Published online Jul 27, 2015. doi: 10.4240/wjgs.v7.i7.102
Peer-review started: January 28, 2015
First decision: March 6, 2015
Revised: May 11, 2015
Accepted: June 1, 2015
Article in press: June 2, 2015
Published online: July 27, 2015
Processing time: 183 Days and 2 Hours
Liver resection (LR) for hepatocellular carcinoma (HCC) in patients with chronic liver disease (CLD) is associated with high risks of developing significant postoperative complications and multicentric metachronous lesions, which can result in the need for repeated treatments. Studies comparing laparoscopic procedures to open LR consistently report reduced blood loss and transfusions requirements, lower postoperative morbidity, and shorter hospital stays, with no differences in oncologic outcomes. In addition, laparoscopic LR is associated with reduced postoperative ascites and a lower incidence of liver failure for HCC patients with CLD, due to the reduced surgery-induced parenchymal injury to the residual liver and limited destruction of the collateral blood/lymphatic flow around the liver. Finally, this procedure facilitates subsequent repeat LR due to minimal adhesion formation and improved vision/manipulation between adhesions. These characteristics of laparoscopic LR may lead to an expansion of the indications for LR. This editorial is based on the review and meta-analysis presented at the 2nd International Consensus Conference on Laparoscopic Liver Resection in Iwate, Japan, in October 2014 (Chairperson of the congress is Professor Go Wakabayashi from the Department of Surgery, Iwate Medical University School of Medicine), which is published in the Journal of Hepato-Biliary-Pancreatic Sciences.
Core tip: Liver resection (LR) for hepatocellular carcinoma patients with chronic liver disease has high risks for developing significant postoperative complications and multicentric metachronous lesions with need of repeated treatments. Laparoscopic LR has advantages of reduced surgery-induced parenchymal injury and destruction of the collateral blood/lymphatic flow, which leads to reduced production of postoperative ascites, and facilitates repeat LR because of reduced adhesion formation and improved vision/manipulation between adhesions. These characteristics of laparoscopic LR may lead to expansion of the indications for LR.
- Citation: Morise Z. Perspective of laparoscopic liver resection for hepatocellular carcinoma. World J Gastrointest Surg 2015; 7(7): 102-106
- URL: https://www.wjgnet.com/1948-9366/full/v7/i7/102.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i7.102
Hepatocellular carcinoma (HCC) is among the most common primary cancers and causes of cancer-related deaths[1,2]. The options for HCC treatment include transarterial chemoembolization and local ablation therapy[3], but the best chance for cure is with liver resection (LR)[4] or liver transplantation[5]. Liver transplantation should be considered in patients with deteriorating liver function who are within the Milan criteria[6], whereas LR should be considered for those with preserved liver function[7,8]. However, most HCC patients are at high risk for developing significant postoperative complications and multicentric metachronous lesions with underlying chronic liver disease (CLD). For these patients, the oncologic therapeutic effects and degree of invasive surgical stress, especially to the impaired liver, should be considered during the treatments. The variety of symptoms in patients with CLD[9] raises the risks associated with anesthesia and surgery[10], which increase according to the preoperative Child-Pugh class[11]. For severe CLD patients, refractory ascites often develop even with limited LR, which then leads to fatal liver failure[12,13].
Currently, the treatment choice for an HCC patient with CLD depends on the combination of tumor and liver conditions[14]. Nevertheless, there are still a considerable number of these patients who are unable to undergo one of the treatment modalities listed above. Such patients may benefit from less-invasive laparoscopic LR (LLR)[15] compared to open LR (OLR)[16]. Indeed, this procedure has recently been evaluated in a review and meta-analysis[17], which was presented at the 2nd International Consensus Conference on Laparoscopic Liver Resection in Iwate, Japan, in October 2014 (the Chairperson of the Congress is Professor Go Wakabayashi from the Department of Surgery, Iwate Medical University School of Medicine).
For the review and meta-analysis[17], 2183 and 466 articles were identified under a PubMed search of “laparoscopic liver resection” and “laparoscopic liver resection + hepatocellular carcinoma,” respectively. No randomized trials were available. All data were reported as case series, case-control studies, reviews, and meta-analyses. Of these, there was one Cochrane review and 81 comparative studies for LLR, as well as 12 meta-analyses for all types of indications[18-22], colorectal metastases[23,24], left lateral sectionectomy[25], and HCC[26].
In the absence of randomized studies, the Cochrane study could not draw any conclusions. The meta-analyses generally showed that LLR reduced blood loss, transfusion requirements and complication rates, shortened the hospital stay, and resulted in identical or better surgical margins than OLR. Several analyses examined long-term results and showed no differences in oncologic outcomes between LLR and OLR.
