INTRODUCTION
Gallbladder stones, or cholelithiasis, are a common biliary tract disease with significant clinical and economic burdens. These stones have multifactorial etiologies, including metabolic, genetic, and environmental factors. Recent evidence highlights an emerging link between hematological disorders, particularly those involving hemolysis or impaired erythropoiesis, and the formation of gallbladder stones, especially pigment stones. Hematological disorders, particularly those involving chronic hemolysis, are associated with an increased risk of gallstone formation due to elevated bilirubin levels resulting from the breakdown of red blood cells. For instance, studies have shown that patients with sickle cell disease (SCD) and thalassemia have a higher prevalence of gallstones compared to the general population. A study in Akre City found a 12% prevalence of gallstones in patients with SCD and sickle β-thalassemia, compared to 3% in healthy controls[1]. This review seeks to explore the mechanisms underlying this association (Figure 1), the clinical implications for affected patients, and potential avenues for future research. By understanding this interplay, clinicians and researchers can improve diagnostic, preventive, and therapeutic strategies. While several studies have examined the link between hematological disorders and gallstones, our review offers new insights by incorporating the latest research on the underlying pathophysiological mechanisms and providing updated management strategies for these patient populations.
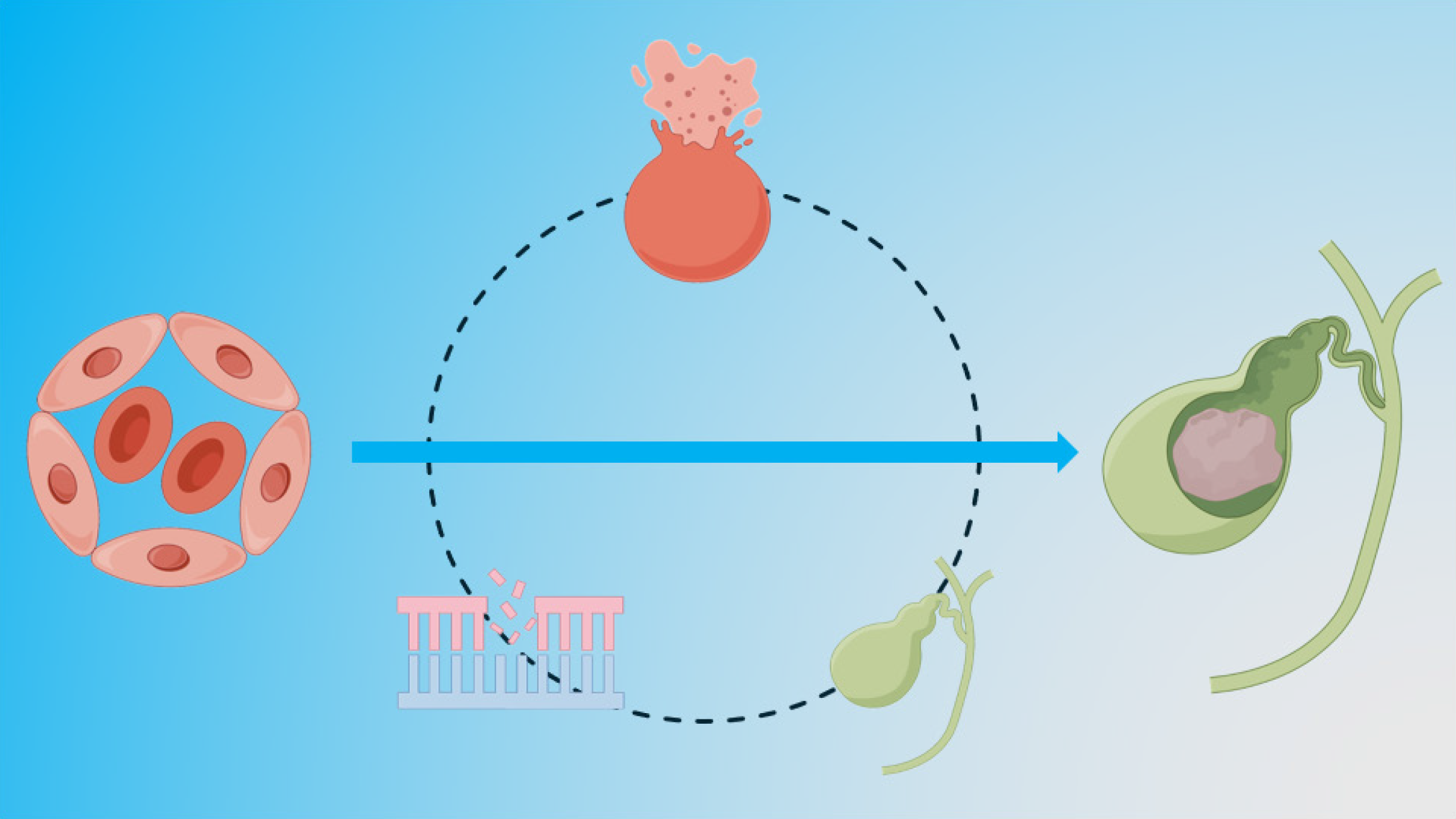
Figure 1 The key pathophysiological mechanisms linking hematological disorders to pigment gallstone formation.
