Published online Dec 27, 2014. doi: 10.4240/wjgs.v6.i12.235
Revised: October 9, 2014
Accepted: November 17, 2014
Published online: December 27, 2014
Processing time: 195 Days and 10.7 Hours
AIM: To demonstrate a new surgical technique of lower mediastinal lymphadenectomy and intrathoracic anastomosis of esophagojejunostomy using OrVil™.
METHODS: After a total median phrenotomy, the supradiaphragmatic and lower thoracic paraesophageal lymph nodes were transhiatally dissected. The esophagus was cut off using a liner stapler and OrVil™was inserted. Finally, end-to-side esophagojejunostomy was created by using a circular stapler. From July 2009, we adopted this surgical technique for five patients with gastric cancer involving the lower esophagus.
RESULTS: The median operation time was 314 min (range; 210-367 min), and median blood loss was 210 mL (range; 100-838 mL). The median numbers of dissected lower mediastinal nodes were 3 (range; 1-10). None of the patients had postoperative complications including anastomotic leakage and stenosis. The median hospital stay was 16 d (range: 15-20 d). The median length of esophageal involvement was 14 mm (range: 6-48 mm) and that of the resected esophagus was 40 mm (range: 35-55 mm); all resected specimens had tumor-free margins.
CONCLUSION: This surgical technique is easy and safe intrathoracic anastomosis for the patients with gastric adenocarcinoma involving the lower esophagus.
Core tip: We report a new technique of lower intrathoracic anastomosis through the transhiatal approach using OrVil™ for five patients with gastric adenocarcinoma involving the esophagus. This surgical technique is an easy and safe method to create lower intrathoracic anastomosis.
- Citation: Yajima K, Kanda T, Kosugi SI, Kano Y, Ishikawa T, Ichikawa H, Hanyu T, Wakai T. Intrathoracic esophagojejunostomy using OrVil™ for gastric adenocarcinoma involving the esophagus. World J Gastrointest Surg 2014; 6(12): 235-240
- URL: https://www.wjgnet.com/1948-9366/full/v6/i12/235.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v6.i12.235
Adenocarcinoma of the esophagogastric junction (EGJ) is still uncommon in Japan although the number of patients with this disease has tended to increase[1-6]. For gastric cancer surgery, ensuring safe cancer-free margins and dedicated systematic lymphadenectomy are both important; however, it is sometimes difficult to achieve these two surgical principles in surgery for gastric adenocarcinoma involving the lower esophagus because of the anatomical complexity of the EGJ. Surgical approach for adenocarcinoma of the EGJ includes transhiatal, transthoracic, and left thoracoabdominal approach.
On the basis of the results of a randomized controlled trial by the Japan Clinical Oncology Group (JCOG 9502) comparing the transhiatal with the left thoracoabdominal approach on the prognosis of patients with Siewert type II or III adenocarcinoma that extended 3 cm or less to the esophagus[7], the Japan Gastric Cancer Guideline recommends the transhiatal approach for patients with this disease[8]. Resection of the long esophageal segment through the transhiatal approach is relatively easy; however, anastomosis becomes increasingly difficult as the resected esophagus is long because the remnant esophagus has shrunk and is hidden behind the heart. The conventional method using purse-string sutures is unstable in a deep and narrow working space. Insertion of an anvil into the distal esophagus is technically difficult and stressful.
Recently, a double stapling technique with a transoral anvil delivery system (EEA™ OrVil™, Covidien Japan, Tokyo, Japan) has been used for enteral anastomoses in laparoscopy-assisted gastrectomy[9-18]. With steady insertion of the anvil, the trans-oral anvil delivery system enables safe anastomosis in surgeries that permit only small working spaces.
This is a preliminary case series of five patients with gastric adenocarcinoma involving the esophagus who underwent lower intrathoracic anastomosis through the transhiatal approach using EEA™ OrVil™.
Between July 2009 and December 2012, five consecutive patients with gastric adenocarcinoma involving the esophagus underwent esophagojejunostomy using a transoral delivery system following total gastrectomy combined with lower esophagectomy. Patients’ clinical backgrounds are shown in Table 1. Preoperative staging was based on upper gastrointestinal endoscopy, fluoroscopy, and thoracic-abdominal computed tomography scans. All the patients had histologically confirmed gastric adenocarcinoma, of which esophageal involvement was clinically evaluated as 3 cm or shorter. No patients had any evidence of lymph node metastasis in the middle or upper mediastinum. Tumor details were described according to the Japanese classification of gastric carcinoma, 3rd English edition[19].
| Case | Age (yr) | Sex | Tumor location | Siewert classification | C-length (mm) | C-stage | Co-morbidity | Neoadjuvant chemotherapy |
| 1 | 73 | M | EU | Type I | 30 | T3(SS)N0M0 | DM | N |
| 2 | 52 | M | UME | Others | 14 | T3(SS)N1M0 | DM | N |
| 3 | 80 | M | EU | Type II | 21 | T3(SS)N1M0 | CI | N |
| 4 | 67 | M | UE | Type II | 10 | T1b(SM)N0M0 | DM, COPD | N |
| 5 | 55 | M | UE | Type III | 12 | T3(SS)N2M0 | COPD | S-1 + CDDP |
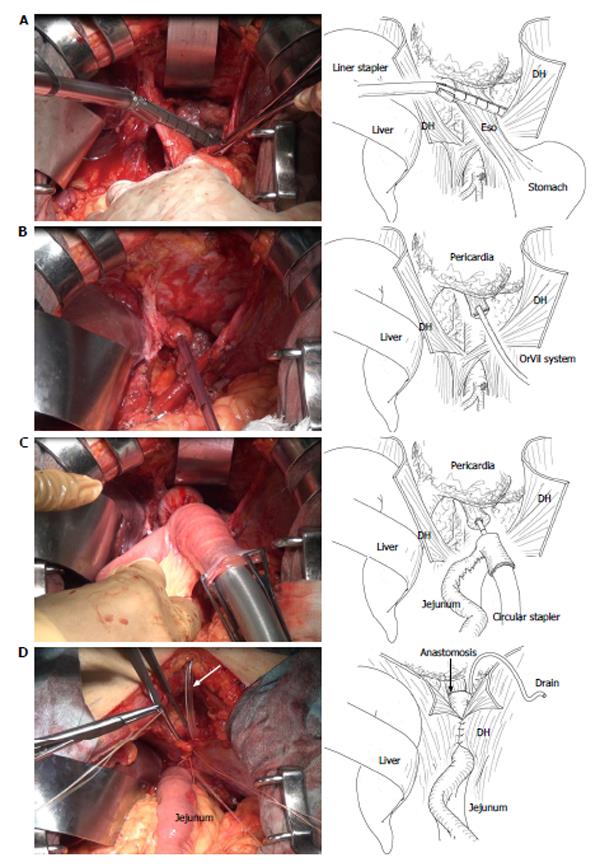
All patients underwent lower mediastinal lymphadenectomy through transhiatal approach, details of which were described elsewhere[20]. After completion of lymphadenectomy, the mobilized esophagus was transected 2 cm above the tumor margin using an Endo GIA (60 mm, purple; Covidien Japan) linear stapler (Figure 1A). The OrVil™ tube was then introduced transorally into the esophagus. As the surgeon identified the OrVil tube reaching the esophageal stump, a small hole was created in the esophageal stump (Figure 1B). The tube was carefully pulled out and then the transoral anvil was positioned at the esophageal stump. Esophagojejunostomy was performed using the Roux-en-Y method. A jejunal loop was pulled-up retrocolically after dividing the jejunum approximately 20 cm from the ligament of Treitz. A circular stapler (DST Series EEA™ Stapler 25; Covidien Japan) was inserted into the jejunal stump and the anvil was connected to the circular stapler (Figure 1C). After an end-to-side anastomosis was performed using the stapler, the jejunal stump was closed with Endo GIA (60 mm, purple), completing the lower intrathoracic esophagojejunostomy. A drainage tube (Salem Sump dual lumen stomach tube, 16 Fr; Covidien Japan) was inserted from the anterior chest wall through the space between the pericardium and diaphragm and positioned in the left-side chest cavity (Figure 1D). The drainage was suctioned continuously with low pressure (12 cm H2O) after the surgery. The schema of the figures were showed below of the Figure 1.
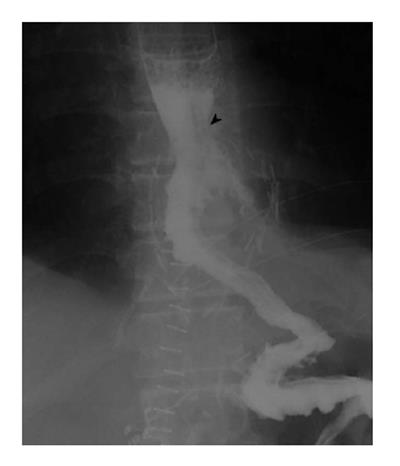
Surgical outcomes of the five patients are shown in Table 2. All patients successfully underwent this surgical technique with no intraoperative complications. The median operation time was 314 min (range: 210-367 min), and median blood loss was 210 mL (range: 100-838 mL). The median interval to water intake was 2 d (range: 1-3 d) and that to oral intake was 7 d (range: 6-10 d). None of the patients had postoperative surgical complications. Postoperative fluorography demonstrated no leakage or stenosis of the esophagojejunal anastomosis in all five patients. Figure 2 shows representative fluorography of the esophagojejunal anastomosis. The median hospital stay was 16 d (range: 15-20 d).
| Case | Surgical | Lymph- | Residual | Operation time | Blood loss | Start of foods | Hospital stay | E-length | P-length |
| procedures | adenectomy | tumor | (min) | (mL) | (d) | (d) | (mm) | (mm) | |
| 1 | Total GR, RY | D2 | R0 | 367 | 838 | 10 | 20 | 55 | 48 |
| 2 | Total GR, RY | D2 | R0 | 314 | 270 | 10 | 16 | 40 | 14 |
| 3 | Total GR, RY | D2 | R0 | 210 | 210 | 7 | 15 | 52 | 22 |
| 4 | Proximal GR, JI | D1+ | R0 | 314 | 100 | 7 | 18 | 36 | 6 |
| 5 | Total GR, RY | D2 | R0 | 277 | 140 | 6 | 15 | 35 | 10 |
The median length of esophageal involvement was 14 mm (range: 6-48 mm) and that of the resected esophagus was 40 mm (range: 35-55 mm); all resected specimens had tumor-free margins.
We have herein reported the use of the EEA™ OrVil™ stapler in end-to-side anastomosis for esophagojejunostomy for patients with gastric adenocarcinoma involving the esophagus. To the best of our knowledge, this is the first report of the use of a transoral anvil in lower intrathoracic esophagojejunostomy and our preliminary results showed that this technique was feasible and safe.
By literature review of PubMed database using the keywords “OrVil™”, “gastric cancer”, and “esophagojejunostomy”, there were ten original reports describing the outcomes of esophagojejunostomy using a transoral anvil (EEA™ OrVil™) so far. However, all five reports addressed the issues of esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer[9-18]. Jeong et al[9] reported that of the 16 patients who underwent esophagojejunostomy using OrVil™ in laparoscopy-assisted total gastrectomy, no patient had intraoperative complications or anastomotic complications, including leakage and stenosis. Liao et al[11] also supported the safety of esophagojejunostomy using a transoral anvil: anastomotic leakage and anastomotic stenosis occurred in one patient in their series of 21 patients undergoing laparoscopy-assisted total gastrectomy. From these reports, gastrojejunostomy using OrVil™ was acceptable in terms of fewer anastomotic complications. We successfully performed intrathoracic anastomosis with Roux-en-Y reconstruction in five patients without any anastomotic complications.