The indications for LLR are essentially the same as those for OLR. However, the centers reported in these studies identified technical feasibilities related to tumor conditions (such as size, and location) and extent of resection as the limiting factors. Typically, giant tumors (> 10-15 cm in diameter) are excluded from the indications for LLR due to the lack of appropriate view of operative field in the small abdominal cavity. Also, LR combined with major vessel resection and reconstruction and living-donor LR for transplantation are performed at only a few experienced centers. A previous international survey[27] reported a relatively small percentage (approximately 40%) of LLR procedures with some groups of higher rates over 80%. Although the low rate and disparity of LLR application could lead to selection bias in the reported results, the studies showed that LLR generally produced better perioperative outcomes without compromising long-term oncologic outcome for the patients selected to undergo these procedures.
Patients who undergo LR are exposed to three different types of stresses that are of particular importance in patients with CLD: (1) general, whole-body surgical stress; (2) reduced liver function due to resected liver volume; and (3) surgery-induced injury to the area around the liver (caused by destruction of the collateral blood and lymphatic flow with laparotomy and mobilization of the liver) and residual liver parenchyma (caused by mesenchymal injury from the compression of the liver). With LLR, the reduced surgery-induced injury can lower the risk of refractory ascites, leading to less successive complications and a smooth recovery without liver failure.
Among the studies in the review, HCC cases were included in four meta-analyses[26,28-30] (with 494 to 1238 patients) and 23 comparative studies[31-53], 13 of which[31-36,41,43,44,49-51,53] examined the rates of postoperative ascites and liver failure. We conducted a meta-analysis for postoperative ascites and liver failure in nine and six of these studies that were of a high quality[17]. The analysis showed reduced incidences of postoperative ascites (odds ratio 0.26, 95%CI: 0.14-0.49; P < 0.001) and liver failure (odds ratio 0.24, 95%CI: 0.10-0.56; P = 0.001), which are associated with LLR.
The impact of LLR on ascites production and liver failure depends on the severity of the background CLD, extent of the resection, and the operative technique (extent of dissection of the peritoneal attachments and adhesions). There are six comparative studies from five institutions in which all patients with HCC had liver cirrhosis[31,33,36,42,45,53]. Among them, all three studies[31,33,53] that examined postoperative ascites production showed a significant reduction with LLR. Another study compared the perioperative results after LLR between patients with severe cirrhosis (Child-Pugh B/C and ICG R15 ≥ 40%) and with mild-moderate cirrhosis[54]. Although it was a retrospective small-sized non-matched study, it showed comparable short-term outcomes, including postoperative ascites production, in these patients. The positive results from these well-designed studies examining the outcome of LLR for severe cirrhotic patients could lead to expansion of the indications for LLR.
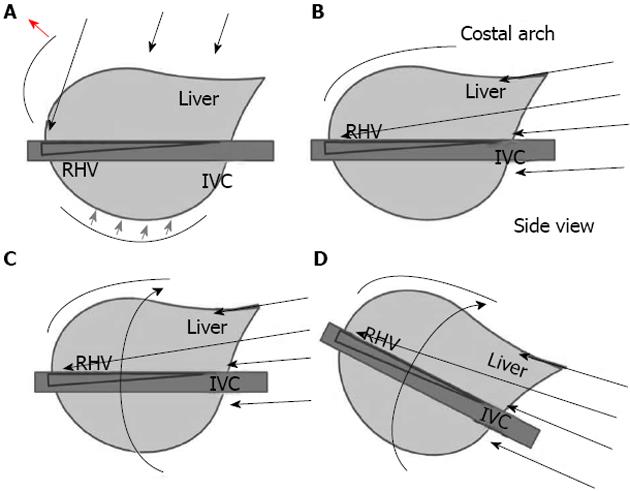
Additional benefits of LLR in other aspects were found in other studies. The development of fewer adhesions with laparoscopic surgery was found to facilitate subsequent surgeries[55]. With the initial LR performed in laparoscopic approach, the subsequent salvage transplantation requires a shorter operative time, with reduced blood loss and fewer transfusions[56]. Furthermore, recurrence with potential multicentric metachronous lesions is an important issue for HCC patients with CLD. Repeat LR increases the difficulty of LR as a result of modifications to the anatomy and the formation of adhesions. Two studies[57,58] compared laparoscopic and open procedures with regard to repeat LR. The operating time of repeat LLR was significantly shorter with previous LLR compared to OLR. In addition, repeat LLR was associated with reduced blood loss and postoperative morbidity, and a shorter hospital stay compared with repeat OLR regardless of the approach used in the previous LR. The benefit of LLR for repeat procedures may be due to a reduced need for adhesiolysis because of the specific view and approach/manipulation of LLR (Figure 1)[59-61]. This may also cause the reduction of surgery-induced injury on the liver and the area surrounding it.
