Published online Dec 27, 2015. doi: 10.4240/wjgs.v7.i12.398
Peer-review started: July 3, 2015
First decision: August 4, 2015
Revised: August 25, 2015
Accepted: October 23, 2015
Article in press: October 27, 2015
Published online: December 27, 2015
Processing time: 177 Days and 22.1 Hours
Accessory gallbladder is a rare congenital anomaly occurring in 1 in 4000 births, that is not associated with any specific symptoms. Usually this cannot be diagnosed on ultrasonography and hence they are usually not diagnosed preoperatively. Removal of the accessory gallbladder is necessary to avoid recurrence of symptoms. H-type accessory gallbladder is a rare anomaly. Once identified intra-operatively during laparoscopic cholecystectomy, the surgery is usually converted to open. By using the main gallbladder for liver traction and doing a dome down technique for the accessory gallbladder, we were able to perform the double cholecystectomy with intra-operative cholangiogram laparoscopically. Laparoscopic cholecystectomy was performed in 27-year-old male for biliary colic. Prior imaging with computer tomography-scan and ultrasound did not show a duplicated gallbladder. Intraoperatively after ligation of cystic artery and duct an additional structure was seen on its medial aspect. Intraoperative cholangiogram confirmed the patency of intra-hepatic and extra-hepatic biliary ducts. Subsequent dissection around this structure revealed a second gallbladder with cystic duct (H-type). Pathological analysis confirmed the presence of two gallbladders with features of chronic cholecystitis. It is important to use cholangiogram to identify structural anomalies and avoid complications.
Core tip: Accessory gallbladders are a rare anatomic anomaly, that classically goes unnoticed. These are often not diagnosed preoperatively in patients undergoing cholecystectomy. We present a 27-year-old male scheduled for gallbladder removal for biliary colic. Intraoperatively, following ligation of cystic artery and duct, an additional structure was noted, and intraoperative cholangiogram confirmed a second gallbladder with an associated accessory cystic duct. Pathological analysis confirmed the presence of two gallbladders with features of chronic cholecystitis. Recognizing and understanding the presentation of accessory gallbladders can prevent the pitfalls of surgery with anatomical abnormalities, as well as offering the appropriate management.
- Citation: Cozacov Y, Subhas G, Jacobs M, Parikh J. Total laparoscopic removal of accessory gallbladder: A case report and review of literature. World J Gastrointest Surg 2015; 7(12): 398-402
- URL: https://www.wjgnet.com/1948-9366/full/v7/i12/398.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v7.i12.398
Multiple gallbladders are a rare congenital biliary variance occurring in 1 per 3800-5000 people[1]. We present a case of an accessory gallbladder not discovered by preoperative ultrasound or computer tomography (CT) imaging. The accessory gallbladder was discovered intraoperatively and a total laparoscopic cholecystectomy of both the main and accessory gallbladder was performed. We used the main gallbladder for liver retraction and did a dome down technique for accessory gallbladder dissection. To date, 20 cases of duplicated gallbladder removal by laparoscopic means[2-4]. We present a successful case of laparoscopic removal of H-type accessory gallbladder, as well as a review of literature.