On the left side, hematological conditions such as sickle cell disease, thalassemia, and hereditary spherocytosis are shown, with arrows pointing to the excessive hemolysis and genetic mutations (e.g., uridine diphosphate glucuronosyl transferase 1A1 gene mutation) that contribute to increased bilirubin production. This excess bilirubin is released into the bile, where it precipitates as calcium bilirubinate, forming pigment stones in the gallbladder. On the right side, the impaired gallbladder motility and altered bile composition (such as in conditions like iron deficiency anemia) are highlighted as additional contributing factors to stone formation.
TYPES OF GALLBLADDER STONES
Gallbladder stones, or gallstones, are solid particles that form in the gallbladder and are primarily classified into three main types: Cholesterol stones, pigment stones, and mixed stones. Each type has distinct characteristics based on their chemical composition, formation mechanisms, and clinical implications. Cholesterol stones are predominantly composed of cholesterol monohydrate crystals and are the most common type, particularly in Western populations[2]. They form due to the supersaturation of cholesterol in bile, often associated with metabolic conditions such as obesity, dyslipidemia, and type 2 diabetes[3]. These stones are more prevalent in females, especially those aged 30 to 50, and are linked to higher body mass index[4]. Typically yellow-green, cholesterol stones can vary in size from small grains to large stones[5].
Pigment stones are divided into black and brown pigment stones, each with distinct formation processes. Black pigment stones are composed mainly of calcium bilirubinate and other calcium salts and are commonly associated with hemolysis or liver cirrhosis[6]. Brown pigment stones, on the other hand, are linked to bacterial infections and parasitic infestations and contain calcium bilirubinate and fatty acids[2,6]. Pigment stones are more common in males aged 40 to 60 and are often associated with chronic liver disease[4]. They are typically smaller and darker than cholesterol stones, with a brittle texture[5].
Mixed stones contain a combination of cholesterol and other components such as calcium carbonate or calcium phosphate[4,7]. These stones form when cholesterol deposits are combined with bile pigments or calcium salts, often due to bile stasis or infection[3]. Mixed stones exhibit varied appearances and textures, reflecting their composite nature[8]. While the primary focus is on the three main types of gallstones, other rare types also exist, such as calcium carbonate stones and protein or cystine stones. Calcium carbonate stones include mud-like and coralliform types, with distinct characteristics: Mud-like stones are earthy yellow or brown with a soft texture, while coralliform stones are black and extremely hard[9]. These rare stones are associated with conditions like cystic duct obstruction and Clonorchis sinensis infection[9]. Phosphate stones, composed of calcium phosphate, and protein or cystine stones, linked to genetic disorders, are even rarer[4]. Understanding these diverse pathways can enhance the overall approach to managing gallstone disease across various patient populations.
HEMATOLOGICAL DISORDERS LINKED TO GALLBLADDER STONES
Hematological disorders such as hemolytic anemias, disorders affecting erythropoiesis, and myeloproliferative disorders have been implicated in the formation of gallbladder stones. Hemolytic disorders like sickle cell anemia, hereditary spherocytosis, and thalassemias lead to chronic hemolysis, significantly elevating unconjugated bilirubin levels, which predisposes patients to pigment stone formation. SCD, a major hemoglobinopathy, has a high prevalence of gallstones, reported at approximately 25.3% among patients[10]. Chronic hemolysis in SCD leads to elevated bilirubin levels, contributing to pigment stone formation[11]. Genetic factors, such as uridine diphosphate glucuronosyltransferase-1A1 (UGT1A1) promoter polymorphism, further increase the risk of cholelithiasis in SCD patients[10].
In thalassemia, particularly β-thalassemia, patients are at increased risk for gallstones due to chronic hemolysis and resultant hyperbilirubinemia. Co-inheritance of genetic mutations, such as those affecting UGT1A1, exacerbates this risk. Similarly, hereditary spherocytosis is characterized by the presence of spherical red blood cells that are prone to hemolysis, leading to increased bilirubin production and a higher incidence of gallstones[12]. The interaction with conditions like Gilbert syndrome can further elevate bilirubin levels, enhancing stone formation[13].
The mechanisms of stone formation in these conditions include bilirubin overproduction, where excessive breakdown of red blood cells leads to increased bilirubin excretion into the bile. This bilirubin can precipitate as calcium bilirubinate, forming pigment stones. Genetic factors, such as mutations in the UGT1A1 gene, impair bilirubin conjugation, further increasing gallstone risk. Additionally, the prevalence of gallstones increases with age and the severity of hemolytic disorders, as seen in SCD, where older patients and those with more severe hemolysis are more likely to develop stones[11].
While hemolytic disorders are a primary focus, other conditions such as iron deficiency anemia have also been linked to gallstone formation. Iron deficiency can lead to bile supersaturation and stone formation, suggesting a complex interplay between different hematological conditions and gallstone pathogenesis[14]. Additionally, factors like liver cirrhosis and post-surgical states can contribute to gallstone formation through mechanisms such as altered bile flow and increased bilirubin production. Understanding these diverse influences is crucial for managing and preventing gallstone disease in patients with hematological disorders.
MECHANISMS LINKING HEMATOLOGICAL DISORDERS AND GALLBLADDER STONES
The pathophysiological mechanisms linking hematological disorders to gallstone formation primarily involve hemolysis and bilirubin metabolism[1]. In conditions such as SCD, thalassemia, and hereditary spherocytosis, chronic hemolysis leads to an overproduction of unconjugated bilirubin[15]. This bilirubin is excreted into bile, where it can precipitate as calcium bilirubinate, forming pigment stones[16].
In addition to hemolysis, genetic factors such as mutations in the UGT1A1 gene (e.g., in Gilbert syndrome) impair bilirubin conjugation, further increasing bilirubin levels and promoting stone formation. Oxidative stress and free radical production in the gallbladder can also contribute to stone formation by altering bile composition and viscosity[16].
These mechanisms are compounded by factors such as impaired gallbladder motility seen in conditions like iron deficiency anemia, which can lead to bile stasis and increased risk of stone formation. Treatment-related factors, such as repeated blood transfusions, can lead to iron overload, altering bile metabolism, while chemotherapy affects bile composition and gallbladder function, indirectly contributing to stone formation[11]. The interaction of these factors creates a complex environment that promotes the development of gallstones in individuals with hematological disorders.
CLINICAL IMPLICATIONS
Patients with hematological disorders and gallbladder stones present unique diagnostic and therapeutic challenges. Diagnosing gallstones in this population is often complicated by overlapping symptoms and comorbidities. Imaging modalities such as ultrasound and computed tomography scans are essential for detecting gallstones, while laboratory tests assessing bilirubin levels and liver function can provide additional diagnostic insights. Regular ultrasound examinations are recommended for patients with inherited hemolytic anemias, such as thalassemia and SCD, to detect gallstones early[17]. In patients with SCD, distinguishing between abdominal pain due to gallstones and sickle cell crises is challenging. Therefore, gallbladder disease should be considered in differential diagnoses for abdominal pain in these patients. For patients with hematologic malignancies, acute acalculous cholecystitis can be diagnosed using specific ultrasound criteria, such as gallbladder wall thickening and pericholecystic fluid, which help identify at-risk patients[18].
Management strategies vary depending on the patient’s condition. Non-surgical approaches, such as the use of ursodeoxycholic acid, may be attempted in select cases, although their effectiveness is limited for pigment stones. Laparoscopic cholecystectomy remains the standard treatment for symptomatic gallstones. In patients with SCD, elective cholecystectomy is recommended to prevent biliary complications; however, the risk of vaso-occlusive crises during the perioperative period necessitates careful preoperative planning, including possible prophylactic transfusions[19]. Endoscopic retrograde cholangiopancreatography may be performed prior to cholecystectomy to remove stones from the bile duct in cases of choledocholithiasis. Although effective, this procedure carries risks such as post-endoscopic retrograde cholangiopancreatography pancreatitis[20]. For patients with hematologic malignancies undergoing cholecystectomy, intraoperative transfusions may be necessary, particularly for those with a history of hematopoietic cell transplantation or immunosuppressive therapy, but these transfusions can increase postoperative complications and hospital stay duration[21]. Risk stratification is crucial, as identifying high-risk patients - such as those with chronic hemolytic anemia or multiple transfusions - can enable timely interventions. Multidisciplinary collaboration between hematologists, gastroenterologists, and surgeons is essential to optimize patient outcomes.
KNOWLEDGE GAPS AND FUTURE DIRECTIONS
Despite advancements in understanding, several gaps remain in the study of the association between hematological disorders and gallbladder stones. There is a need for more detailed studies on the lipid profiles and hematological changes in patients with gallstones related to hemolytic anemia, as current studies indicate distinct lipid profiles, such as lower total cholesterol and high-density lipoprotein levels compared to the general population with gallstones[22,23]. Additionally, the role of genetic mutations, such as those in the UGT1A1 and ATP-binding cassette transporters G8 genes, and their interaction with hemolytic disorders like thalassemia and sickle cell anemia, requires further exploration. Longitudinal studies are needed to track gallstone development in patients with hematological disorders and to identify biomarkers for early detection and risk prediction. Experimental models focusing on the biochemical processes, such as the precipitation of bilirubin monoconjugate in bile, can also provide deeper insights into the pathogenesis of pigment gallstones[24].
Future research should include comparative studies between patients with and without genetic mutations to better understand genetic predispositions to gallstone formation. Additionally, investigating the impact of risk factors such as blood transfusion frequency, hydroxyurea intake, and splenomegaly on gallstone formation could help refine screening strategies[25]. Clinical trials assessing the effectiveness of interventions like dietary modifications and pharmacological treatments in reducing gallstone risk in hemolytic disorders are also warranted[22,23]. Addressing these gaps could significantly enhance the understanding and management of gallbladder stones in this patient population.
LIMITATION
One limitation of this manuscript is that the studies included vary in design, sample size, and patient populations. Furthermore, the absence of longitudinal studies on the long-term impact of hematological disorders on gallstone formation limits our understanding of the chronicity and progression of these conditions.
CONCLUSION
In conclusion, our review highlights the complex relationship between hematological disorders and gallbladder stone formation. Hemolysis, genetic factors, and impaired bilirubin metabolism play key roles in promoting the formation of pigment stones in conditions such as SCD, thalassemia, and hereditary spherocytosis. These findings underscore the importance of early diagnosis, regular screening, and tailored management strategies for patients with hematological disorders at risk for gallstones. Future research should focus on elucidating the precise molecular mechanisms involved, exploring the role of genetic mutations, and developing better screening tools to predict gallstone risk. Additionally, studies on the effectiveness of preventive measures, including pharmacological treatments and dietary interventions, will be crucial in improving patient outcomes.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade B
Novelty: Grade C, Grade C
Creativity or Innovation: Grade C, Grade C
Scientific Significance: Grade B, Grade C
P-Reviewer: Abdullah OO; Oviedo RJ S-Editor: Wang JJ L-Editor: A P-Editor: Wang WB