The advantages of LLR for HCC patients with CLD include reductions of surgery-induced parenchymal injury and destruction of the collateral blood/lymphatic flow around the liver. LLR also minimizes the production of postoperative ascites and results in fewer subsequent fatal complications. The formation of fewer adhesions and improved vision and manipulation between adhesions facilitates subsequent repeat LR procedures. These characteristics of LLR may lead to expansion of the indications for LR for these patients (Table 1). However, further investigations are required to document the benefits of LLR in specific conditions.
| Patient group | Indications |
| Patients with severe liver dysfunction (Child-Pugh B/C) | LLR for subcapsular HCCs, particularly for the tumors on suspended ruptures |
| LLR as the bridging therapy to liver transplantation, with the advantage of examination and evaluation of tumor pathology before transplantation | |
| LLR for HCCs in the patients with hepatitis B virus-related severe liver dysfunction without previous antiviral treatments who could acquire the recovery of liver function after antiviral treatments[62] | |
| Patients with repeat lesions | Repeat LLR for the patients with deteriorated liver function and multicentric metachronous HCCs who have undergone multiple treatments and are usually treated with local ablation therapy, transarterial chemoembolization, or sorafenib |
P- Reviewer: Gatselis NK, Penkova-Radicheva MP, Uchiyama H S- Editor: Song XX L- Editor: A E- Editor: Yan JL
| 1. | El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557-2576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3846] [Cited by in RCA: 4267] [Article Influence: 237.1] [Reference Citation Analysis (2)] |
| 2. | Schütte K, Bornschein J, Malfertheiner P. Hepatocellular carcinoma--epidemiological trends and risk factors. Dig Dis. 2009;27:80-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 309] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 3. | Lau WY, Leung TW, Yu SC, Ho SK. Percutaneous local ablative therapy for hepatocellular carcinoma: a review and look into the future. Ann Surg. 2003;237:171-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 179] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 4. | Capussotti L, Ferrero A, Viganò L, Polastri R, Tabone M. Liver resection for HCC with cirrhosis: surgical perspectives out of EASL/AASLD guidelines. Eur J Surg Oncol. 2009;35:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Hwang S, Lee SG, Belghiti J. Liver transplantation for HCC: its role: Eastern and Western perspectives. J Hepatobiliary Pancreat Sci. 2010;17:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. [PubMed] |
| 7. | Ryder SD. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut. 2003;52 Suppl 3:iii1-iii8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 220] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 8. | Cha CH, Ruo L, Fong Y, Jarnagin WR, Shia J, Blumgart LH, DeMatteo RP. Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg. 2003;238:315-321; discussion 321-323. [PubMed] |
| 9. | Hoeper MM, Krowka MJ, Strassburg CP. Portopulmonary hypertension and hepatopulmonary syndrome. Lancet. 2004;363:1461-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 283] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 10. | Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology. 1999;90:42-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 224] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 11. | Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery. 1997;122:730-735; discussion 735-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 308] [Cited by in RCA: 250] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 12. | Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000;191:38. [RCA] [DOI] [Full Text] [Cited by in Crossref: 800] [Cited by in RCA: 799] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 13. | Lai EC, Fan ST, Lo CM, Chu KM, Liu CL, Wong J. Hepatic resection for hepatocellular carcinoma. An audit of 343 patients. Ann Surg. 1995;221:291-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 319] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 14. | Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, Kubota K, Zucchi A. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg. 1999;134:984-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 352] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 15. | Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc. 1992;6:97-98. |
| 16. | Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, Watanabe M, Tamura A. Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. J Hepatobiliary Pancreat Surg. 2009;16:433-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 17. | Morise Z, Ciria R, Cherqui D, Chen KH, Belli G, Wakabayashi G. Can We Expand theIndicationsfor Laparoscopic Liver Resection? A Systematic Review and Meta-Analysis of Laparoscopic Liver Resection for Patients with Hepatocellular Carcinoma and Chronic Liver Disease. J Hepatobiliary Pancreat Sci. 2015;In press. |
