Published online Apr 27, 2010. doi: 10.4240/wjgs.v2.i4.143
Revised: January 28, 2010
Accepted: February 4, 2010
Published online: April 27, 2010
Pancreaticobiliary maljunction is a congenital anomaly in which the junction between the pancreatic duct and the common bile duct is located outside the sphincter of Oddi. It is well known that pancreaticobiliary maljunction is frequently associated with carcinoma of the
biliary tract. We report a case of metachronous cancer of the gallbladder and pancreas associated with pancreaticobiliary maljunction and cystic dilatation of common bile duct in a 68-year-old Tunisian woman who underwent a cholecystectomy for acute cholecystitis. The pancreatic tumor was an adenosquamous carcinoma. Pancreaticobiliary maljunction allows for pancreatobiliary or biliopancreatic reflux which may induce biliary tract carcinoma. Few cases of multifocal cancer associated with this anomaly have been reported. The association with pancreatic carcinoma remains rare. Close attention should be given to both the biliary tract system and pancreas during the long-term follow-up of patients with pancreaticobiliary maljunction, especially after they have undergone a choledochojejunostomy.
- Citation: Lahmar A, Abid SB, Arfa MN, Bayar R, Khalfallah MT, Mzabi-Regaya S. Metachronous cancer of gallbladder and pancreas with pancreatobiliary maljunction. World J Gastrointest Surg 2010; 2(4): 143-146
- URL: https://www.wjgnet.com/1948-9366/full/v2/i4/143.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v2.i4.143
It is well known that pancreaticobiliary maljunction is frequently associated with carcinoma of the biliary tract[1]. However, its association with adenocarcinoma of the pancreas remains rare. Furthermore, metachronous cancer of the gallbladder and pancreas associated with pancreaticobiliary maljunction and cystic dilatation of common bile duct has never, to our knowledge, been reported. Pancreaticobiliary maljunction is a congenital anomaly in which the junction between the pancreatic duct and the common bile duct is located outside the sphincter of Oddi. This anomaly leads to two-way regurgitation of pancreatic juice into the biliary tract or bile into the pancreatic duct because of the lack of a sphincter mechanism. Here we report a case of metachronous cancer of the gallbladder and pancreas associated with pancreaticobiliary maljunction and cystic dilatation of the common bile duct. To date, only four cases of metachronous double cancer of the pancreas and gallbladder associated with pancreaticobiliary maljunction without cystic dilatation of common bile duct have been reported.
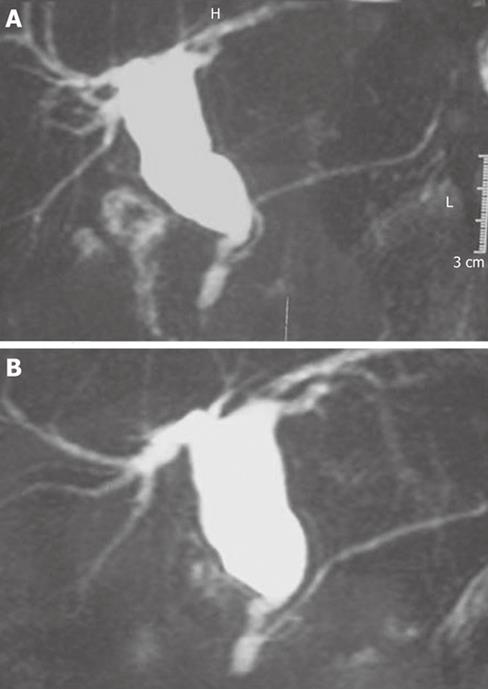
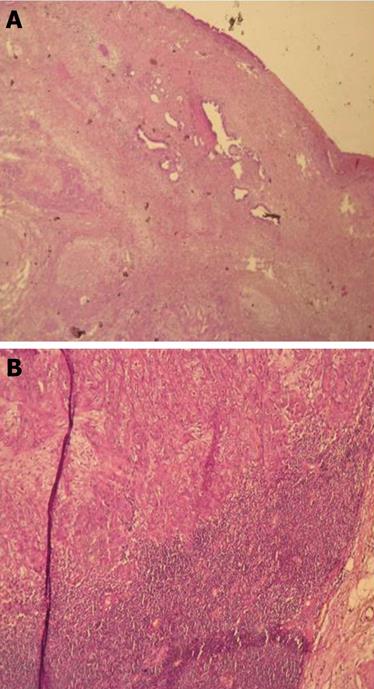
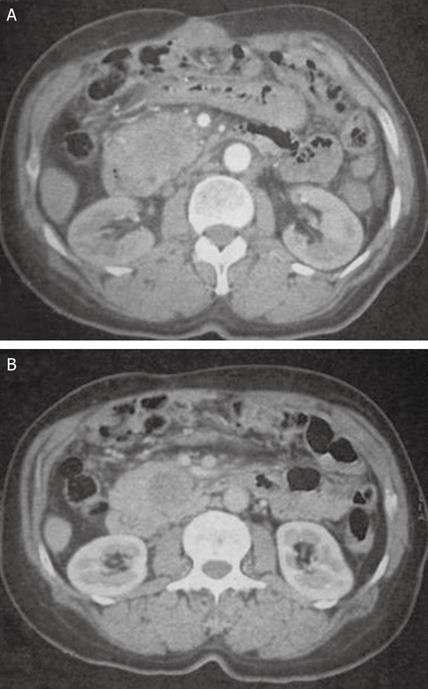
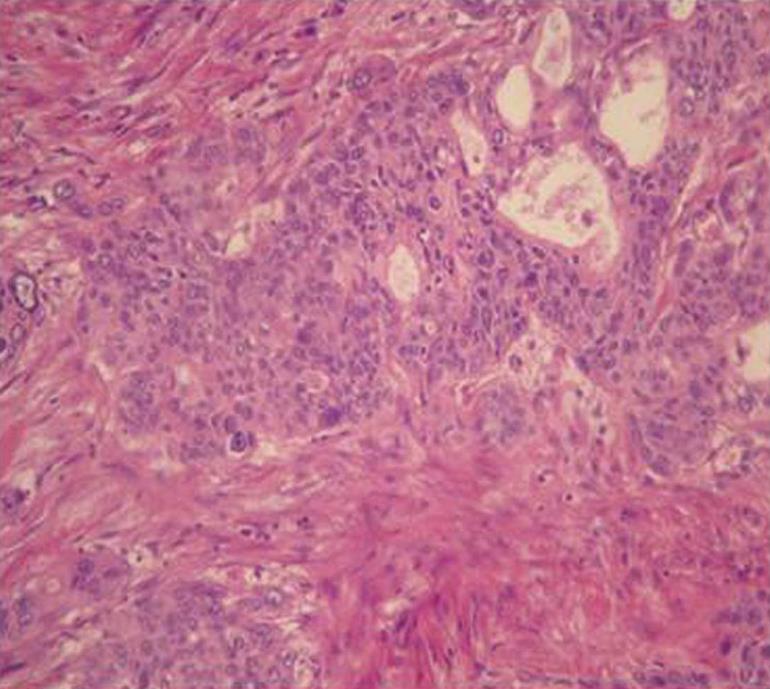
In April 2004, a 68-year-old Tunisian woman underwent a cholecystectomy for acute cholecystitis. The histological examination revealed moderately differentiated adenocarcinoma of gallbladder classified pT2N1M0. She was referred to our department. On the admission, physical examination and hepatic test were normal. Ultrasonography and computed tomography (CT) showed a bile duct dilatation. Magnetic resonance imaging (MRI) showed a cystic dilatation of common bile duct and revealed that the pancreatic duct was joined to the bile duct 22 mm above the papilla of Vater. The cystic dilatation of the common bile duct was classified as Type I of Todani and the pancreaticobiliary maljunction as variety I of Kumura (Figure 1A and B). The patient underwent a bisegmentectomy IV-V, wide lymph node dissection and resection of all the pathological common bile duct. The common bile duct was transected in the intra pancreatic part which is important to reduce the risk of recurrence in the intra pancreatic part of the bile duct. The post operative course was complicated by an intra peritoneal abscess treated by percutaneous drainage and antibiotics. Histological examination revealed moderately differentiated adenocarcinoma invading the cystic dilatation of common bile duct and lymph nodes (Figure 2A and B). She underwent a postoperative chemotherapy (Cisplatine, 5FU). In January 2008, the serum carcinoembryonic antigen level was 125 ng/mL (Nl = 5 ng/mL). On admission, physical examination was unremarkable. The serum CA 19-9 level was 965 U/l, alkaline phosphatase was 90 IU/L and γ-glutamyl transpeptidase was 23 IU/L. Abdominal CT revealed a low-density head pancreatic tumor measuring 40 mm in maximum diameter (Figure 3). In February 2009, she underwent a pancreatoduodenectomy with regional lymph node dissection without resection of the hepatico-jejunostomy. The final histological diagnosis was adenosquamous carcinoma of pancreas with two malignant components (one glandular and the other squamous) without regional lymph node metastasis (pT2N0M0) (Figure 4). The patient’s postoperative course was complicated by pancreatic fistula treated by percutaneous drainage and antibiotics. She was discharged about 1 mo after the surgery and is still alive without any evidence of recurrence 1 year after the procedure.
Pancreaticobiliary maljunction is a congenital anomaly in which the junction between the pancreatic duct and the common bile duct is located outside the sphincter of Oddi; it is an uncommon anomaly, with an incidence of 3.2% in patients undergoing ERCP or operative cholangiopancreatography[2]. This anomaly allows pancreatobiliary or biliopancreatic reflux. Refluxed proteolytic pancreatic enzymes are activated in the biliary tract and may induce biliary tract carcinoma.
After a meal, the bile duct pressure is raised by contraction of the gallbladder and regurgitation occurs in the opposite direction with bile flowing into the pancreatic duct. The reflux of bile may activate pancreatic enzymes which may cause chronic inflammation and metaplastic epithelial change in the pancreatic duct and pancreatic cancer may eventually develop[3]. In our patient, the cystic dilatation of the common bile duct was classified as Type I of Todani and the pancreaticobiliary maljunction as variety I of Kimura; this variety account for only 5% of pancreaticobiliary maljunction[2]. The pancreatic cancer was found 4 years after the resection of her gallbladder and excision of the cystic dilatation of the common bile duct. Therefore, it seems that the inflammatory changes in the pancreas had been present for many years with the tendency for carcinogenesis[3-5]. There have been 27 reported cases of pancreatic cancer in patients who had pancreaticobiliary maljunction. Multifocal cancer of the biliary tree and pancreas associated with pancreaticobiliary maljunction has been reported in 7 patients (two cases were triple cancer of the gallbladder, the bile duct and the pancreas)[4-6] and six of them were women. In the seven patients, the cancer of the gallbladder occurred previously or synchronously with the pancreatic cancer[7]. Gallbladder cancer was more frequent than bile duct cancer[7]. Three patients had bile duct dilatation and none presented a choledochal cyst. Our patient had double cancer of gallbladder and pancreas associated with a choledochal cyst.
The histological diagnosis on examination of the surgical specimen was adenosquamous carcinoma which has two associated carcinomatous components: glandular and squamous. It is rare, accounting for 3%-4% of all pancreatic carcinoma[8]. Adenosquamous carcinoma of the pancreas has a poor prognosis because of systemic metastases in the liver and peritoneal dissemination. In addition, tumor recurrence occurs frequently early after tumor resection[8].
Pancreatic carcinoma associated with pancreaticobiliary maljunction is rare. The relationship between pancreatic carcinoma and pancreaticobiliary maljunction is clear. Therefore, close attention should be paid to both the biliary tract system and the pancreas during the long-term follow-up of patients with pancreaticobiliary maljunction following a choledochojejunostomy.
Peer reviewer: Giorgio Ercolani, MD, PhD, Department of Surgery and Transplantation, Sant’Orsola-Malpighi Hospital, Via Massarenti 9, Bologna 40138, Italy
S- Editor Li LF L- Editor Roemmele A E- Editor Yang C
| 1. | Seki M, Yanagisawa A, Ninomiya E, Ninomiya Y, Ohta H, Saiura A, Yamamoto J, Yamaguchi T, Aruga A, Yamada K. Clinicopathology of pancreaticobiliary maljunction: relationship between alterations in background biliary epithelium and neoplastic development. J Hepatobiliary Pancreat Surg. 2005;12:254-262. |
| 2. | Sugiyama M, Atomi Y, Kuroda A. Pancreatic disorders associated with anomalous pancreaticobiliary junction. Surgery. 1999;126:492-497. |
| 3. | Todani T, Watanabe Y, Urushihara N, Noda T, Morotomi Y. Choledochal cyst, pancreaticobiliary malunion, and cancer. J Hepatobiliary Pancreat Surg. 1994;1:247–251. |
| 4. | Ueda N, Nagakawa T, Ohta T, Tugawa K, Takeda T, Kadoya N. A case of carcinomas of the gallbladder, common bile duct and pancreas associated with anomalous arrangement of the pancreaticobiliary ductal system. Nippon Rinsyou Geka Gakkai Zasshi. 1988;49:2198–2205. |
| 5. | Kunimura T, Morohoshi T, Kanda M, Kuroki T, Umezawa T, Asanuma K. Anomalous arrangement of pancreatobiliary ductal system associated with gallbladder and pancreatic cancer. Tando. 1990;4:68–74. |
| 6. | Morohoshi T, Kunimura T, Kanda M, Takahashi H, Yagi H, Shimizu K, Nakayoshi A, Asanuma K. Multiple carcinomata associated with anomalous arrangement of the biliary and pancreatic duct system. A report of two cases with a literature survey. Acta Pathol Jpn. 1990;40:755-763. |
| 7. | Minami Y, Hasuike Y, Takeda Y, Tsujinaka T. Metachronous double cancer of the gallbladder and pancreas associated with pancreaticobiliary maljunction. J Hepatobiliary Pancreat Surg. 2008;15:330-333. |
| 8. | Okabayashi T, Hanazaki K. Surgical outcome of adenosquamous carcinoma of the pancreas. World J Gastroenterol. 2008;14:6765-6770. |