Published online May 27, 2024. doi: 10.4240/wjgs.v16.i5.1336
Revised: March 14, 2024
Accepted: April 15, 2024
Published online: May 27, 2024
Processing time: 118 Days and 19.2 Hours
Magnetic anchor technique (MAT) has been applied in laparoscopic cholecy
To evaluate the feasibility of the MAT in laparoscopic left lateral segment liver resection.
Retrospective analysis was conducted on the clinical data of eight patients who underwent laparoscopic left lateral segment liver resection assisted by MAT in our department from July 2020 to November 2021. The Y-Z magnetic anchor de
All eight patients underwent a MAT-assisted laparoscopic left lateral segment liver resection, including three patients undertaking conventional 5-port and five patients having a transumbilical single-port operation. The mean operation time was 138 ± 34.32 min (range 95-185 min) and the mean intraoperative blood loss was 123 ± 88.60 mL (range 20-300 mL). No adverse events occurred during the operation. The Y-Z MADs showed good workability and maneuverability in both tissue and organ exposure. In particular, the operators did not experience either a “chopstick” or “sword-fight” effect in the single-port laparoscopic operation.
The results show that the MAT is safe and feasible for laparoscopic left lateral segment liver resection, especially, exhibits its unique abettance for transumbilical single-port laparoscopic left lateral segment liver resection.
Core Tip: Magnetic anchor technique (MAT) can be used to assist in exposing tissues or organs during laparoscopic surgery, thereby effectively reducing the number of trocars and eliminating interference between laparoscopic instruments. This study retrospectively analyzed eight patients who underwent laparoscopic left lateral lobectomy using Y-Z magnetic anchor devices. The results showed that MAT is safe and feasible for transumbilical single-port laparoscopic left lateral hepa
- Citation: Zhang MM, Bai JG, Zhang D, Tao J, Geng ZM, Li ZQ, Ren YX, Zhang YH, Lyu Y, Yan XP. Clinical feasibility of laparoscopic left lateral segment liver resection with magnetic anchor technique: The first clinical study from China. World J Gastrointest Surg 2024; 16(5): 1336-1343
- URL: https://www.wjgnet.com/1948-9366/full/v16/i5/1336.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i5.1336
Since the laparoscopic resection of benign liver tumors was first reported in 1991[1], laparoscopic liver resection has progressively developed and its safety and feasibility have gradually increased[2,3]. Laparoscopic hepatectomy has become a common operation in hepatobiliary surgery with the advantages being less trauma and faster recovery[4]. The unique anatomical structure of the left lateral hepatic lobe makes laparoscopic left lateral segment liver resection an earlier and more widely used laparoscopic hepatectomy. As a result, it has thus been considered to be the first “gold standard” laparoscopic procedure, replacing open left lateral lobectomy for liver resection[5-7].
Transumbilical single-port laparoscopic left lateral lobectomy has been reported[8-10]. However, the “chopstick” and “sword-fight” effects caused by the single-port not only confines the intraoperative maneuverability of the laparoscope instruments[11], but also hinders the interplay of traction and counter-traction between the instruments for effectively stretching and exposing the tissues and organs in the single-port laparoscopic operation. Taking this into account, in addition to the demand for laparoscopic surgeons to continuously improve their single-port operating skills, there is a need for developing better instruments for single-port laparoscopic operations.