| 18. | Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, Antoniou A. Laparoscopic versus open hepatic resections for benign and malignant neoplasms--a meta-analysis. Surgery. 2007;141:203-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 260] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 19. | Croome KP, Yamashita MH. Laparoscopic vs open hepatic resection for benign and malignant tumors: An updated meta-analysis. Arch Surg. 2010;145:1109-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 116] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 20. | Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, Sutcliffe RP. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford). 2011;13:295-308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 174] [Cited by in RCA: 167] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 21. | Mizuguchi T, Kawamoto M, Meguro M, Shibata T, Nakamura Y, Kimura Y, Furuhata T, Sonoda T, Hirata K. Laparoscopic hepatectomy: a systematic review, meta-analysis, and power analysis. Surg Today. 2011;41:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Rao A, Rao G, Ahmed I. Laparoscopic or open liver resection? Let systematic review decide it. Am J Surg. 2012;204:222-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Zhou Y, Xiao Y, Wu L, Li B, Li H. Laparoscopic liver resection as a safe and efficacious alternative to open resection for colorectal liver metastasis: a meta-analysis. BMC Surg. 2013;13:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Wei M, He Y, Wang J, Chen N, Zhou Z, Wang Z. Laparoscopic versus open hepatectomy with or without synchronous colectomy for colorectal liver metastasis: a meta-analysis. PLoS One. 2014;9:e87461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Rao A, Rao G, Ahmed I. Laparoscopic left lateral liver resection should be a standard operation. Surg Endosc. 2011;25:1603-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Yin Z, Fan X, Ye H, Yin D, Wang J. Short- and long-term outcomes after laparoscopic and open hepatectomy for hepatocellular carcinoma: a global systematic review and meta-analysis. Ann Surg Oncol. 2013;20:1203-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 160] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 27. | Hibi T, Cherqui D, Geller DA, Itano O, Kitagawa Y, Wakabayashi G. International Survey on Technical Aspects of Laparoscopic Liver Resection: a web-based study on the global diffusion of laparoscopic liver surgery prior to the 2nd International Consensus Conference on Laparoscopic Liver Resection in Iwate, Japan. J Hepatobiliary Pancreat Sci. 2014;21:737-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 28. | Zhou YM, Shao WY, Zhao YF, Xu DH, Li B. Meta-analysis of laparoscopic versus open resection for hepatocellular carcinoma. Dig Dis Sci. 2011;56:1937-1943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 29. | Li N, Wu YR, Wu B, Lu MQ. Surgical and oncologic outcomes following laparoscopic versus open liver resection for hepatocellular carcinoma: A meta-analysis. Hepatol Res. 2012;42:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 30. | Xiong JJ, Altaf K, Javed MA, Huang W, Mukherjee R, Mai G, Sutton R, Liu XB, Hu WM. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol. 2012;18:6657-6668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 112] [Cited by in RCA: 132] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 31. | Memeo R, de’Angelis N, Compagnon P, Salloum C, Cherqui D, Laurent A, Azoulay D. Laparoscopic vs. open liver resection for hepatocellular carcinoma of cirrhotic liver: a case-control study. World J Surg. 2014;38:2919-2926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 32. | Kim H, Suh KS, Lee KW, Yi NJ, Hong G, Suh SW, Yoo T, Park MS, Choi Y, Lee HW. Long-term outcome of laparoscopic versus open liver resection for hepatocellular carcinoma: a case-controlled study with propensity score matching. Surg Endosc. 2014;28:950-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 33. | Kanazawa A, Tsukamoto T, Shimizu S, Kodai S, Yamazoe S, Yamamoto S, Kubo S. Impact of laparoscopic liver resection for hepatocellular carcinoma with F4-liver cirrhosis. Surg Endosc. 2013;27:2592-2597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 34. | Cheung TT, Poon RT, Yuen WK, Chok KS, Jenkins CR, Chan SC, Fan ST, Lo CM. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg. 2013;257:506-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 35. | Ai JH, Li JW, Chen J, Bie P, Wang SG, Zheng SG. Feasibility and safety of laparoscopic liver resection for hepatocellular carcinoma with a tumor size of 5-10 cm. PLoS One. 2013;8:e72328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 36. | Truant S, Bouras AF, Hebbar M, Boleslawski E, Fromont G, Dharancy S, Leteurtre E, Zerbib P, Pruvot FR. Laparoscopic resection vs. open liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: a case-matched study. Surg Endosc. 2011;25:3668-3677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 37. | Lee KF, Chong CN, Wong J, Cheung YS, Wong J, Lai P. Long-term results of laparoscopic hepatectomy versus open hepatectomy for hepatocellular carcinoma: a case-matched analysis. World J Surg. 2011;35:2268-2274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 38. | Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011;146:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 293] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 39. | Hu BS, Chen K, Tan HM, Ding XM, Tan JW. Comparison of laparoscopic vs open liver lobectomy (segmentectomy) for hepatocellular carcinoma. World J Gastroenterol. 2011;17:4725-4728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 40. | Kim HH, Park EK, Seoung JS, Hur YH, Koh YS, Kim JC, Cho CK, Kim HJ. Liver resection for hepatocellular carcinoma: case-matched analysis of laparoscopic versus open resection. J Korean Surg Soc. 2011;80:412-419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 41. | Ker CG, Chen JS, Kuo KK, Chuang SC, Wang SJ, Chang WC, Lee KT, Chen HY, Juan CC. Liver Surgery for Hepatocellular Carcinoma: Laparoscopic versus Open Approach. Int J Hepatol. 