Complete resection with no residual tumor remains the only treatment that can lead to cure in gastric cancer[21]. Obtaining a safe free margin of the distal esophagus is one of the most important problems, especially in patients with junctional cancer invading the esophagus. On the other hand, the correlation between the length of esophageal resection and free surgical margin has not been well described. In the JCOG9502 trial, the median length of the resected esophagus was 4.2 cm in the transhiatal approach, with two having positive proximal margin[7]. In the present study, the median length of the resected esophagus was 40 mm and all patients had a negative proximal margin. In our technique exposing the lower mediastinum by dissection using a lower mediastinal lymphadenectomy, a wide and good view was obtained. Using this space, we could easily cut the esophagus and insert the anvil head transorally with a sufficient tumor-free margin.
Insertion of an anvil into the distal esophagus is technically difficult and stressful for the esophagojejunostomy. Kunisaki et al[10] and Liao et al[11] reported that total operation time and time of reconstruction were significantly shortened when comparing mini-laparotomy and a transorally inserted anvil in laparoscopy-assisted total gastrectomy esophagojejunostomy using OrVil™. At the same way, OrVil™ might decrease the time of reconstruction also in conventional open gastrectomy when intrathoracic anastomosis. In our series, unfortunately, the time of anastomosis was not measured, there were no trouble concerning the insertion of the OrVil and anastomosis using EEA™ during surgery. In our experience, lower intrathoracic esophagojejunostomy using OrVil™ was less stressful technique.
In conclusion, we report the surgical techniques of the EEA™ OrVil™ stapler in end-to-side anastomosis for esophagojejunostomy. We believe that this technique is especially useful for patients with lower intrathoracic anastomosis, in whom conventional anastomosis is difficult.
For gastric cancer surgery, ensuring safe cancer-free margins and dedicated systematic lymphadenectomy are both important; however, it is sometimes difficult to achieve these two surgical principles in surgery for gastric adenocarcinoma involving the lower esophagus because of the anatomical complexity of the esophagogastric junction.
A double stapling technique with a transoral anvil delivery system (EEA™ OrVil™, Covidien Japan, Tokyo, Japan) has been used for enteral anastomoses in laparoscopy-assisted gastrectomy. With steady insertion of the anvil, the trans-oral anvil delivery system enables safe anastomosis in surgeries that permit only small working spaces.
The authors demonstrate a new surgical technique of lower mediastinal lymphadenectomy and intrathoracic anastomosis of esophagojejunostomy using OrVil™. This is the first report of the use of a transoral anvil in lower intrathoracic esophagojejunostomy and our preliminary results showed that this technique was feasible and safe.
By understanding surgical procedures, this study demonstrates the photographs during the surgery and the schema of the photographs.
A transoral anvil delivery system (EEA™ OrVil™) is one of the surgical items of anvil placement for circler stapling technique.
The authors preliminarily demonstrated the use of the EEA™ OrVil™ stapler in end-to-side anastomosis for esophagojejunostomy and usefulness and safely in five patients. This surgical technique is easy and safe intrathoracic anastomosis for the patients with gastric adenocarcinoma involving the lower esophagus.