The magnetic anchor technique (MAT) uses magnetic devices to perform non-contact spatial anchoring between the anchor magnet and the target magnet[12], which can be used to assist tissue or organ exposure in laparoscopic surgery[13], thereby feasibly reducing the number of inserted trocars, and eliminating the reciprocal interferences between la
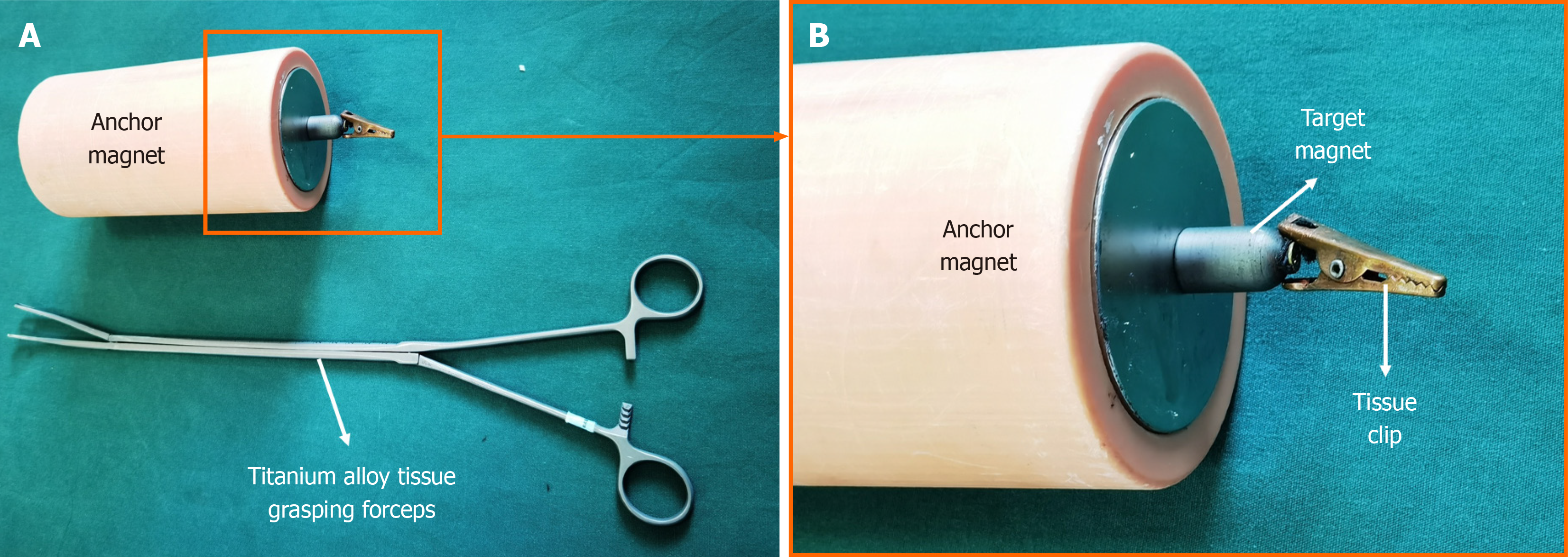
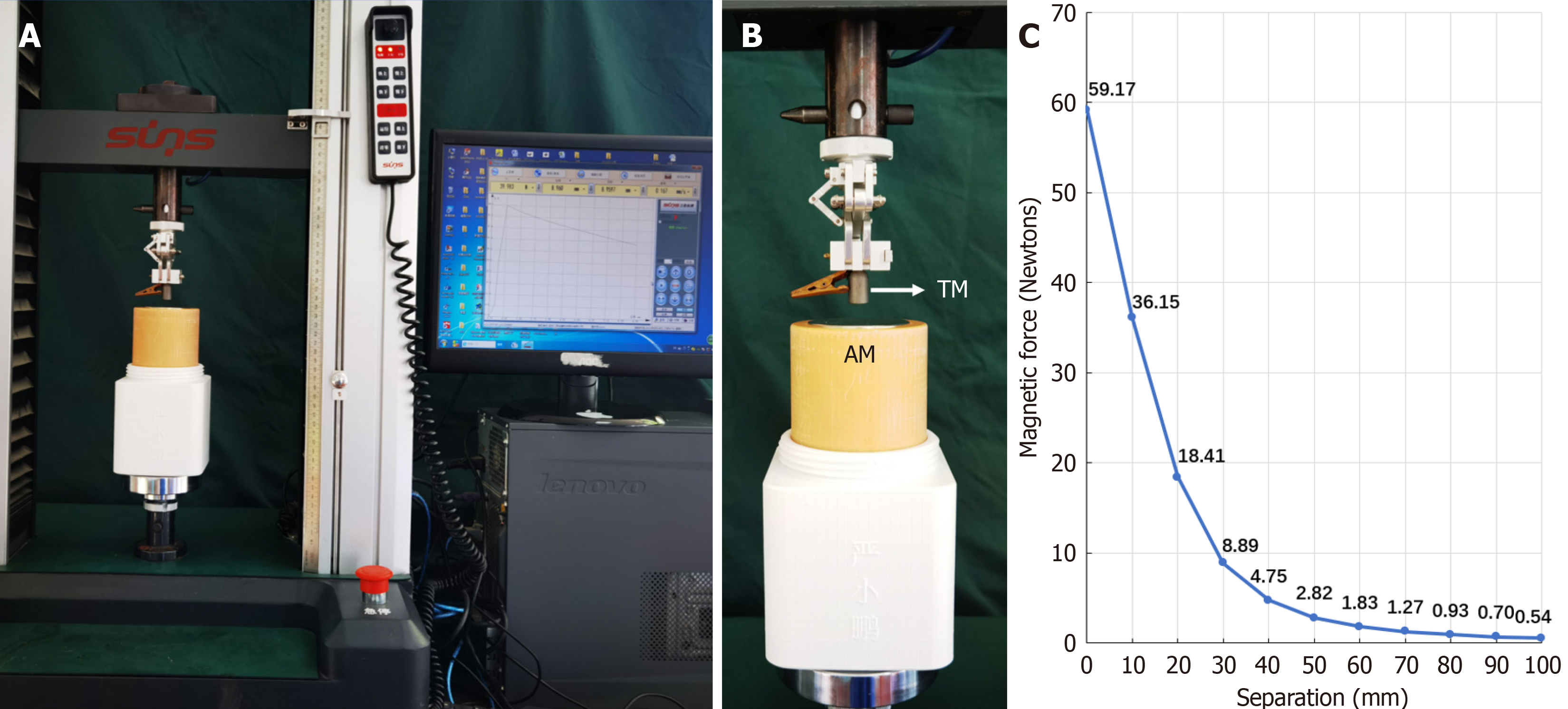
The Y-Z MADs was designed by the authors (Yan XP and Zhang MM) and consists of an anchor magnet and a magnetic grasping apparatus. The auxiliary operation instrument is a titanium alloy tissue grasping forceps. The anchor magnet is a cylindrical magnet with a diameter of 60 mm, a height of 160 mm, and a mass of 2242 g (Figure 1A), made of N50 sintered-type neodymium-iron-boron magnetized with axial saturation with 7500 gausses of the magnetic induction in
This single-center, retrospective clinical study was conducted at an academic medical center and approved by its ethics committee (No. 2018-W18). We conducted this study in accordance with the Declaration of Helsinki, and all methods were performed in accordance with the relevant guidelines and regulations. All patients or their authorized legal representatives signed the informed consent form for the use of MAT in their operations.