2011;2011:596792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 42. | Alemi F, Kwon E, Freise C, Kang SM, Hirose R, Stewart L, Corvera CU. Hepatic surgery at a VA tertiary medical center: lessons learned. Am J Surg. 2010;200:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 43. | Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, Ferla G. Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol. 2010;102:82-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 44. | Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D, Dagher I. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24:1170-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 187] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 45. | Belli G, Limongelli P, Fantini C, D’Agostino A, Cioffi L, Belli A, Russo G. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg. 2009;96:1041-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 166] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 46. | Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM. Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol. 2009;16:1572-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 47. | Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009;144:143-147; discussion 148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 48. | Endo Y, Ohta M, Sasaki A, Kai S, Eguchi H, Iwaki K, Shibata K, Kitano S. A comparative study of the long-term outcomes after laparoscopy-assisted and open left lateral hepatectomy for hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech. 2009;19:e171-e174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 49. | Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Maeda T, Shiba T. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg. 2005;189:190-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 50. | Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003;138:763-769; discussion 769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 219] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 51. | Shimada M, Hashizume M, Maehara S, Tsujita E, Rikimaru T, Yamashita Y, Tanaka S, Adachi E, Sugimachi K. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc. 2001;15:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 145] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 52. | Lee KF, Cheung YS, Chong CN, Tsang YY, Ng WW, Ling E, Wong J, Lai PB. Laparoscopic versus open hepatectomy for liver tumours: a case control study. Hong Kong Med J. 2007;13:442-448. [PubMed] |
| 53. | Belli G, Fantini C, D’Agostino A, Cioffi L, Langella S, Russolillo N, Belli A. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc. 2007;21:2004-2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 186] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 54. | Morise Z, Sugioka A, Kawabe N, Umemoto S, Nagata H, Ohshima H, Kawase J, Arakawa S, Yoshida R. Pure laparoscopic hepatectomy for hepatocellular carcinoma patients with severe liver cirrhosis. Asian J Endosc Surg. 2011;4:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 55. | Soubrane O, Goumard C, Laurent A, Tranchart H, Truant S, Gayet B, Salloum C, Luc G, Dokmak S, Piardi T. Laparoscopic resection of hepatocellular carcinoma: a French survey in 351 patients. HPB (Oxford). 2014;16:357-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 88] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 56. | Laurent A, Tayar C, Andréoletti M, Lauzet JY, Merle JC, Cherqui D. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2009;16:310-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 114] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 57. | Kanazawa A, Tsukamoto T, Shimizu S, Kodai S, Yamamoto S, Yamazoe S, Ohira G, Nakajima T. Laparoscopic liver resection for treating recurrent hepatocellular carcinoma. J Hepatobiliary Pancreat Sci. 2013;20:512-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 58. | Belli G, Cioffi L, Fantini C, D’Agostino A, Russo G, Limongelli P, Belli A. Laparoscopic redo surgery for recurrent hepatocellular carcinoma in cirrhotic patients: feasibility, safety, and results. Surg Endosc. 2009;23:1807-1811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 59. | Tomishige H, Morise Z, Kawabe N, Nagata H, Ohshima H, Kawase J, Arakawa S, Yoshida R, Isetani M. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J Gastrointest Surg. 2013;5:173-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 60. | Soubrane O, Schwarz L, Cauchy F, Cauchy F, Perotto LO, Brustia R, Bernard D, Scatton O. A Conceptual Technique for Laparoscopic Right Hepatectomy Based on Facts and Oncologic Principles: The Caudal Approach. Ann Surg. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 118] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 61. | Wakabayashi G, Cherqui D, Geller DA, Han HS, Kaneko H, Buell JF. Laparoscopic hepatectomy is theoretically better than open hepatectomy: preparing for the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci. 2014;21:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 108] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 62. | Yu LH, Li N, Cheng SQ. The Role of Antiviral Therapy for HBV-Related Hepatocellular Carcinoma. Int J Hepatol. 2011;2011:416459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |