Published online Feb 27, 2014. doi: 10.4240/wjgs.v6.i2.33
Revised: December 12, 2013
Accepted: January 13, 2014
Published online: February 27, 2014
Processing time: 348 Days and 5.4 Hours
Primary tumors of the diaphragm are quite rare. About 150 cases have been reported in the literature. Fibrosarcomas are the commonest malignant neoplasms of the diaphragm; however, only a few (less than 20) cases have been reported to date. We present the case of an extremely rare tumor of the diaphragm mimicking a liver mass. The patient, a young 28-year-old woman, presented with an 8-month-history of mildly progressive upper abdominal pain and early fullness after meals. Computed tomography scan of the abdomen revealed a mass located in the region of the left lobe of the liver with non visualized left lobe and partial vascular supply of the mass from the left hepatic artery. The tumor was also seen to draw its vascularity from bilateral internal mammary arteries. Surgical excision and hepatectomy was planned, keeping in mind the diagnosis of an atypical left hepatic mass. Laparotomy revealed a left diaphragmatic tumor growing caudally into the upper abdomen, compressing and splaying the liver along the left medial surface where the tumor was virtually adherent to it. Successful excision of the mass and subsequent histopathological and immunochemistry examination of the specimen revealed low grade fibromyxoid sarcoma of the diaphragm. This case highlights the unusual presentation of a diaphragmatic mesenchymal tumor and how it can be mistaken as an atypical liver mass. It also emphasizes the tumoral vascular supply as an indicator of its organ of origin.
Core tip: In this paper, a patient with low grade fibromyxoid sarcoma of the diaphragm which mimicked a liver mass on preoperative imaging is reported. Particular attention is paid to retrospective analysis of the vascularity of the mass on computed tomography angiography to differentiate it as an extrahepatic mass. The histopathological analysis of this case, as well as a collective review, is also presented in this report.
- Citation: Thapar S, Ahuja A, Rastogi A. Rare diaphragmatic tumor mimicking liver mass. World J Gastrointest Surg 2014; 6(2): 33-37
- URL: https://www.wjgnet.com/1948-9366/full/v6/i2/33.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i2.33
Primary tumors of the diaphragm have a rare incidence and prevalence. Only about 150 cases have been reported in literature to date[1-5]. Most primary tumors of the diaphragm are benign. Of the malignant subgroup, fibrosarcoma appears to be the commonest. Low grade fibromyxoid sarcoma (LGFMS) is a unique sub entity in the group of fibrosarcomas. These tumors are unique in their reappearance as metastases after significant time intervals. Around 20 cases of the same have been reported in the English literature so far, to the best of our knowledge[1-7]. LGFMS shows characteristic histopathological and immunochemistry features. In the last decade, sporadic cases of fibromyxoid sarcoma have been reported in the literature. Even after recent major advances in imaging technology, such as the advent of multidetector, multi slice computed tomography (CT) and 3Tesla magnetic resonance imaging (MRI), diaphragmatic tumors still present as a diagnostic dilemna and are difficult to diagnose preoperatively or without a pathological diagnosis. They are known to mimic other large masses arising from the mediastinum in the majority of cases. In this paper, a patient with low grade fibromyxoid sarcoma of the diaphragm which mimicked a liver mass on preoperative imaging is reported. Particular attention is paid to retrospective analysis of the vascularity of the mass on CT angiography to differentiate it as an extrahepatic mass. The histopathological analysis of this case, as well as a collective review, is also presented in this report.
A 28-year-old lady presented to the hospital with an 8 mo progressive history of nagging upper abdominal pain and a feeling of early satiety. The pain was localized without associated vomiting, aggravating or relieving factors. The patient complained of feeling a gradually increasing lump in the upper abdomen for 6 mo. However, she had no definite history of cough, hiccups or difficulty in breathing. The lady had loss of appetite with significant weight loss of 5 kg over 6 mo. On general examination, the lady was well preserved. Local palpation revealed a firm lump in the epigastrium and left hypochondrium with a perceptible lower border. Palpating fingers could not be insinuated between the lump and the upper border, as well as the costal margin. Laboratory tests showed normal serum alpha fetoprotein and carcinoembryonic antigen levels (1.16 U) and (1.8 mg/L) respectively. All other tests, such as hemogram, kidney function tests and liver function tests, were within the normal reference ranges.