The included patients conformed to the following criteria: (1) A preoperative computerized tomography scan or magnetic resonance imaging of the upper abdomen gave a clear diagnosis, and if the malignant lesion was unveiled, it must be confined to the left lateral lobe of the liver; (2) Informed consent had been signed by the patient or their family members; and (3) Body mass index (BMI) should be no more than 30 kg/m2. In addition, the patients were excluded from this study if they: (1) Presented with a history of upper abdominal surgery or severe intra-abdominal adhesions; (2) Were found to have any metastatic lesion, either intrahepatic or extrahepatic; (3) Had a cardiac pacemaker implanted; (4) Had a BMI over 30 kg/m2; (5) Suffered severe cardiopulmonary diseases and were not able to tolerate general anesthesia during surgery and/or patients with pneumoperitoneum; and (6) Were considered inappropriate by the investigator for other reasons.
The clinical data of eight patients who underwent magnetic anchor-assisted laparoscopic left lateral hepatic lobectomy were retrospectively analyzed. Demographically, two patients were female and six were male in this study, aged between 23 and 75 years, with a median age of 49.5 years. Their BMI ranged from 19.26 to 26.30 kg/m2, with a median of 23.19 kg/m2. Diagnostically, three of the patients had hepatic hemangioma, one had primary liver cancer, two had primary liver cancer complicated with gallbladder stones, one had liver metastases, and one had focal hepatic steatosis.
