Published online Jun 27, 2015. doi: 10.4240/wjgs.v7.i6.94
Peer-review started: August 30, 2014
First decision: November 27, 2014
Revised: December 29, 2014
Accepted: May 5, 2015
Article in press: May 6, 2015
Published online: June 27, 2015
Total colectomy with ileostomy placement is a treatment for patients with inflammatory bowel disease or familial adenomatous polyposis (FAP). A rare and late complication of this treatment is carcinoma arising at the ileostomy site. We describe two such cases: a 78-year-old male 30 years after subtotal colectomy and ileostomy for FAP, and an 85-year-old male 50 years after colectomy and ileostomy for ulcerative colitis. The long latency period between creation of the ileostomies and development of carcinoma suggests a chronic metaplasia due to an irritating/inflammatory causative factor. Surgical excision of the mass and relocation of the stoma is the mainstay of therapy, with possible benefits from adjuvant chemotherapy. Newly developed lesions at stoma sites should be biopsied to rule out the possibility of this rare ileostomy complication.
Core tip: A rare and late complication of ileostomy creation is carcinoma arising from the ileostomy site. Physicians and patients should be aware of this phenomenon and require regular physical exams. Any and all parastomal lesions should be biopsied to rule out adenocarcinoma at the ileostomy site.
- Citation: Procaccino L, Rehman S, Abdurakhmanov A, McWhorter P, La Gamma N, Bhaskaran MC, Maurer J, Grimaldi GM, Rilo H, Nicastro J, Coppa G, Molmenti EP, Procaccino J. Adenocarcinoma arising at ileostomy sites: Two cases and a review of the literature. World J Gastrointest Surg 2015; 7(6): 94-97
- URL: https://www.wjgnet.com/1948-9366/full/v7/i6/94.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i6.94
Total colectomy with ileostomy is the definitive treatment for patients with ulcerative colitis and familial adenomatous polyposis (FAP). Although rare, a late complication of this treatment is carcinoma at the ileostomy. We report two cases of ileostomy carcinoma and review the literature regarding this rare phenomenon.
There has been much speculation regarding the etiology of such cancers. The prevailing theory suggests that chronic inflammation and cell proliferation at the convergence of mucosa and skin are the likely causative factors[1].
This patient is a 78-year-old male with a history of FAP treated with subtotal colectomy in 1969 and ileostomy in 1984, who presented with a mass at his ileostomy site. He denied having abdominal pain, cramps, or weight loss. His medical history was also relevant for anemia, atrial flutter, essential hypertension, gastroesophageal reflux, gout, hyperlipidemia, myocardial infarction, non-insulin-requiring diabetes mellitus, a perforated gastroduodenal ulcer requiring open repair, and renal calculi. His surgical history includes extracorporeal shockwave lithotripsy for renal calculi, bilateral cataract extraction, trans-urethral excision of bladder stones, prostate vaporization, open cholecystectomy, appendectomy, and tonsillectomy.
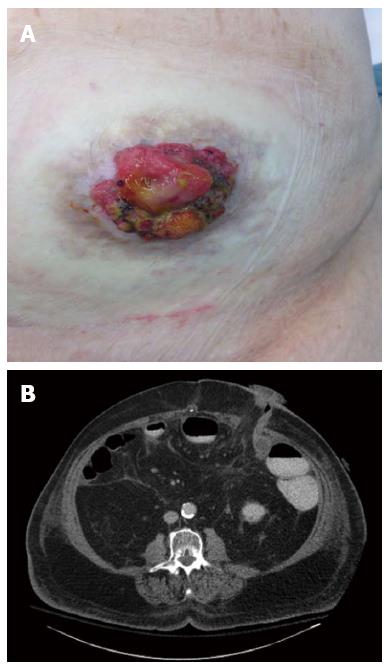
On physical exam, a fungating tumor could be detected involving the mucosa of the ileostomy (Figure 1). Ileoscopy revealed multiple polyps up to 30 cm from the ileostomy site.
Biopsy of the lesion showed adenocarcinoma. A work-up for metastatic disease was performed, including a chest X-ray and computed tomography (CT) scans. Laboratory tests, including a carcinoembryonic antigen level, were all within normal range.