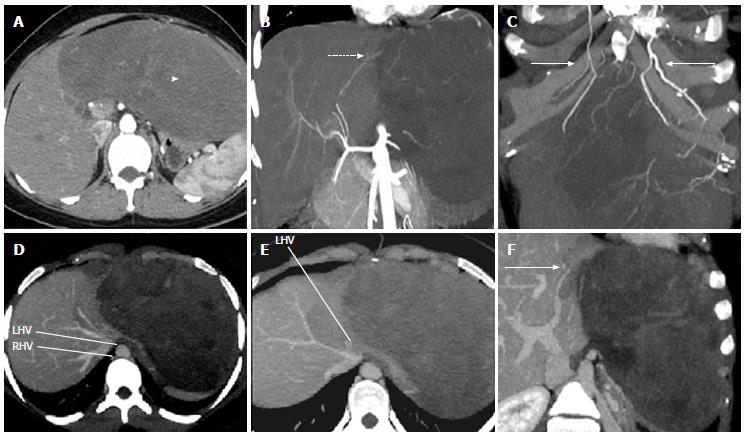
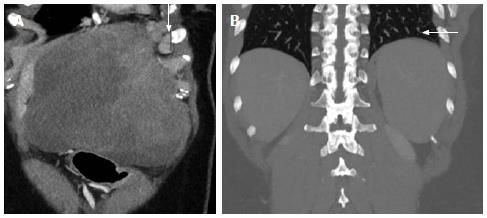
A dynamic triple phase CT scan of the upper abdomen was performed and showed a homogenous soft tissue mass lesion measuring approximately 25 cm × 20 cm × 13.5 cm in the left upper hypochondrium, almost entirely replacing the left lobe of the liver (Figure 1A). The left hepatic vein and portal vein were only partially visualized and were grossly attenuated by the mass (Figure 1E-G). Enlarged left supra-diaphragmatic nodes were present (Figure 2A). The sections of bilateral lower lobes of chest did not show evidence of basal atelectasis or pleural effusion (Figure 2B). The tumor showed arterial feeders from the left hepatic artery which was splayed but showed normal patency (Figure 1B). The major chunk of tumor vascularity appeared to be from bilateral internal mammary arteries (Figure 1C). The tumor appearance was thought to be of an atypical hepatic mass and a decision for surgical laparotomy with surgical excision of the tumor was made.
On laparotomy, a solid, rounded, grey tumor was found arising from the left diaphragm, compressing and splaying the entire left lobe of liver which was adherent to the tumor medially. The upper border of the mass was attached to the inferior surface of the left diaphragm. The entire mass was excised along with the left lower 3 ribs from which it was inseparable. The superficial structures of the left chest wall were not involved. Local left supra-diaphragmatic lymph nodes were also excised.
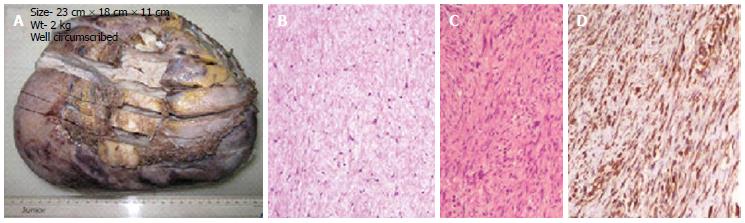
The tumor was well encapsulated, firm, weighed approximately 2 kg and measured 23 cm × 18 cm × 11 cm (Figure 3A). Microscopy revealed a bland appearing spindle cell tumor of low cellularity. The tumor showed contrasting fibrous and myxoid areas (Figure 3B). The spindle cells demonstrated a focal swirling or whorled pattern. On high power, the tumor cells showed minimal pleomorphism without any mitosis. Focally, tumor cells appeared stellate shaped. Few areas showed curvilinear or capillary sized blood vessels with spindle cells encasing around them (Figure 3C). Immunohistochemistry revealed strong positive immunostaining of the spindle cells with vimentin and focally for Bcl-2 (Figure 3D), but negative for S100, smooth muscle antigen, desmin, epithelial membrane antigen and CD34. Based on characteristic histomorphological features and immunohistochemistry results, a diagnosis of low grade fibromyxoid sarcoma was made.
The patient was offered radiation therapy, which she refused. At the 1 year follow up, she is symptom free, with no evidence of disease spread.
Primary tumors of the diaphragm are very rare. The first diaphragmatic tumor was reported in 1868 by Grancher[8]. About 150 cases have been reported in the English literature since then[9]. The majority of diaphragmatic tumors are benign. Most malignant tumors of the diaphragm are sarcomas of fibrous or muscular origin[7].
They include leiomyosarcoma, germ cell tumors, hemangiopericytoma, pheochromocytoma, fibrosarcoma and malignant fibrous histiocytoma. On imaging, most diaphragmatic tumors present as homogenous masses which appear as mediastinal or thoracic masses with contour abnormality of the diaphragmatic leaves, suggesting herniation or eventration. Although multiplanar imaging with CT and MRI are almost first line modes of investigation in the present era, large tumors may sometimes pose a diagnostic difficulty. A differential diagnosis of lung, mediastinal, pleural, vertebral or upper abdominal masses has to be considered in such situations. All of the above tumors may sometimes grow to large proportions without any specific clinical symptoms. Secondary involvement of the diaphragm from adjacent structures may also be present. Symptoms are usually produced due to esophageal, stomach or mediastinal compression and not due to the tumor bulk.
The patient in our study also reported vague symptoms, which did not raise any suspicion about the extent of the mass. Imaging provided the only clue to the large size and extent of the tumor, which was solely limited to the upper abdomen. The initial suspicion of a liver mass was compounded by the vascular supply of the mass from the left hepatic artery. However, in retrospect, the majority of the tumor blood supply from bilateral internal mammary arteries was indicative of the extrahepatic origin of the tumor. The sharp interface of the mass with the liver parenchyma despite the lack of a proper cleavage plane was also a soft indicator of the extrahepatic origin.
Low-grade fibromyxoid sarcomas are distinctive, indolent soft-tissue sarcomas, first described by Evans in 1987. Low grade fibromyxoid sarcoma of the diaphragm is extremely rare. From 1868 to 1982, only 11 cases of low grade fibrosarcoma were reported[4]. Less than 20 cases have been reported in literature to date, to the best of our knowledge[1-3,6,7]. The sites described in literature so far have been commonly in the shoulder, neck or thigh[1]. On histopathology, low-grade fibromyxoid sarcomas demonstrate contrasting fibrous and myxoid areas, a swirling, whorled growth pattern and bland benign-appearing fibroblastic spindle cells. Cellularity is low to moderate, mitotic figures are uncommon, and nuclear pleomorphism is usually absent or slight. In addition, LFGMS shows a specific genetic transcript fused in sarcoma-cAMP responsive element binding protein 3 (FUS-CREB3)L2 and FUS-CREB3L1 in up to 95%-100% of cases[10]. The common differentials of low grade fibromyxoid sarcoma include myxoid neurofibroma, malignant peripheral nerve sheath tumor of low grade, myxofibrosarcoma and spindle cell liposarcoma. Myxoid neurofibroma and low grade malignant peripheral nerve sheath tumor show slender and wavy nuclei which are positive for S100. Myxofibrosarcoma is mostly a subcutaneous tumor of the elderly and shows a greater degree of nuclear pleomorphism, hyperchromasia and brisk mitosis. Spindle cell liposarcoma is cellular and shows more nuclear atypia. It always contains an atypical adipocytic component which includes the presence of lipoblasts and shows positivity for S100.
Primary diaphragmatic fibromyxoid sarcomas, especially low grade like in this case, have a good prognosis. One of the reports has shown survival even up to 10 years[7]. Treatment options include surgery followed by radiotherapy and, in some cases, chemotherapy to shrink tumor bulk, followed by resection. These tumors are usually resistant to chemotherapy and radiotherapy with surgical resection being the treatment of choice[11].
