Published online Aug 27, 2014. doi: 10.4240/wjgs.v6.i8.164
Revised: March 27, 2014
Accepted: July 18, 2014
Published online: August 27, 2014
Processing time: 182 Days and 4.2 Hours
We report two cases of solitary mediastinal lymph node recurrence after colon cancer resection. Both cases had para-aortic lymph node metastasis at the time of initial surgery and received adjuvant chemotherapy for 4 years in case 1 and 18 mo in case 2. The time to recurrence was more than 8 years in both cases. After resection of the recurrent tumor, the patient is doing well with no recurrence for 6 years in case 1 and 4 mo in case 2. Patients should be followed up after colon cancer surgery considering the possibility of solitary mediastinal lymph node recurrence if they had para-aortic node metastasis at the time of initial surgery.
Core tip: The first site of recurrence of colon cancer is rarely the mediastinal lymph nodes, and solitary recurrence at this site without another site of recurrence is extremely rare. The operative indication and prognostic significance of the resection of mediastinal lymph node metastasis has not been determined because such recurrence is very rare. Patients should be followed up after colon cancer surgery considering the possibility of solitary mediastinal lymph node recurrence if they had para-aortic node metastasis at the time of initial surgery.
- Citation: Matsuda Y, Yano M, Miyoshi N, Noura S, Ohue M, Sugimura K, Motoori M, Kishi K, Fujiwara Y, Gotoh K, Marubashi S, Akita H, Takahashi H, Sakon M. Solitary mediastinal lymph node recurrence after curative resection of colon cancer. World J Gastrointest Surg 2014; 6(8): 164-168
- URL: https://www.wjgnet.com/1948-9366/full/v6/i8/164.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i8.164
Distant organ recurrence after resection of colon cancer is frequently seen in the liver, lung, bone, and brain[1]. The first site of recurrence is rarely the mediastinal lymph nodes, and solitary recurrence at this site without another site of recurrence is extremely rare[2,3]. With respect to recurrence of colon cancer in the lung and liver, surgical resection is recommended if curative resection of the recurrent tumors is possible. However, the operative indication and prognostic significance of the resection of mediastinal lymph node metastasis has not been determined because such recurrence is very rare. We report two cases of resection for isolated colon cancer metastasis to the mediastinal lymph nodes.
A 65-year-old man visited our hospital for treatment of colon cancer in June 1998. Elevated serum carcinoembryonic antigen (CEA, 17.0 ng/dL; normal range, 0-5 ng/dL) was found at the time of diagnosis. Colonoscopy revealed a type 2 tumor in the sigmoid colon. Computed tomography (CT) showed a T3 tumor in the sigmoid colon with multiple lymph node metastases (cT3N2bM0 cStage IIIc). In September 1998, we performed extended left hemicolectomy (D3 dissection) and para-aortic lymph node dissection. Histological examination revealed moderately differentiated adenocarcinoma invading the muscularis propria without exposure on the serosal surface (n 2b, ly 2, v 1). Metastasis to the para-aortic lymph nodes was also found. After surgery, the patient’s serum CEA level normalized. Adjuvant chemotherapy with tegafur-uracil (100 mg/m2) was given to the patient for 4 years until 2003.
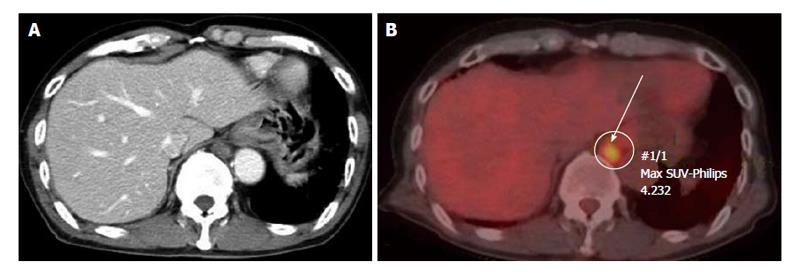
In February 2007, the patient’s tumor markers were normal but CT showed a tumor in the lower mediastinum. The tumor was 16 mm in size and located in the retrocrural space with suspicion of enlarged lymph nodes (Figure 1). CT, magnetic resonance imaging (MRI), and positron emission tomography-CT (PET-CT) did not identify any other primary cancer or any other site of recurrence, such as distant organ or locoregional recurrence. We considered that the tumor was probably a solitary recurrence of the colon cancer and planned a surgical resection because the tumor had enlarged over 3 mo.
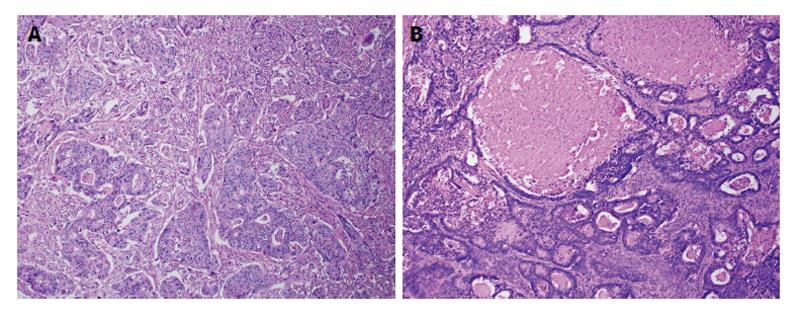
In May 2007, the patient underwent surgical resection of the tumor. We decided against a laparotomy, but performed a left thoracotomy to avoid adhesion due to the previous operation. After thoracotomy, the tumor was identified on the right-anterior surface of the descending aorta. The tumor was easily separated from neighboring organs, such as the aorta or vertebrae, but had extensively invaded the thoracic duct. Therefore, we resected the thoracic duct along with the mediastinal tumor. Histopathology revealed the widespread metastasis of moderately differentiated adenocarcinoma accompanied by necrosis, and it was diagnosed as mediastinal metastases of colon cancer (Figure 2).
The patient was given adjuvant chemotherapy with S-1 (100 mg/m2) and irinotecan (115 mg/m2) for 6 mo. He is doing well with no recurrence for 6 years after the surgery for the recurrent tumor.
In November 2004, a 50-year-old man was admitted to our hospital for treatment of rectal cancer. Colonoscopy revealed a tumor that occupied the entire circumference of the rectum (type 2). Pre-operative CT and MRI showed a T3 tumor in the rectal colon with multiple lymph node metastasis (cT3, N2b, M0 cStage IIIc). In January 2005, we performed para-aortic lymph node and lateral lymph node dissection, in addition to low anterior resection (D3 dissection). Histological examination revealed moderately > poorly differentiated adenocarcinoma invading the muscularis propria without involvement of the serosa (n 2b, ly 0, v 0). Metastasis to para-aortic and lateral lymph nodes was also found. After surgery, the patient’s tumor marker normalized (serum CEA 80.9 ng/dL to 3.5 ng/dL). Three regimens of adjuvant chemotherapy were carried out for 18 mo. The first regimen was irinotecan (100 mg/m2), levofolinate (250 mg/m2), and fluorouracil (500 mg/m2) for 6 mo, the second was S-1 (80 mg/m2) and irinotecan (80 mg/m2) for 4 mo, and the last was S-1 (120 mg/m2) for 8 mo.
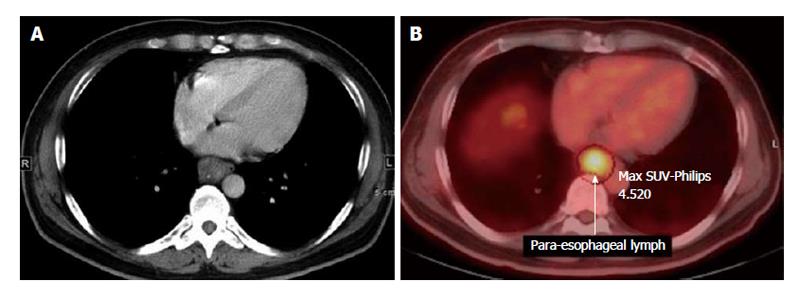
In January 2013, we noted swelling of a para-esophageal lymph node on CT (Figure 3) and elevation of serum CEA (19.0 ng/dL). We performed an endoscopic ultrasound-guided fine-needle aspiration biopsy and diagnosed mediastinal metastasis of rectal cancer. No other site of distant metastasis or local recurrence was found. The patient complained of dysphagia. Therefore, we considered that the tumor was a solitary recurrence of the rectal cancer and decided to perform tumor resection.
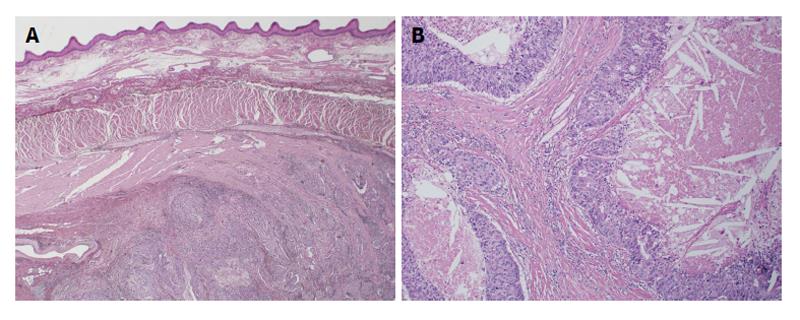
In March 2013, using video-assisted thoracic surgery, we resected the mediastinal tumor, lower esophagus, and thoracic duct, because the tumor located in the posterior mediastinum had widely invaded the right side of the esophagus and thoracic duct, and performed reconstruction with a subtotal gastric tube. Histopathology revealed no neoplastic change in the esophageal mucosal surface, compression from the esophageal adventitia, or infiltration of the muscularis propria (Figure 4). Immunohistochemical analysis showed that the metastatic tumor was positive for cytokeratin (CK) AE1/AE3, CK20 and caudal-type homeobox transcription factor 2 (cdx-2) and negative for CK7, confirming that it was metastasis from rectal cancer.
Adjuvant chemotherapy was not given because the patient did not want it. He is doing well with no recurrence for 4 mo after the surgery for the recurrent tumor.
According to the 2010 guidelines for the treatment of colorectal cancer in Japan, the incidence of first site of recurrence after curative resection of colon cancer is 41.2% in the liver, 27.6% in a lung, 23.1% for local recurrence, and 22.0% for others[4]. Eisenberg et al[1] reviewed 844 cancer-related deaths from colorectal cancer. Among the patients with evidence of recurrent metastatic diseases, the liver was the most common site (50%), followed by lung (25%), bone (10%), and brain (5%). As reported above, lymph node recurrence from colon cancer is relatively rare, especially mediastinal lymph node recurrence. We searched PubMed using keywords (colon cancer, metastasis and solitary mediastinal lymph node). To the best of our knowledge, only two cases have been reported thus far. One was a combined recurrence in an ovary and mediastinal lymph node, and another was solitary mediastinal lymph node recurrence[5,6].
Malignant intra-thoracic tumors, such as lung and esophageal cancers, often metastasize to mediastinal lymph nodes, but malignant extra-thoracic tumors are not likely to metastasize to lymph nodes. Although head and neck cancers and urogenital tumors sometimes metastasize to mediastinal lymph nodes, gastrointestinal cancers do not[7-9]. Libson et al[10] reported 15 cases of mediastinal lymphadenopathy among 1194 cases of gastrointestinal carcinoma. The primary tumor was colonic in nine cases, gastric in four cases, and pancreatic in two cases.
Confirmation of mediastinal lymph node metastasis is more difficult than confirmation of abdominal lymph node metastasis because more non-malignant lymph node enlargement or accumulation is present on PET-CT due to inflammation and granulation in the mediastinum[11]. Mediastinoscopy is often needed for accurate diagnosis[6]. In addition, a primary malignant tumor in the head and neck region or urological region also needs to be ruled out as a differential diagnosis.
The final pathological diagnosis of our two cases was mediastinal lymph node recurrence from colon cancer because both cases exhibited a glandular cavity formation with necrosis and histological similarity to the initial colon cancer. Furthermore, in case 2, the recurrent tumor and primary colonic tumor had the same immunostaining pattern: positive for CKAE1/AE3 CK20 and cdx-2 and negative for CK7.
There are two possible routes for mediastinal lymph node metastasis from the primary colon cancer: retrograde lymph node metastasis and hematogenous metastasis. The former occurs via the thoracic duct from a retroperitoneal lymph node. Thus far, several cases of gastrointestinal cancer have been reported to metastasize to mediastinal nodes via this route[10]. The latter occurs via the paravertebral venous plexus and is often seen in cases in which the patients have distant organ metastases, such as ovarian metastasis[5]. We speculated that, in our cases, the mediastinal lymph node metastasis developed via retrograde lymph node metastasis, as both of the cases had retroperitoneal metastasis at the time of the initial colon cancer surgery and no distant organ metastasis at the time of recurrence.
Interesting findings in our cases are that the time interval from colon cancer surgery to mediastinal lymph node recurrence was very long, more than 8 years. In addition, both of the cases received adjuvant chemotherapy for a relatively long time: 4 years in case 1 and 18 mo in case 2. Adjuvant chemotherapy over a very long time may play a role in delayed recurrence by inducing tumor dormancy or other unknown mechanism.
The prognosis of patients with lymph node recurrence after surgery for colon cancer depends on the number of organs or site of recurrence[4]. Patients with mediastinal lymph node recurrence plus lung metastasis or with multiple lymph node metastases have a poor prognosis[12,13]. Solitary lymph node metastasis without other non-curative factors has generally been reported to be a good indication for surgical treatment[14]. Min et al[15] investigated the outcome of 38 patients (1.3%) who developed isolated para-aortic lymph node recurrence (IPLR) from among 2916 patients who underwent curative surgery for colorectal carcinoma. The median survival time from IPLR was 34 mo, but it was 12 mo for those who did not undergo resection, suggesting the usefulness of surgical resection. Although no report has addressed the surgical indication and prognosis of patients with solitary mediastinal node recurrence, our case report indicates that surgical resection may prolong the survival of patients, considering that case 1 has survived 6 years without repeated recurrence after resection of the recurrent mediastinal node.
In conclusion, we report two very rare cases of solitary mediastinal lymph node recurrence after colon cancer surgery. Patients should be followed up after colon cancer surgery considering the possibility of mediastinal node recurrence if they had para-aortic node metastasis at the time of initial surgery.
A 65-year-old male and a 50-year-old male with a history of resected colon cancer had no symptoms.
Clinical findings were not particular.
Esophagus cancer, metastasis of head and neck cancer or urological cancer, mediastinal tumor.
Tumor markers were normal in case 1 and serum carcinoembryonic antigen elevated 19.0 ng/dL in case 2.
Positron emission tomography/computed tomography scan showed lower mediastinal mass (16 mm) with standardized uptake value (SUV) of 4.232 in case 1 and a para-esophageal lymph node with SUV of 4.520 in case 2.
Histopathology revealed the widespread metastasis of moderately differentiated adenocarcinoma in case 1 and immunohistochemical analysis showed that the metastatic tumor was positive for cytokeratin (CK), AE1/AE3, CK20 and caudal-type homeobox transcription factor 2 and negative for CK7, confirming that it was metastasis from rectal cancer in case 2.
After surgical resection, the patient in case 1 was given adjuvant chemotherapy with S-1 (100 mg/m2) and irinotecan (115 mg/m2) for 6 mo and the patient in case 2 was not given adjuvant chemotherapy.
Mediastinal lymph node recurrence is very rare and only two cases have been reported thus far. One was a combined recurrence in an ovary and mediastinal lymph node, and another was solitary mediastinal lymph node recurrence.
Retrograde lymph node metastasis occurs via the thoracic duct from a retroperitoneal lymph node. Hematogenous metastasis occurs via the paravertebral venous plexus.
Patients should be followed up after colon cancer surgery considering the possibility of solitary mediastinal lymph node recurrence if they had para-aortic node metastasis at the time of initial surgery.
This article highlights a rare entity, metastatic solitary mediastinal lymph node after resection of colon cancer in the form of two cases.
P- Reviewer: Ding MX, Greenspan M S- Editor: Wen LL L- Editor: A E- Editor: Liu SQ
| 1. | Eisenberg B, Decosse JJ, Harford F, Michalek J. Carcinoma of the colon and rectum: the natural history reviewed in 1704 patients. Cancer. 1982;49:1131-1134. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | August DA, Sugarbaker PH, Schneider PD. Lymphatic dissemination of hepatic metastases. Implications for the follow-up and treatment of patients with colorectal cancer. Cancer. 1985;55:1490-1494. [PubMed] |
| 3. | Vetto JT, Cohen AM. Isolated spread of hepatic metastatic disease to a mediastinal lymph node. Report of a case and review of pertinent anatomy and literature. Dis Colon Rectum. 1991;34:1128-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 597] [Article Influence: 42.6] [Reference Citation Analysis (0)] |
| 5. | Kuba H, Sato N, Uchiyama A, Nakafusa Y, Mibu R, Yoshida K, Kuroiwa K, Tanaka M. Mediastinal lymph node metastasis of colon cancer: report of a case. Surg Today. 1999;29:375-377. [PubMed] |
| 6. | Musallam KM, Taher AT, Tawil AN, Chakhachiro ZI, Habbal MZ, Shamseddine AI. Solitary mediastinal lymph node metastasis in rectosigmoid carcinoma: a case report. Cases J. 2008;1:69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | McLoud TC, Kalisher L, Stark P, Greene R. Intrathoracic lymph node metastases from extrathoracic neoplasms. AJR Am J Roentgenol. 1978;131:403-407. [PubMed] |
| 8. | Latour A, Shulman HS. Thoracic manifestations of renal cell carcinoma. Radiology. 1976;121:43-48. [PubMed] |
| 10. | Libson E, Bloom RA, Halperin I, Peretz T, Husband JE. Mediastinal lymph node metastases from gastrointestinal carcinoma. Cancer. 1987;59:1490-1493. [PubMed] |
| 11. | Kobayashi M, Okubo K, Morikawa H, Hayatsu E. Evaluation of Mediastinal Node Metastasis in Lung Cancer by FDG-PET. Jpn J Lung Cancer. 2007;47:233-238. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Tsubaki M, Nemoto K, Yoda N, Hasimoto R, Sunagawa M, Masawa N. Sigmoid colon cancer with mediastinal lymph node metastases. Int Surg. 2007;92:209-213. [PubMed] |
| 13. | Kitami A, Suzuki T, Suzuki S, Hori G. Two Cases of Postoperative Mediastinal Lymph Nodes Metastasis of Colonic Cancer. J Jpn Soc Clin Surg. 1995;56:2595-2598. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Kawasaki M, Kameyama M, Imagawa A, Ueki T, Yamazaki K, Sonoo H, Ogawa M, Demura K, Ooba K, Fujio N. Resection of Para-aortic Lymph Node Metastases of Colorectal Cancer. Jpn J Gastroenterol Surg. 2011;44:1097-1104. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Min BS, Kim NK, Sohn SK, Cho CH, Lee KY, Baik SH. Isolated paraaortic lymph-node recurrence after the curative resection of colorectal carcinoma. J Surg Oncol. 2008;97:136-140. [PubMed] |