The patient underwent a laparotomy, resection of the terminal ileum, ileostomy, and abdominal wall skin, and creation of a new ileostomy. Pathological evaluation showed invasive intestinal type, moderately differentiated adenocarcinoma of the small bowel arising at the ileostomy site with a background of high-grade dysplasia and intramucosal carcinoma in tubular adenoma. Multiple (at least 50) tubular adenomas were present throughout the length of the specimen. All resection margins were negative for invasive tumor. No adjuvant therapy was recommended. He is currently alive and well one month post-operatively.
This patient is an 85-year-old male who had a colectomy and ileostomy created 50 years ago for ulcerative colitis, who presented with lethargy, dehydration, a small bowel obstruction, and a parastomal mass. He had been diagnosed with Crohn’s disease three years ago when he had bleeding from the ileostomy. Since that time, he has had significant weight loss, anorexia, and numerous hospitalizations for dehydration. His medical and surgical history is also significant for atrial fibrillation, sick sinus syndrome requiring a permanent pacemaker, and benign prostatic hypertrophy.
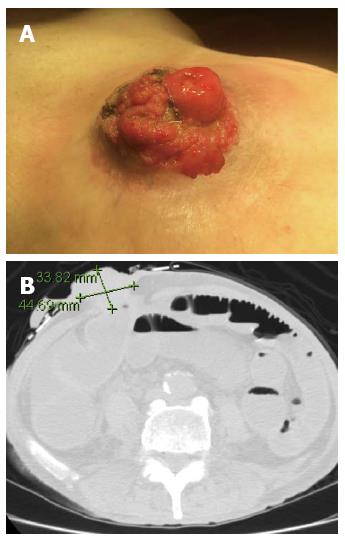
Physical exam revealed an ulcerated mass at the ostomy site (Figure 2). Biopsy of the parastomal mass revealed a well-differentiated adenocarcinoma with ulceration involving the stoma. A CT scan of the abdomen/pelvis showed diffuse dilation of small bowel loops with air-fluid levels to the level of the mass, consistent with small bowel obstruction. Ileoscopy showed large amounts of friable tissue compressing the ileostomy opening.
The patient underwent resection of the ileostomy and surrounding abdominal wall, followed by creation of a new ileostomy and abdominal wall reconstruction with Strattice mesh. Although he recovered from the surgical intervention, this patient succumbed one month later as a result of urosepsis.
The first case of carcinoma arising from an ileostomy site was reported in 1969 in a patient who was treated for ulcerative colitis[2]. The first report associated with FAP was in 1982[3]. There have been 40 adenocarcinomas and 4 squamous cell carcinomas reported as of 2005[1]. This increase in incidence can be attributed to the latency period between creation of ileostomies and the development of carcinoma (estimated to average 30 years) and the introduction of the eversion ileostomy in 1952[4].
Adenocarcinomas at the mucocutaneous junction of an ileostomy were reported in four patients in 1988[5]. All four patients developed cancer approximately 30 years after stoma creation. Another primary mucinous adenocarcinoma was reported at that time in a 60-year-old woman 28 years after subtotal colectomy and ileostomy creation[6]. Histopathology revealed a tubulovillous adenoma origin. The same authors also reviewed five cases of primary adenocarcinomas arising at ileostomy sites. While three of the patients were described as having fungating, exophytic, polypoid growths (similar to our cases), the other two patients presented with skin induration and irritation, providing more of a diagnostic challenge.
A review of 36 primary adenocarcinomas at ileostomy sites by Metzger et al[7] affirmed the mechanism to be likely associated with colonic metaplasia from chronic inflammation. The authors found lymph node involvement in 19% of cases, and an 85% survival rate. This study showed an average of 27 years between placement of ileostomy and development of a parastomal lesion, and emphasized the importance of patient education in early detection. Our two cases presented 30 and 50 years post ileostomy placement. Surgical excision and relocation of the stoma is the mainstay of therapy, with possible benefits from adjuvant therapy.
Another report described a 37-year-old man misdiagnosed with a pyogenic granuloma at an ostomy site after presenting with an asymptomatic polypoid lesion 18 years after subtotal colectomy for ulcerative colitis[8]. Only after failed treatment with topical silver nitrate was a biopsy taken, which revealed a primary adenocarcinoma. Although peristomal dermatoses such as contact dermatitis, psoriasis, and pyoderma gangrenosum are far more common than carcinoma at an ileostomy site, a high index of suspicion is warranted for any parastomal lesion. Dermatologists or primary care physicians who often follow up with these patients are urged to be aware of this rare complication of ileostomies.
Other investigators found a total of 14 patients with FAP[9] and metaplasia of pre-existing adenomas discovered on pathology, suggesting still a different mechanism from the previously mentioned chronic irritation and inflammation of the mucosa and skin junction. The median interval between ileostomy creation and adenocarcinoma was 25 years in this small sample. None of the patients had lymph node involvement, while two had local recurrence. The difference in proposed mechanisms of ileostomy adenocarcinomas is attributed to the initial reason for colectomy. If due to FAP, the theory is a pre-existing adenoma that undergoes metaplasia. In ulcerative colitis or Crohn’s, chronic inflammation is regarded to be the metaplasia culprit.
Patient and physician education and regular physician physical exams are of paramount importance in early detection. Newly developed lesions at stomas should be biopsied to rule out this rare ileostomy complication.
The main symptoms were a fungating mass at the ileostomy site, additionally accompanied by lethargy, dehydration, and a small bowel obstruction in one case.
The main clinical findings were a parastomal mass.
Common differential diagnoses for parastomal lesions include contact dermatitis, psoriasis, and pyoderma gangrenosum due to the constant contact of surrounding skin with feces. This chronic irritation more commonly causes a dermatological condition rather than a malignancy.
Biopsy of the mass is absolutely essential to distinguish it from the previously mentioned more common differentials, and found adenocarcinoma.
Computed tomography scan was used to visualize the extent of the mass.
Pathological examination of the biopsies found well-differentiated adenocarcinoma.
Treatment consists of surgical excision and relocation of the stoma.
A rare and late complication of ileostomy creation is carcinoma arising from the ileostomy site and physicians and patients should be aware of this phenomenon and require regular physical exams.
The strengths of this article include it’s simple core tip and lesson, and it’s well written form and language.
P- Reviewer: Fusaiu G, Seow-Choen F S- Editor: Tian YL L- Editor: A E- Editor: Zhang DN
| 1. | Quah HM, Samad A, Maw A. Ileostomy carcinomas a review: the latent risk after colectomy for ulcerative colitis and familial adenomatous polyposis. Colorectal Dis. 2005;7:538-544. |
| 2. | Sigler L, Jedd FL. Adenocarcinoma of the ileostomy occurring after colectomy for ulcerative colitis: report of a case. Dis Colon Rectum. 1969;12:45-48. |
| 3. | Roth JA, Logio T. Carcinoma arising in an ileostomy stoma: an unusual complication of adenomatous polyposis coli. Cancer. 1982;49:2180-2184. |
| 5. | Suarez V, Alexander-Williams J, O’Connor HJ, Campos A, Fuggle WJ, Thompson H, Enker WE, Greenstein AJ. Carcinoma developing in ileostomies after 25 or more years. Gastroenterology. 1988;95:205-208. |
| 6. | Smart PJ, Sastry S, Wells S. Primary mucinous adenocarcinoma developing in an ileostomy stoma. Gut. 1988;29:1607-1612. |
| 7. | Metzger PP, Slappy AL, Chua HK, Menke DM. Adenocarcinoma developing at an ileostomy: report of a case and review of the literature. Dis Colon Rectum. 2008;51:604-609. |
| 8. | Al-Niaimi F, Lyon CC. Primary adenocarcinoma in peristomal skin: a case study. Ostomy Wound Manage. 2010;56:45-47. |
| 9. | Hammad A, Tayyem R, Milewski PJ, Gunasekaran S. Primary adenocarcinoma in the ileostomy of a woman with familial adenomatous polyposis: a case report and literature review. J Med Case Rep. 2011;5:556. |