In conclusion, this case highlights that an extrahepatic vascular supply may act as an indicator of the extrahepatic origin of a tumor showing indistinct fat planes from the liver. Also, although rare, diaphragmatic mesenchymal tumors should also be included in the differential of atypical appearing hepatic or extrahepatic masses in the upper abdomen. In a recent study at a dedicated sarcoma centre in Denmark where 14 patients of LGFMS were studied for the disease and metastases treatment strategies, multi-agent chemotherapy was found useful, especially in the setting of metastases. The best possible response to chemotherapy was only a short term disease non progression with the use of trabectedin[12].
We thank Rita Gulabani for transcription help and Abhishek Anand and Dhananjay Kumar for their technical assistance.
The patient, a young-28-year old woman, presented with an 8-mo-history of mildly progressive upper abdominal pain and early fullness after meals.
The patient complained of feeling a gradually increasing lump in the upper abdomen for 6 mo.
Laboratory tests showed normal serum alpha fetoprotein and carcinoembryonic antigen levels (1.16 U) and (1.8 mg/L) respectively.
Computed tomography scan of the abdomen revealed a mass located in the region of left lobe of liver with non visualized left lobe and partial vascular supply of the mass from the left hepatic artery.
Immunohistochemistry revealed strong positive immunostaining of the spindle cells with vimentin and focally for Bcl-2, but negative for S100, smooth muscle antigen, desmin, epithelial membrane antigen and CD34.
Surgical excision and hepatectomy was planned, keeping in mind the diagnosis of an atypical left hepatic mass.
This case highlights that extrahepatic vascular supply may act as an indicator of the extrahepatic origin of a tumor showing indistinct fat planes from the liver.
The authors need to discuss pathological findings in more detail to substantiate the diagnosis of Low grade fibromyxoid sarcoma at this relatively uncommon location.
P- Reviewer: Rekhi B S- Editor: Zhai HH L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Evans HL. Low-grade fibromyxoid sarcoma: a clinicopathologic study of 33 cases with long-term follow-up. Am J Surg Pathol. 2011;35:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 169] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 2. | Wiener MF, Chou wh. primary tumors of the diaphragm. Arch Surg. 1965;90:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Olafsson G, Rausing A, Holen O. Primary tumors of the diaphragm. Chest. 1971;59:568-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Mandal AK, Lee H, Salem F. Review of primary tumors of the diaphragm. J Natl Med Assoc. 1988;80:214-217. [PubMed] |
| 5. | Midorikawa Y, Kubota K, Mori M, Koyama H, Aihara N, Makuuchi M, Kajiura N. Rhabdomyosarcoma of the diaphragm: report of an adult case. Jpn J Clin Oncol. 1998;28:222-226. [PubMed] |
| 6. | Zhang H, Wu D, Wang Z, Xu J, Wang H. Primary fibrosarcoma of the diaphragm with pleural effusion. Clin Respir J. 2010;4:127-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Sbokos CG, Salama FD, Powell V, McMillan IK. Primary fibrosarcoma of the diaphragm. Br J Dis Chest. 1977;71:49-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Weksler B, Ginsberg RJ. Tumors of the diaphragm. Chest Surg Clin N Am. 1998;8:441-447. [PubMed] |
| 9. | Cada M, Gerstle JT, Traubici J, Ngan BY, Capra ML. Approach to diagnosis and treatment of pediatric primary tumors of the diaphragm. J Pediatr Surg. 2006;41:1722-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Mertens F, Fletcher CD, Antonescu CR, Coindre JM, Colecchia M, Domanski HA, Downs-Kelly E, Fisher C, Goldblum JR, Guillou L. Clinicopathologic and molecular genetic characterization of low-grade fibromyxoid sarcoma, and cloning of a novel FUS/CREB3L1 fusion gene. Lab Invest. 2005;85:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 206] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 11. | Menon S, Krivanek M, Cohen R. Low-grade fibromyxoid sarcoma, a deceptively benign tumor in a 5-year-old child. Pediatr Surg Int. 2012;28:211-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Maretty-Nielsen K, Baerentzen S, Keller J, Dyrop HB, Safwat A. Low-Grade Fibromyxoid Sarcoma: Incidence, Treatment Strategy of Metastases, and Clinical Significance of the FUS Gene. Sarcoma. 2013;2013:256280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |