Published online Jan 27, 2011. doi: 10.4240/wjgs.v3.i1.13
Revised: December 31, 2010
Accepted: January 7, 2011
Published online: January 27, 2011
The occurrence of intussusception in adults is rare, accounting for less than 5% of all cases of intussusceptions and almost 1%-5% of bowel obstruction. The condition is found in less than 1 in 1300 abdominal operations and 1 in 100 patients operated for intestinal obstruction. The child to adult ratio is more than 20:1. We report a rare case of ileocolic intussusception in an adult secondary to an ileal lipoma.
- Citation: Balamoun H, Doughan S. Ileal lipoma - a rare cause of ileocolic intussusception in adults: Case report and literature review. World J Gastrointest Surg 2011; 3(1): 13-15
- URL: https://www.wjgnet.com/1948-9366/full/v3/i1/13.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v3.i1.13
The occurrence of intussusception in adults is rare, accounting for less than 5% of all cases of intussusceptions and almost 1%-5% of bowel obstruction. The condition is found in less than 1 in 1300 abdominal operations and 1 in 100 patients operated for intestinal obstruction. The child to adult ratio is more than 20:1. We report a rare case of ileocolic intussusception in an adult secondary to an ileal lipoma.
A 65-year old man presented with a three day history of colicky abdominal pain and bilious vomiting. He had a weight loss of 10 kg in the preceding year. His past medical history included duodenal ulcer surgery 27 years ago and an appendicectomy during childhood.
On examination, he was apyrexial and hemodynamically stable. His abdomen was distended with localized tenderness in the right iliac fossa and no palpable abdominal masses; bowel sounds were hyperaudible. Initial laboratory blood tests were normal.
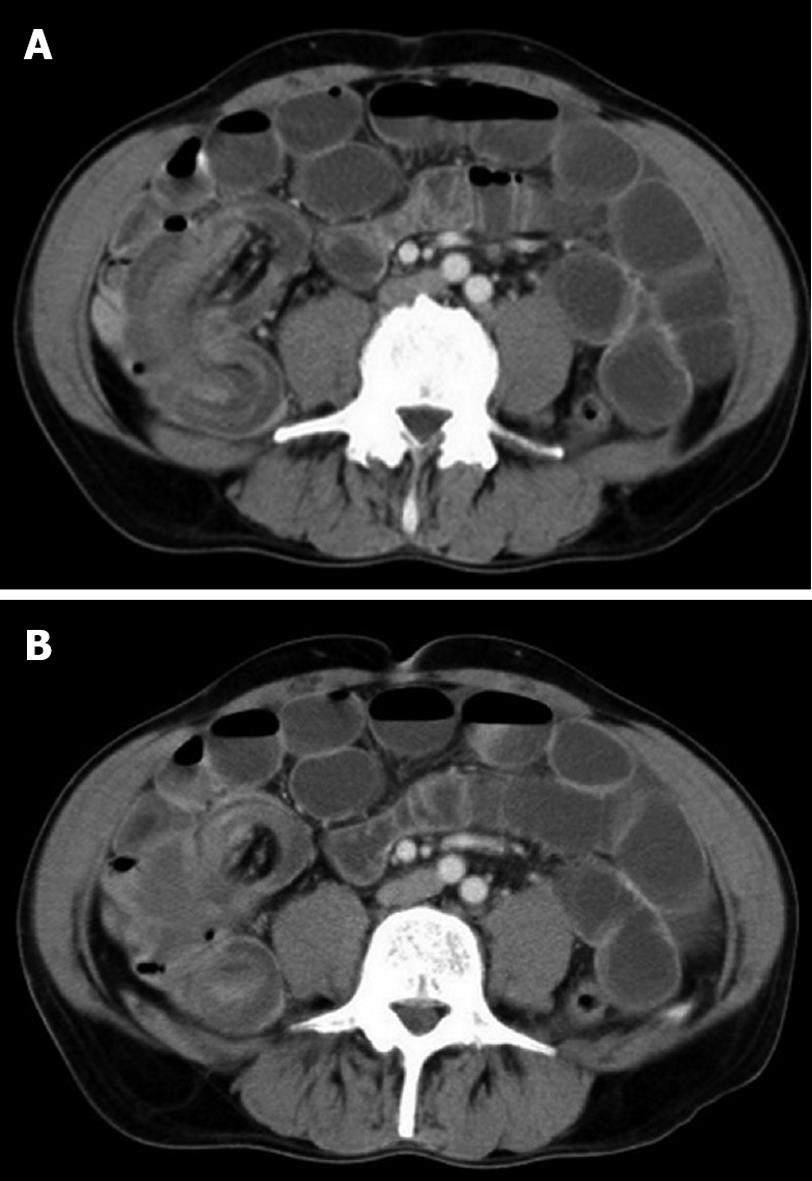
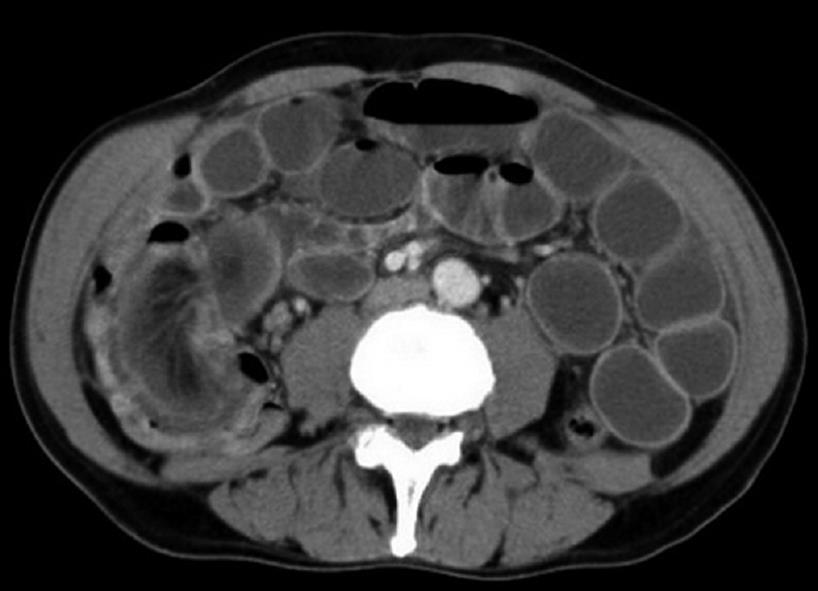
