight loss, no episodes of fever or shivering, no evidence for dysfunction of the gastrointestinal tract, and no previous abdominal surgeries. The patient underwent a screening colonoscopy without any pathologic findings. A clinical examination revealed abdominal distention in the left lower quadrant without peritonitis or resistance. An abdominal CT scan showed an inflammatory infiltration of the mesenteric adipose tissue with lymphadenopathy, interpreted as sclerosing mesenteritis without evidence of malignancy or other pathology (Figures 5 and 6). The pain declined further in the course spontaneously without any treatment.
There are only a few described cases of sclerosing mesenteritis in the literature. The pathogenesis of sclerosing mesenteritis remains to be elucidated; however, it seems to be an inflammatory and immune response to local stimuli, such as abdominal surgery or trauma. Moreover, infections, autoimmune processes, malignancy, drugs, vasculitis, avitaminosis and hypersensitivity have been described as potential causes for sclerosing mesenteritis[5-7]. Furthermore, immunological disorders, such as elevated IgG4 levels, have been discussed as related to the occurrence of sclerosing mesenteritis[8,9]. However, the causes for sclerosing mesenteritis often remain idiopathic[1,3,4]. Histological exams reveal a benign fibro-inflammatory process of the intra-abdominal fat, including fat necrosis, signs of chronic inflammation with lymphocytes, plasma cells, lipid-laden macrophages and fibrosis. However, no malignant cells are identified[1,4,10]. The symptoms of sclerosing mesenteritis are nonspecific and may include fever, vomiting, abdominal pain with distension, abdominal tenderness as well as intestinal obstruction[3,11,12]. Because of its nonspecific presentation, it is crucial to rule out other pathologies, such as lymphoma, sarcoma, peritoneal mesothelioma, infectious diseases (tuberculosis or histoplasmosis) or amyloidosis and post-interventional abscesses and other complications[3]. Differentiating between a ”real” postoperative/post-interventional complication and a sclerosing mesenteritis may be extremely challenging. As sclerosing mesenteritis is extremely rare, it is often difficult to establish a definitive diagnosis[13]. Due to the nonspecific clinical presentation, a surgical biopsy is often performed[12]; however, it is rarely actually necessary[3]. It used to be the only method to confirm the diagnosis. Today, based on the increasing use of ultrasonography and CT scan with improved quality, the diagnosis can be established based on imaging and clinical presentation[10]. In ultrasonography the features are nonspecific, including a poorly defined hyperechoic mesenteric fat with a decreased compressibility[10]. CT scans reveal a well-defined mass of fatty tissue with increased density in comparison to normal fat or a nonspecific inflammatory process involving the adipose tissue of the mesenterium of the small bowel[10,14]. In addition, a fat-ring sign, a tumoral pseudocapsule or soft-tissue nodules may be observed[10]. Clinical manifestations are nonspecific and can consist of abdominal pain (70%), diarrhea (25%), weight loss (23%), abdominal muscle defense (50%), rebound tenderness (10%-15%), ascites/chylous (14%)[3,7] and, in rare cases, fever[15]. Most patients with sclerosing mesenteritis have an uneventful course and the symptoms resolve spontaneously[3]. Several therapeutic approaches with agents such as steroids, colchicine and azathioprine have been described with various therapeutic effects[16-18]. In cases of non-resolving bowel obstruction or an advanced inflammatory reaction, surgical resection of the inflamed fat may be necessary[1,12]. Asymptomatic sclerosing mesenteritis requires no therapy[7]. However, the symptomatic sclerosing mesenteritis must be treated surgically or with a trial of immunosuppressive medication[7].
These case presentations reflect that currently the etiology and the treatment of sclerosing mesenteritis are still not fully understood and further investigations are needed. The only evidence in the treatment of these patients is that, in the case of non-resolving bowel obstruction, surgery is needed. Because of the small number of patients suffering from sclerosing mesenteritis, prospective and randomized trials are difficult to perform. Therefore, it is still under investigation if patients need immunosuppressive agents.
Abdominal pain and signs of acute inflammation after abdominal surgery, with specific radiological signs in two patients and in one patient without prior surgical intervention.
Nonspecific with signs of acute inflammation and abdominal pain.
Lymphoma, sarcoma, peritoneal mesothelioma, infectious diseases (tuberculosis or histoplasmosis) or amyloidosis and post-interventional abscesses.
Elevated C-reactive protein levels and increased white blood count.
Steroids, antibiotics and watchful waiting. In the case of non-resolving bowel obstruction or an advanced inflammatory reaction, surgical resection is needed.
In the current literature, there are several case reports of mostly single cases. Data from prospective and randomized studies are lacking.
Sclerosing mesenteritis is a rare pathology and the etiology is unclear. Several potential triggers, including abdominal surgery and abdominal trauma, have been discussed. The pathology includes a benign acute or chronic inflammatory process affecting the adipose tissue of the mesenterium.
This disease is rare and often misdiagnosed. Especially in the postoperative course, the occurrence of sclerosing mesenteritis is often difficult to identify. The etiology is unclear and there are currently no specific treatment algorithms. The only evidence is that in the case of non-resolving bowel obstruction or an advanced inflammatory reaction, surgical resection is needed.
It is a well written clinical report about the rarely occurring sclerosing mesenteritis including three cases with pictorial presentation. The information conveyed should be of help to the peers in the same field for improving their clinical practice.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Switzerland
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Misiakos DPP, Ni Y, Surlin VM S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Popkharitov AI, Chomov GN. Mesenteric panniculitis of the sigmoid colon: a case report and review of the literature. J Med Case Rep. 2007;1:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Jura V. Sclerosing and retractile mesenteritis. Policlinica. 1924;31:575-581. |
| 3. | Issa I, Baydoun H. Mesenteric panniculitis: various presentations and treatment regimens. World J Gastroenterol. 2009;15:3827-3830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 76] [Cited by in RCA: 74] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 4. | Hirono S, Sakaguchi S, Iwakura S, Masaki K, Tsuhada K, Yamaue H. Idiopathic isolated omental panniculitis. J Clin Gastroenterol. 2005;39:79-80. [PubMed] |
| 5. | van Putte-Katier N, van Bommel EF, Elgersma OE, Hendriksz TR. Mesenteric panniculitis: prevalence, clinicoradiological presentation and 5-year follow-up. Br J Radiol. 2014;87:20140451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Badet N, Sailley N, Briquez C, Paquette B, Vuitton L, Delabrousse É. Mesenteric panniculitis: still an ambiguous condition. Diagn Interv Imaging. 2015;96:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Forcione DG, Lamont JT, Grover S. Sclerosing mesenteritis. 2011;UpToDate Available from: http://cursoenarm.net/UPTODATE/contents/mobipreview.htm?5/61/6096?source=HISTORY. |
| 8. | Harvin G, Graham A. Sclerosing Mesenteritis: A Rare Cause of Small Bowel Obstruction. Case Rep Gastroenterol. 2016;10:63-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Chen TS, Montgomery EA. Are tumefactive lesions classified as sclerosing mesenteritis a subset of IgG4-related sclerosing disorders? J Clin Pathol. 2008;61:1093-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | van Breda Vriesman AC, Schuttevaer HM, Coerkamp EG, Puylaert JB. Mesenteric panniculitis: US and CT features. Eur Radiol. 2004;14:2242-2248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Ruiz-Tovar J, Alonso Hernández N, Sanjuanbenito Dehesa A, Martínez Molina E. [Mesenteric paniculitis: report of ten cases]. Rev Esp Enferm Dig. 2007;99:240-241. [PubMed] |
| 12. | Delgado Plasencia L, Rodríguez Ballester L, López-Tomassetti Fernández EM, Hernández Morales A, Carrillo Pallarés A, Hernández Siverio N. [Mesenteric panniculitis: experience in our center]. Rev Esp Enferm Dig. 2007;99:291-297. [PubMed] |
| 13. | Volpicelli G, Saracco W. A case of mesenteric panniculitis: multiple involvement of the emergency department before final diagnosis and appropriate treatment. Eur J Emerg Med. 2007;14:104-105. [PubMed] |
| 14. | Canyigit M, Koksal A, Akgoz A, Kara T, Sarisahin M, Akhan O. Multidetector-row computed tomography findings of sclerosing mesenteritis with associated diseases and its prevalence. Jpn J Radiol. 2011;29:495-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Hirano H, Yoshida A, Sasae Y, Sakuta T, Morita Y. Mesenteric panniculitis: a rare cause of fever. Int J Rheum Dis. 2012;15:e40-e42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Miyake H, Sano T, Kamiya J, Nagino M, Uesaka K, Yuasa N, Oda K, Nimura Y. Successful steroid therapy for postoperative mesenteric panniculitis. Surgery. 2003;133:118-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Tytgat GN, Roozendaal K, Winter W, Esseveld MR. Successful treatment of a patient with retractile mesenteritis with prednisone and azathioprine. Gastroenterology. 1980;79:352-356. [PubMed] |
| 18. | Fasoulas K, Beltsis A, Katsinelos T, Dimou E, Arvaniti M, Charsoula A, Gourvas V, Atmatzidis S, Chatzimavroudis G, Katsinelos P. Efficacy of colchicine in the treatment of mesenteric panniculitis in a young patient. Saudi J Gastroenterol. 2012;18:146-148. [PubMed] |