P- Reviewer: Aoyagi K, Tiberio GAM S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Powell J, McConkey CC. Increasing incidence of adenocarcinoma of the gastric cardia and adjacent sites. Br J Cancer. 1990;62:440-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 264] [Cited by in RCA: 279] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | Devesa SS, Blot WJ, Fraumeni JF. Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer. 1998;83:2049-2053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 3. | Blot WJ, Devesa SS, Kneller RW, Fraumeni JF. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265:1287-1289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1287] [Cited by in RCA: 1150] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 4. | Hasegawa S, Yoshikawa T. Adenocarcinoma of the esophagogastric junction: incidence, characteristics, and treatment strategies. Gastric Cancer. 2010;13:63-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 112] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Hasegawa S, Yoshikawa T, Cho H, Tsuburaya A, Kobayashi O. Is adenocarcinoma of the esophagogastric junction different between Japan and western countries? The incidence and clinicopathological features at a Japanese high-volume cancer center. World J Surg. 2009;33:95-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 6. | Hosokawa Y, Kinoshita T, Konishi M, Takahashi S, Gotohda N, Kato Y, Daiko H, Nishimura M, Katsumata K, Sugiyama Y. Clinicopathological features and prognostic factors of adenocarcinoma of the esophagogastric junction according to Siewert classification: experiences at a single institution in Japan. Ann Surg Oncol. 2012;19:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 7. | Sasako M, Sano T, Yamamoto S, Sairenji M, Arai K, Kinoshita T, Nashimoto A, Hiratsuka M. Left thoracoabdominal approach versus abdominal-transhiatal approach for gastric cancer of the cardia or subcardia: a randomised controlled trial. Lancet Oncol. 2006;7:644-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 304] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 8. | Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1723] [Cited by in RCA: 1897] [Article Influence: 135.5] [Reference Citation Analysis (0)] |
| 9. | Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc. 2009;23:2624-2630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 149] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 10. | Kunisaki C, Makino H, Oshima T, Fujii S, Kimura J, Takagawa R, Kosaka T, Akiyama H, Morita S, Endo I. Application of the transorally inserted anvil (OrVil) after laparoscopy-assisted total gastrectomy. Surg Endosc. 2011;25:1300-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Liao GQ, Ou XW, Liu SQ, Zhang SR, Huang W. Laparoscopy-assisted total gastrectomy with trans-orally inserted anvil (OrVil™): a single institution experience. World J Gastroenterol. 2013;19:755-760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Hirahara N, Monma H, Shimojo Y, Matsubara T, Hyakudomi R, Yano S, Tanaka T. Reconstruction of the esophagojejunostomy by double stapling method using EEA™ OrVil™ in laparoscopic total gastrectomy and proximal gastrectomy. World J Surg Oncol. 2011;9:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Bose KS, Sarma RH. Delineation of the intimate details of the backbone conformation of pyridine nucleotide coenzymes in aqueous solution. Biochem Biophys Res Commun. 1975;66:1173-1179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Jung YJ, Kim DJ, Lee JH, Kim W. Safety of intracorporeal circular stapling esophagojejunostomy using trans-orally inserted anvil (OrVil) following laparoscopic total or proximal gastrectomy - comparison with extracorporeal anastomosis. World J Surg Oncol. 2013;11:209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | LaFemina J, Viñuela EF, Schattner MA, Gerdes H, Strong VE. Esophagojejunal reconstruction after total gastrectomy for gastric cancer using a transorally inserted anvil delivery system. Ann Surg Oncol. 2013;20:2975-2983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 16. | Hirahara N, Tanaka T, Yano S, Yamanoi A, Minari Y, Kawabata Y, Ueda S, Hira E, Yamamoto T, Nishi T. Reconstruction of the gastrointestinal tract by hemi-double stapling method for the esophagus and jejunum using EEA OrVil in laparoscopic total gastrectomy and proximal gastrectomy. Surg Laparosc Endosc Percutan Tech. 2011;21:e11-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Ito H, Inoue H, Odaka N, Satodate H, Onimaru M, Ikeda H, Takayanagi D, Nakahara K, Kudo SE. Evaluation of the safety and efficacy of esophagojejunostomy after totally laparoscopic total gastrectomy using a trans-orally inserted anvil: a single-center comparative study. Surg Endosc. 2014;28:1929-1935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | Shim JH, Yoo HM, Oh SI, Nam MJ, Jeon HM, Park CH, Song KY. Various types of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer. Gastric Cancer. 2013;16:420-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2390] [Cited by in RCA: 2873] [Article Influence: 205.2] [Reference Citation Analysis (0)] |
| 20. | Suzuki T, Nishimaki T, Kanda T, Obinata I, Nakagawa S, Hatakeyama K. Transhiatal radical En Bloc dissection of the low- and mid- mediastinum for vardioesophageal carcinomas. Acta medica et Biologica. 1998;46:153-159. |
| 21. | Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, Tsujinaka T, Kinoshita T, Arai K, Yamamura Y. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol. 2004;22:2767-2773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 493] [Article Influence: 23.5] [Reference Citation Analysis (0)] |