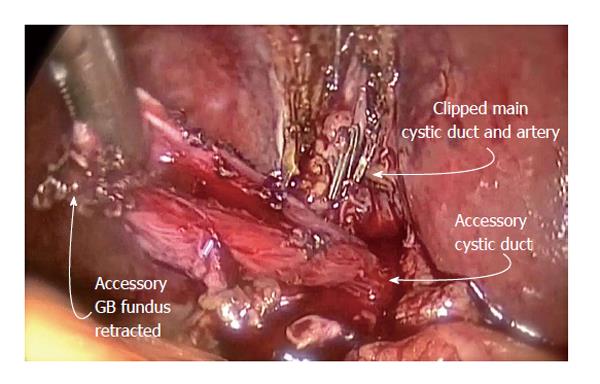
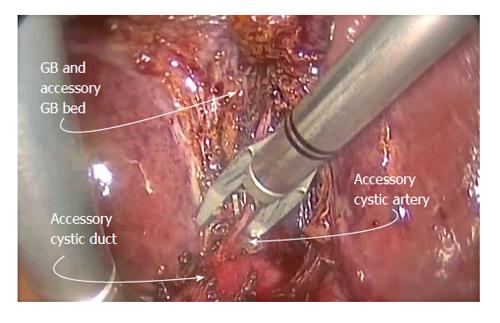
A 27-year-old male was worked up for biliary colic. Ultrasound of the abdomen and CT of the abdomen revealed cholelithiasis (multiple subcentimeter stones), and they did not show any structural abnormalities. Liver enzymes were within normal range. The patient was scheduled for an elective laparoscopic cholecystectomy. Intra-operatively cystic artery and duct of the main gallbladder were ligated and divided after obtaining a critical view. During dissection of the gallbladder from the liver bed, an additional structure was seen on its medial aspect (Figure 1). At this time, the main gallbladder was still bound to the liver edge at the fundus, allowing the use of the gallbladder to retract the liver. Subsequent dissection revealed an accessory gallbladder, with an accessory cystic duct and accessory cystic artery (Figure 2). The accessory gallbladder was then dissected with a dome down technique, from the gallbladder fundus towards the neck, and the accessory cystic duct and artery were identified. An intraoperative cholangiogram was performed through the accessory cystic duct to delineate the anatomy. No stones or filling defects were identified, the intra-hepatic and extra-hepatic biliary ducts were patent, and contrast confirmed the accessory cystic duct draining into the common bile duct, with contrast then entering the duodenum. Chromic endoloop were tied around the accessory cystic duct and transected. The main gallbladder was then dissected from the liver bed. The whole procedure was completed laparoscopically without any additional ports. The patient was discharged home on post-operative day one. Pathology confirmed a main gallbladder measuring 8 cm × 3 cm showing cholelithiasis with chronic cholecystitis and an accessory gallbladder 1.5 cm × 1.5 cm in dimensions with mild chronic cholecystitis. This accessory gallbladder was of the H-type, or ductular type, per the Harlaftis classification.
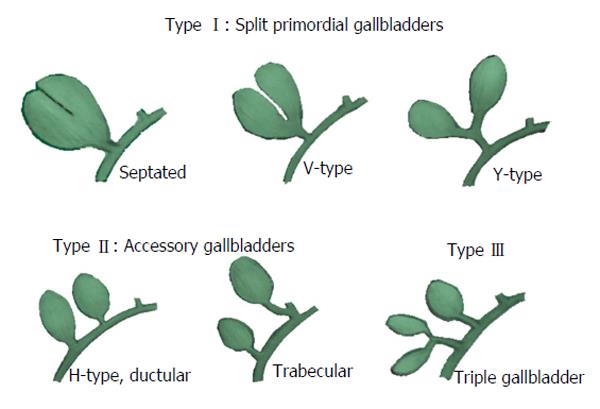
True incidence of duplicated gallbladders is difficult to calculate, as the gallbladder anomalies are often asymptomatic and goes undiscovered. Incidence is deduced from cadaveric studies[5]. The first report of an accessory gallbladder was in 1674 during an autopsy by Blasius. It was not until 1911 that Sherren first documented a case of double accessory gallbladder in a living human[5,6]. This anatomic anomaly occurs during the third and fourth week of embryological development. The anatomical variations of accessory gallbladders have been classified by several authors, with Harlaftis’s classification being widely used in the literature. Harlaftis classifies gallbladder anomalies into 3 types (Figure 3).
Type 1, or the split primordial group, has only one cystic duct draining into the common bile duct[7]. Sub classification of type 1 includes a septated, V-shaped, or Y-shaped duplicated gallbladder. The septated subtype grossly presents as a single gallbladder with an indentation at the fundus and has only one cystic duct. This morphology likely represents an incomplete resolution of the solid stage of the development of the gallbladder[7]. The V-shaped subtype of duplicated gallbladder refers to gallbladders that are joined at the neck level, draining into a single cystic duct as well. The Y-shaped subtype duplicated gallbladder, has a separated cystic duct that joins together with the main cystic duct to become a shared, single “common” cystic duct that later joins the common bile duct[1,6,8]. This morphology likely represents an out-pocketing of the cystic duct which subsequently develops into a definitive second gallbladder. These gallbladders are usually close in proximity, commonly sharing a single gallbladder bed.
Type 2, or the accessory gallbladder group, has more than one cystic duct draining into the biliary tree. Here, each subtype consists of a main gallbladder with a main cystic duct and an accessory gallbladder with an accessory cystic duct. The main and accessory cystic ducts drain independently into the biliary tree. Sub classification of type 2 accessory gallbladders includes H or Ductular type and trabecular type. In H or ductular type the accessory cystic duct connects to the common bile duct. In the trabecular type the accessory cystic duct connects to the left or right hepatic duct. Our case represents the H or ductular type accessory gallbladder with the accessory cystic duct inserting into the common bile duct distal to the main cystic duct. A review of 148 cases of accessory gallbladders found that H-type accessory gallbladder was the most common variant accounting for nearly half of the reports[8]. Van Steenbergen et al[9] reported a trabecular type accessory gallbladder identified preoperatively with an endoscopic retrograde cholangiopancreatogram, which showed the accessory gallbladder to be intrahepatic. Cholangiography showed the accessory cystic duct draining into the intrahepatic right hepatic duct. Postoperative pathology report noted both gallbladder walls to be fused together[9]. Anomalies of type 2 have been reported by several authors, including a laparoscopic cholecystectomy converted to open of an accessory gallbladder draining into the left hepatic duct[2], an accessory gallbladder arising from the left hepatic duct, which was found on pathology to harbor adenocarcinoma[8]. There are two more reports of carcinoma found in the accessory gallbladder[10,11].
Type 3 accessory gallbladders include gallbladders with anatomical anomalies that do not fit either type 1 nor type 2. These are rare examples of triple gallbladders and other anomalies. Triple gallbladders are rare in humans and were mainly deduced from feline dissections. Roeder et al[12] described triplication of the gallbladder with two of the gallbladders surgically removed, one showing acute cholecystitis and cholelithiasis and the second containing papillary adenocarcinoma. The third gallbladder was demonstrated by T tube cholangiogram but not identified during the operation and was assumed to be intrahepatic[12]. Schroeder et al[13] described a triple gallbladder in a 38-year-old male, of which two were identified preoperatively, and the third (or second accessory GB) was found intraoperatively. All final histopathology report noted cholelithiasis and chronic inflammation. The entire case was performed laparoscopically[13].
Accessory gallbladder may be missed on routine preoperative imaging[2,3,14]. Ultrasound and computerized tomography do not provide sufficient visualization of biliary anatomy to reliably detect double accessory gallbladders[14,15]. Oral cholecystography has been studied and results showed this imaging modality misses 30%-66% of double gallbladders[15-17]. Hence, it is important to thoroughly investigate biliary anatomy intraoperatively to identify an accessory gallbladder, noting that these may vary in position. The H-type accessory gallbladder has been reported in the literature as intrahepatic, subhepatic, within the gastrohepatic ligament, and adjacent to the primary gallbladder as seen in this case report[16,18].
When an accessory gallbladder is found intraoperatively both gallbladders should be removed to avoid complications[3,5,14,16,19]. If the accessory gallbladder is not removed, patients can return with biliary symptoms[2,14,20,21]. Reinisch et al[22] revisited a 73-year-old patient 17 years following laparoscopic cholecystectomy due to acute cholecystitis of the accessory gallbladder, not detected during the index operation[22]. The accessory gallbladder is prone to the same pathology as the primary gallbladder including cholecystitis, empyema, cholecystocolic fistula, torsion, papilloma, and carcinoma[3,5,11,12,16,23-25]. Before removing the accessory gallbladder, intraoperative imaging is imperative to outline the biliary anatomy and avoid injury to the biliary tree[16]. The superior imaging test is an intraoperative cholangiography[3,14,26-28]. Studies have shown that intraoperative cholangiography reduces the degree of bile duct injury by approximately thirty percent during cholecystectomy, and we believe this would apply in cases of accessory gallbladders as well, although this has not been documented for these cases specifically[14,21].
It is important to note that the complications and pathology of multiple gallbladders relies on many anecdotal publications. There is not yet a standardized approach when such case is encountered, though there is an agreement among authors that removal of the accessory gallbladder should be attempted, cholangiography is warranted, careful dissection with recognition of the accessory cystic artery and duct aids in recognizing the accessory gallbladder, and the laparoscopic approach, if possible, is an appropriate method of removal of the accessory gallbladder. Final diagnosis is completed with histopathological evaluation, to differentiate from other biliary lesions.
Multiple gallbladders are a rare congenital abnormality that may be missed on routine imaging. Intraoperative identification and subsequent removal of the accessory gallbladder is necessary to avoid recurrent biliary symptoms. Total laparoscopic removal can be performed safely. By using the main gallbladder for liver retraction, the accessory gallbladder can be dissected using dome down technique. Intraoperative cholangiogram should be performed to define biliary anatomy. There is no evidence at this time to remove an incidental accessory gallbladder, and we recommend removal only in association with main gallbladder disease destined for cholecystectomy.
Patient had right upper quadrant discomfort for several months, associated with fatty indigestion.
Patient was suspected to have biliary colic.
On the authors’ differential diagnosis were biliary colic due to cholelithiasis, sphincter of oddi dysfunction, chronic/subacute cholecystitis.
Patient’s basic metabolic and liver function panels were all within normal limits.
Ultrasound and computer tomography scan were only positive for wall thickening and cholelithiasis, otherwise negative.
Pathology confirmed a main gallbladder measuring 8 cm × 3 cm showing cholelithiasis with chronic cholecystitis and an accessory gallbladder 1.5 cm × 1.5 cm in dimensions with mild chronic cholecystits.
Patient was scheduled for elective cholecystectomy.
None of the report describes the technique for a total laparoscopic approach for double gallbladder.
ERCP: Endoscopic retrograde cholangiopancreatogram.
Biliary anatomy has great diversity, and as surgeons, it is better to make themselves familiar with this great variability, for the authors’ to be better and safer surgeons.
The authors described interesting case of laparoscopic cholecystectomy for accessory gallbladder. It is important to know the anomalies of biliary tract including accessory gallbladder in order to avoid injury of the biliary tree during cholecystectomy.
P- Reviewer: Cecka F, Nagem RG, Srinath AI S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Boyden EA. The accessory gallbladder- an embryological and comparative study of aberrant biliary vesicles occurring in man and the domestic mammals. Am J Anat. 1926;38:177-231. [RCA] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 194] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Gorecki PJ, Andrei VE, Musacchio T, Schein M. Double gallbladder originating from left hepatic duct: a case report and review of literature. JSLS. 1998;2:337-339. [PubMed] |
| 3. | Cueto García J, Weber A, Serrano Berry F, Tanur Tatz B. Double gallbladder treated successfully by laparoscopy. J Laparoendosc Surg. 1993;3:153-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Miyajima N, Yamakawa T, Varma A, Uno K, Ohtaki S, Kano N. Experience with laparoscopic double gallbladder removal. Surg Endosc. 1995;9:63-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Paraskevas GK, Raikos A, Ioannidis O, Papaziogas B. Duplicated gallbladder: surgical application and review of the literature. Ital J Anat Embryol. 2011;116:61-66. [PubMed] |
| 6. | Sherren J. IX. A Double Gall-bladder Removed by Operation. Ann Surg. 1911;54:204-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Ingegno AP, D’albora JB. Double gallbladder; roentgenographic demonstration of a case of the Y type; classification of accessory gallbladder. Am J Roentgenol Radium Ther. 1949;61:671-676. [PubMed] |
| 8. | Kawanishi M, Kuwada Y, Mitsuoka Y, Sasao S, Mouri T, Takesaki E, Takahashi T, Toyota K, Nakatani T. A case of double gallbladder with adenocarcinoma arising from the left hepatic duct: a case report and review of the literature. Gastroenterol Res Pract. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Van Steenbergen W, Krekelbergh F, Ectors N, Ponette E, Yap SH. Double gallbladder documented by endoscopic retrograde cholangiography. J Belge Radiol. 1993;76:243-244. [PubMed] |
| 10. | Kin Y, Yamaguchi A, Isogai M, Hori A. Duplication of the gallbladder with advanced adenocarcinoma: diagnostic value of MRI and angiography. Hepatogastroenterology. 1996;43:405-408. [PubMed] |
| 11. | Raymond SW, Thrift CB. Carcinoma of a duplicated gall bladder. Ill Med J. 1956;110:239-240. [PubMed] |
| 12. | Roeder WJ, Mersheimer WL, Kazarian KK. Triplication of the gallbladder with cholecystitis, cholelithiasis, and papillary adenocarcinoma. Am J Surg. 1971;121:746-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Schroeder C, Draper KR. Laparoscopic cholecystectomy for triple gallbladder. Surg Endosc. 2003;17:1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Fazio V, Damiano G, Palumbo VD, Spinelli G, Scio A, Tomasello G, Marrazzo A, Buscemi S, Lo Monte AI. An unexpected surprise at the end of a “quiet” cholecystectomy. A case report and review of the literature. Ann Ital Chir. 2012;83:265-267. [PubMed] |
| 15. | Yorganci K, Kabay B, Aran O. Laparoscopic double cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2001;11:126-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 16. | Gigot J, Van Beers B, Goncette L, Etienne J, Collard A, Jadoul P, Therasse A, Otte JB, Kestens P. Laparoscopic treatment of gallbladder duplication. A plea for removal of both gallbladders. Surg Endosc. 1997;11:479-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Harlaftis N, Gray SW, Skandalakis JE. Multiple gallbladders. Surg Gynecol Obstet. 1977;145:928-934. [PubMed] |
| 18. | Gross RE. Congenital anomalies of the gallbladder: a review of one hundred and forty-eight cases, with a report of a double gallbladder. Arch Surg. 1936;32:131. [RCA] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 258] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Shapiro T, Rennie W. Duplicate gallbladder cholecystitis after open cholecystectomy. Ann Emerg Med. 1999;33:584-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Heinerman M, Lexer G, Sungler P, Mayer F, Boeckl O. Endoscopic retrograde cholangiographic demonstration of a double gallbladder following laparoscopic cholecystectomy. Surg Endosc. 1995;9:61-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Silvis R, van Wieringen AJ, van der Werken CH. Reoperation for a symptomatic double gallbladder. Surg Endosc. 1996;10:336-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Reinisch A, Brandt L, Fuchs K-H. Doppelt angelegte Gallenblase – Laparoskopische Cholezystektomie 17 Jahre nach konventioneller Cholezystektomie. Zentralblatt Für Chir. 2009;134:576-579. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Cunningham JJ. Empyema of a duplicated gallbladder: echographic findings. J Clin Ultrasound. 1980;8:511-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Recht W. Torsion of a double gallbladder; a report of a case and a review of the literature. Br J Surg. 1952;39:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Ritchie AW, Crucioli V. Double gallbladder with cholecystocolic fistula: a case report. Br J Surg. 1980;67:145-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Hobbs MS, Mai Q, Knuiman MW, Fletcher DR, Ridout SC. Surgeon experience and trends in intraoperative complications in laparoscopic cholecystectomy. Br J Surg. 2006;93:844-853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 27. | Davidoff AM, Pappas TN, Murray EA, Hilleren DJ, Johnson RD, Baker ME, Newman GE, Cotton PB, Meyers WC. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 335] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 28. | Flowers JL, Zucker KA, Graham SM, Scovill WA, Imbembo AL, Bailey RW. Laparoscopic cholangiography. Results and indications. Ann Surg. 1992;215:209-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 126] [Article Influence: 3.8] [Reference Citation Analysis (0)] |