Plain abdominal X-ray showed dilated small bowel loops (Figure 1) with no evidence of free intraperitoneal air on chest X-ray. Computed tomography (CT) scan of the abdomen and pelvis showed findings suggestive of ileocolic intussusception (Figure 2A and B). The leading point was a 12 mm fatty density structure within the bowel lumen and separate from the mesentery (Figure 3). The decision was made to undertake an urgent exploratory laparotomy.
At laparotomy, ileocolic intussusception (Figure 4) was found for which a right hemicolectomy with ileo-tranvserse colon anastomosis was performed. The patient had an uneventful postoperative recovery. The histopathology report confirmed a 12-mm submucosal lipoma in the terminal ileum as a cause for a 15-cm ileocolic intussusception. There was no evidence of dysplasia or malignancy.
Intussusceptions are classified according to location. The most common classification system divides intussusception into four categories: enteric, ileocolic, ileocaecal and colonic[1-4]. Enteric and colonic intussusceptions are those that are confined to the small intestine and large intestine respectively. Ileocolic intussusceptions are defined as those with prolapse of the ileum through the ileocaecal valve into the colon and these constitute 15% of all intussusceptions. The ileocaecal valve and the appendix preserve their normal anatomical position and the organic lesion is usually in the ileum[4,5]. These organic lesions are mostly benign although malignant lesions can also be seen[3].
Lipomas are benign tumors of mesenchymal origin. They are the second most common benign tumors in the small intestine and account for 10% of all benign gastrointestinal tumors and 5% of all gastrointestinal tumors. They are predominantly submucosal and protrude into the lumen. Occasionally, they arise in the serosa. Gastrointestinal lipomas are most commonly located in the colon (65% to 75%, especially on the right side), small bowel (20% to 25%) and occasionally in the foregut (< 5%)[6]. Lipomas are largely asymptomatic. The majority of presenting features are either intestinal obstruction or hemorrhage[7].
The clinical presentation is very non-specific which makes this a difficult condition to diagnose. Abdominal pain, nausea, diarrhea and bleeding per rectum are the common symptoms. Rarely, this can present with acute intestinal obstruction. The classical triad of abdominal pain, sausage shaped palpable mass and passage of red current jelly stools seen in children is rarely seen in adults[1,8].
Lipomas can be diagnosed through conventional endoscopy, capsule endoscopy, barium studies and, most importantly, CT scan. Typical endoscopic features are a smooth, yellowish surface with pedunculated or sessile base. Other endoscopic characteristics are the “cushion sign” and “naked fat sign”[6]. CT usually reveals a smooth, well-demarcated sausage-shaped mass. It may also reveal associated intussusception if present[9]. Capsule endoscopy and digital balloon endoscopy are newer means for diagnosing lipomas and are particularly helpful in cases involving small bowel lipomas[6]. Associated intussusception can be confirmed on contrast enema (“crescent sign”), CT and magnetic resonance imaging (MRI). Multislice CT facilitates the assessment of vascular supply to the affected bowel loop in cases of intussusception where impending ischemia is suspected[10].
In most cases of adult colonic intussusception, primary resection without reduction should be performed, particularly in those over 60 years of age due to a higher risk of malignancy. In cases of small bowel intussusception, reduction before resection should be carried out only if the pre-operative diagnosis of benign etiology is confirmed, the bowel is viable or it entails resecting massive lengths of small bowel with the risk of short gut syndrome as a sequela[11-13].
In conclusion, adult bowel intussusception is a rare but challenging condition for the surgeon. Preoperative diagnosis is usually missed or delayed because of nonspecific and often subacute symptoms. A high index of suspicion and appropriate investigations (USS, barium enema and CT scan) can result in prompt diagnosis. Gastrointestinal lipoma is a rare pathology and its most common complications are invagination and obstruction.
Due to the fact that adult intussusception is often frequently associated with malignant organic lesions, surgical intervention is necessary. Treatment usually requires formal resection of the involved bowel segment.
Peer reviewers: Ned Abraham, MBBS, FRACS, FRCS, PhD, Coffs Colorectal and Capsule Endoscopy Centre, University of New South Wales, 187 Rose Avenue, PO Box 2244, Coffs Harbour, NSW 2450, Australia; Thomas J Miner, MD, FACS, Department of Surgery, Rhode Island Hospital, 593 Eddy Street - APC 439, Providence, RI 02903, United States
S- Editor Wang JL L- Editor Roemmele A E- Editor Lin YP
| 3. | Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230-236. |
| 4. | Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531-535. |
| 5. | Orlando R. Intussusception in adults. Bowel obstruction: Differential diagnosis and clinical management. Philadelphia: WB Saunders Company 1990; . |
| 6. | Chou JW, Feng CL, Lai HC, Tsai CC, Chen SH, Hsu CH, Cheng KS, Peng CY, Chung PK. Obscure gastrointestinal bleeding caused by small bowel lipoma. Intern Med. 2008;47:1601-1603. |
| 7. | Balik AA, Ozturk G, Aydinli B, Alper F, Gumus H, Yildirgan MI, Basoglu M. Intussusception in adults. Acta Chir Belg. 2006;106:409-412. |
| 8. | Eisen LK, Cunningham JD, Aufses AH Jr. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390-395. |
| 9. | Michael A, Dourakis S, Papanikolaou I: Ileocaecal intussusception in an adult caused by a lipoma of the terminal ileum. Ann Gastroenterol. 2001;14:56-59. |
| 11. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. |
| 12. | Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36:18-21. |
| 13. | Khan MN, Agrawal A, Strauss P. Ileocolic Intussusception - A rare cause of acute intestinal obstruction in adults; Case report and literature review. World J Emerg Surg. 2008;3:26. |