Among the eight patients in this study, the first three underwent 5-port laparoscopic operations with the purpose of developing the stepwise procedure for the MAT-assisted laparoscopic left lateral hepatic lobectomy. Afterwards, based upon the practical experience gained from the first three patients, we performed transumbilical single-port laparoscopic left lateral hepatic lobectomy on the remaining five patients.
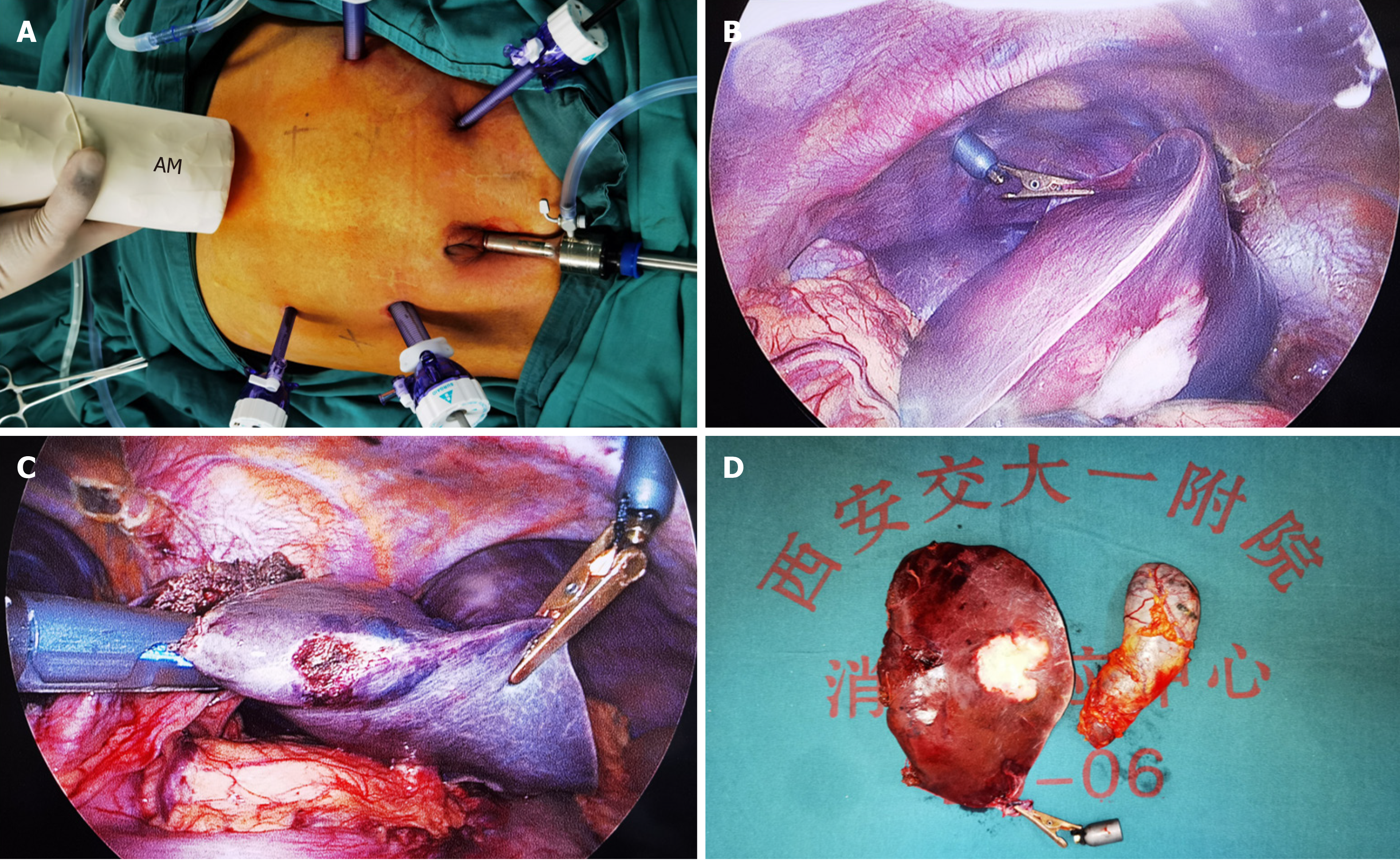
The MAT-assisted 5-port left lateral hepatic lobectomy was started once general anesthesia took effect. After the patients were placed in a lithotomy position with slight reverse trendelenburg tilting to left, five trocars were placed in the abdominal wall as shown in Figure 3A, and subsequently, the pneumoperitoneum was established with the pressure maintained at the level of 12 mmHg. The magnetic grasping forceps were delivered into the peritoneal cavity through the 12 mm port using the titanium alloy tissue grasping forceps, and then clamped on the edge of the left lateral lobe of the liver. The anchor magnet was then placed on the abdominal wall to attract the target magnet so that the liver could be pulled up following the movement of the anchor magnet (Figure 3B). Once this was completed, the coronary ligament and the left deltoid ligament were disconnected from their attachment to peritoneal wall, and the liver capsule and su
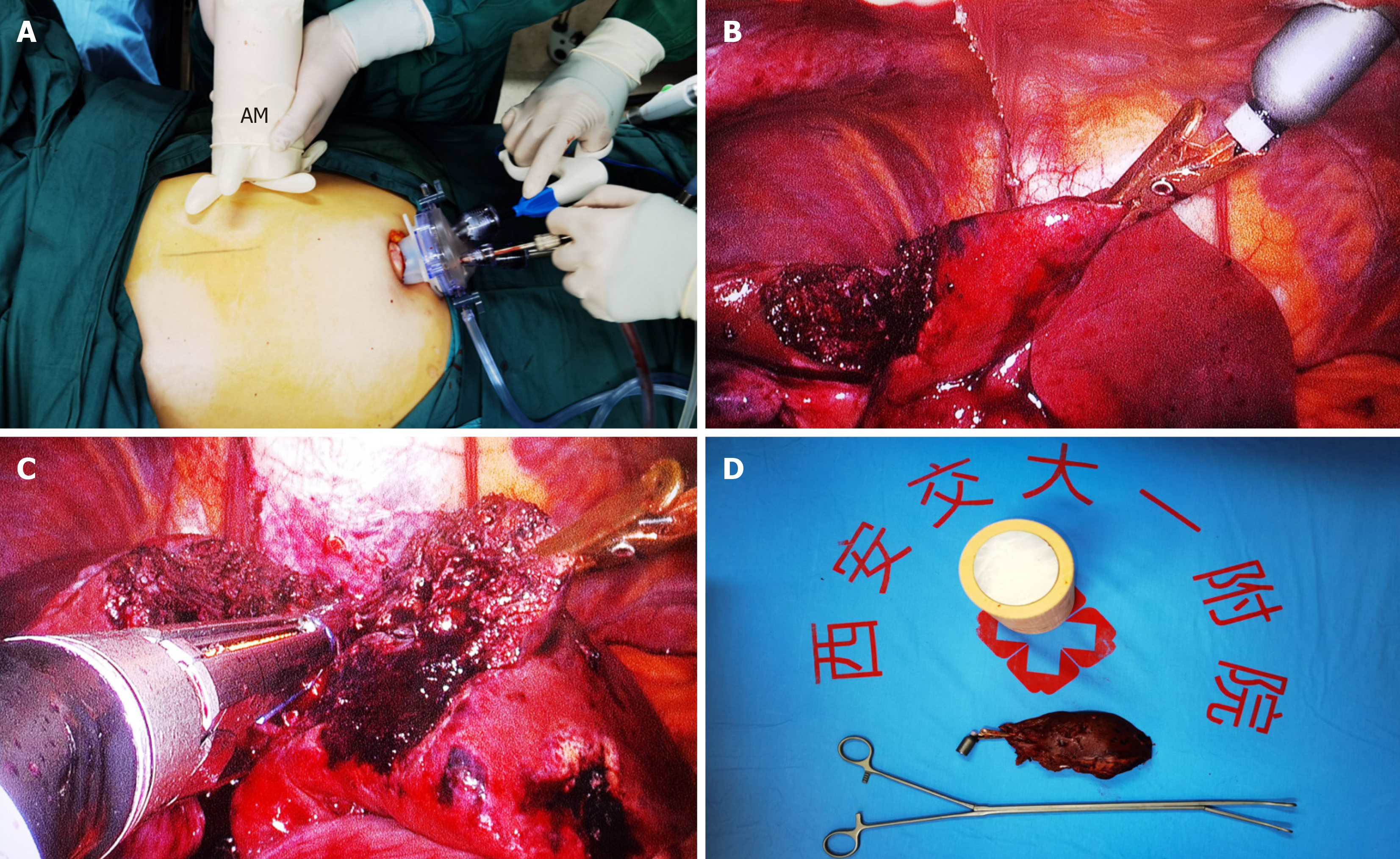
For the MAT-assisted transumbilical single-port laparoscopic left lateral hepatic lobectomy, after a 4 cm arcuate incision was first made under the umbilicus as shown in Figure 4A, a single-port (Hangzhou Kangji Medical Instrument Co., Ltd.) was inserted, and the pneumoperitoneum was established with a pressure of 12 mmHg. After laparoscopically surveying the abdominal cavity, the magnetic grasping apparatus was introduced into the cavity through the single-port to clamp the edge of the left lateral lobe of the liver. At the same time, the anchoring magnet was placed outside the right upper abdominal wall of the patient to attract the target magnet to the magnetic grasping apparatus. After maneuvering the pulling direction and strength to create ample exposure to the operating field, the falciform ligament, left coronary ligament, and left deltoid ligament were sacrificed by ultrasonic scalpel, and the “two-step two-nail” technique was adopted to sequentially remove segment II and part of segment III of the left lateral lobe of the liver (Figure 4B and C). Following this, the anchoring magnet was removed from the abdominal wall, both the magnetic grasping apparatus and the bagged resected liver were taken out through the single-port, and the indwelling abdominal drainage tube in the liver section was led out of the body from the umbilical incision and fixed (Figure 4D). The operation was then complete. The surgical procedure of patient 8 is shown in the Video.
Study parameter indicators included operating time, intraoperative blood loss, damage to the surrounding organ, failure of the magnetic anchoring device, the operating experience of the operator and assistants, postoperative incision pain score, postoperative hospital stay, perioperative complications, and other indicators. SPSS 20.0 software was used for statistical analysis. The measurement data of normal distribution were expressed as (mean ± SD), while the measurement data of skewed distribution were expressed as a median.
MAT-assisted laparoscopic left lateral hepatic lobectomy was successfully performed on all eight patients without the conversion to an open procedure or use of the Pringle maneuver. Five patients had successful single-port operations without the addition of any trocars in the abdominal wall. Intraoperatively, the Y-Z MADs made the surgical field ex
| Patient no. | Gender | Age (yr) | BMI (kg/m2) | Diagnosis | Child-Pugh scoring | Extent of resection | Tumor size | Number of ports | Operative (min) | Bleeding volume (mL) | Pain score1 | Drainage tube retention time (d) | Postoperative hospital stay (d) |
| 1 | Male | 61 | 26.30 | Primary liver cancer | 5 | Left lateral lobe | 45 mm × 45 mm × 32 mm | 5 | 100 | 100 | 2/3/3 | 5 | 5 |
| 2 | Male | 51 | 21.67 | Primary liver cancer, gallstone | 5 | Left lateral lobe + gallbladder | 40 mm × 35 mm × 40 mm | 5 | 170 | 110 | 3/3/3 | 4 | 5 |
| 3 | Female | 42 | 19.26 | Hepatic hemangioma | 6 | S2 + partial S3 | 82 mm × 60 mm × 45 mm | 5 | 110 | 100 | 3/3/2 | 4 | 6 |
| 4 | Female | 23 | 21.88 | Focal hepatic steatosis | 5 | Left lateral lobe | 25 mm × 23 mm × 20 mm | 1 | 185 | 300 | 1/1/2 | 0 | 4 |
| 5 | Male | 48 | 24.91 | Hepatic hemangioma | 5 | Left lateral lobe | 62 mm × 50 mm × 43 mm | 1 | 150 | 100 | 2/2/2 | 2 | 5 |
| 6 | Male | 75 | 24.24 | Liver metastases | 5 | S2 + partial S3 | 55 mm × 45 mm × 60 mm | 1 | 165 | 200 | 2/2/2 | 5 | 6 |
| 7 | Male | 37 | 22.65 | Hepatic hemangioma | 5 | Left lateral lobe | 72 mm × 55 mm × 45 mm | 1 | 130 | 50 | 1/2/2 | 3 | 3 |
| 8 | Male | 57 | 23.72 | Primary liver cancer, gallstone | 5 | S2 + gallbladder | 25 mm × 20 mm × 13 mm | 1 | 95 | 20 | 2/1/1 | 0 | 2 |
Single-port laparoscopic surgery further reduces abdominal wall trauma and is of great significance for the development of minimally invasive surgery. However, both the “chopstick” and “sword-fight” effects in the single port laparoscopic operations seriously impair the operating experience of the surgeons and their assistants through increasing the difficulty of surgical field exposure and making the maneuverability of the laparoscopic instruments more awkward. Despite several methods being applied in practice, such as a reduction in the number of instruments or suture suspension[17], none of the modus operandi can workably expose the surgical field well. As a special traction technique, the MAT has been tentatively used in port-reduced laparoscopic surgery and endoscopic submucosal dissection. Mechanically, the magnetic anchor device can generate non-contact attraction outside the body cavity on the target magnet in the cavity, thus being able to create a traction and counter traction effect, which may pull the tissue or organs away from the surgical field and improve the visibility of the anatomical structures. The MAT has been piloted to assist thoracoscopic lung wedge resection and esophagectomy[18,19], laparoscopic cholecystectomy[14,15], and laparoscopic hysterectomy[20]. Moreover, in the endoscopic operation technique, the MAT has been shown to assist the lesion traction in endoscopic submucosal dissection[21,22].
We independently designed and developed Y-Z MADs suitable for laparoscopic surgery. The device has been clinically used for port-reducing and single-port laparoscopic cholecystectomy and has achieved promising clinical results in our clinics. In this study, the Y-Z MAD was used for the first time in a laparoscopic left lateral hepatic lobectomy. Since laparoscopic liver resection is more complex than laparoscopic cholecystectomy, the key aspects should be emphasized during the operation. Firstly, compared with the use of the MAT in laparoscopic cholecystectomy, transumbilical single-port laparoscopic left lateral hepatic lobectomy required a much stronger traction force to be applied to the left lateral lobe of the liver than the gallbladder. If the abdominal wall is too thick, it may mitigate the magnetic field for achieving a firm grasp of the liver, so we only performed the MAT-assisted single port liver procedure on the patients with a BMI less than 30 kg/m2. Secondly, the assistant (magnetic palmist) should know how to dexterously move the anchor magnet to change the grasping direction or extent of tissue or organ exposure to accommodate the needs of the surgeon during the operation. One important aspect to avoid is the large-scale rapid movement of the target magnet to eliminate the “de-anchoring”, which can interrupt the continuity of the surgical operation. In addition, when the magnetic palmist cannot obtain satisfactory exposure by adjusting the anchor magnet, the surgeon should internally adjust the position of the grasping forceps in time in order to obtain a better traction effect. Thirdly, the MAT-assisted transumbilical single-port laparoscopic left lateral hepatic lobectomy is an innovative operating method, so both the surgeon and the assistant should not only master the knowledge of the MAT but also train themselves to improve operating finesses in order to perform the MAT-assisted single-port procedure(s).
This study preliminarily shows that the MAT can assist multiple-port as well as single-port laparoscopic left lateral hepatic lobectomy. The MAT indeed undermined the single-port-related “chopstick” and “sword-fight” effects so that it improved the surgeon’s operating experience and contributed to abating postoperative pain at incisional sites. Of course, this study is a retrospective study with only eight cases, which is a limitation of this study. In future, we will conduct a prospective randomized controlled trial to continuously evaluate the safety and feasibility of the use of the MAT in transumbilical single port left lateral hepatectomy. In summary, this study showed that the MAT is safe and feasible for transumbilical single-port laparoscopic left lateral segment liver resection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade C
Creativity or Innovation: Grade C
Scientific Significance: Grade B
P-Reviewer: Hu Y, China S-Editor: Wang JJ L-Editor: A P-Editor: Xu ZH
| 1. | Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78:956-958. [PubMed] |
| 2. | Delvecchio A, Conticchio M, Ratti F, Gelli M, Anelli FM, Laurent A, Vitali GC, Magistri P, Assirati G, Felli E, Wakabayashi T, Pessaux P, Piardi T, Di Benedetto F, de'Angelis N, Briceño-Delgado J, Adam R, Cherqui D, Aldrighetti L, Memeo R. Laparoscopic major hepatectomy for hepatocellular carcinoma in elderly patients: a multicentric propensity scorebased analysis. Surg Endosc. 2021;35:3642-3652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Hou Z, Xie Q, Qiu G, Jin Z, Mi S, Huang J. Trocar layouts in laparoscopic liver surgery. Surg Endosc. 2022;36:7949-7960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Delvecchio A, Conticchio M, Riccelli U, Ferraro V, Ratti F, Gelli M, Anelli FM, Laurent A, Vitali GC, Magistri P, Assirati G, Felli E, Wakabayashi T, Pessaux P, Piardi T, Di Benedetto F, de'Angelis N, Briceño-Delgado J, Adam R, Cherqui D, Aldrighetti L, Memeo R. Laparoscopic versus open liver resection for hepatocellular carcinoma in elderly patients: a propensity score matching analysis. HPB (Oxford). 2022;24:933-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Viganò L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009;16:410-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, Brock G, McMasters KM. Experience with more than 500 minimally invasive hepatic procedures. Ann Surg. 2008;248:475-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 264] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 7. | Abu Hilal M, McPhail MJ, Zeidan B, Zeidan S, Hallam MJ, Armstrong T, Primrose JN, Pearce NW. Laparoscopic versus open left lateral hepatic sectionectomy: A comparative study. Eur J Surg Oncol. 2008;34:1285-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Cheng Y, Jiang ZS, Xu XP, Huang WF, He GL, Zhou CJ, Qin JS, Gao Y, Pan MX. Single-Port Laparoscopic Surgery Is Feasible and Safe for Hepatic Left Lateral Sectionectomy for Benign Liver Lesions. Gastroenterol Res Pract. 2019;2019:1570796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Hu M, Zhao G, Wang F, Xu D, Liu R. Single-port and multi-port laparoscopic left lateral liver sectionectomy for treating benign liver diseases: a prospective, randomized, controlled study. World J Surg. 2014;38:2668-2673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Struecker B, Haber P, Öllinger R, Bahra M, Pascher A, Pratschke J, Schmelzle M. Comparison of Single-Port Versus Standard Multiport Left Lateral Liver Sectionectomy. Surg Innov. 2018;25:136-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 11. | Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009;23:1393-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 166] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 12. | Yan XP, Shang P, Shi AH, Liu WY, Liu YX, Lü Y. [Exploration and establishment of magnetic surgery]. Kexue Tongbao. 2019;64:815-826. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Shi A, Ma S, Fu S, Zhang Y, Bai J, Zhang X, Ma F, Lyu Y, Yan X. [Design of Internal Grasper Based on Magnetic Anchoring Technique in Trocar-Less Laparoscopic Surgery]. Zhongguo Yi Liao Qi Xie Za Zhi. 2019;43:334-336. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Shang Y, Guo H, Zhang D, Xue F, Yan X, Shi A, Dong D, Wang S, Ma F, Wang H, Li J, Liu X, Luo R, Wu R, Lv Y. An application research on a novel internal grasper platform and magnetic anchoring guide system (MAGS) in laparoscopic surgery. Surg Endosc. 2017;31:274-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Rivas H, Robles I, Riquelme F, Vivanco M, Jiménez J, Marinkovic B, Uribe M. Magnetic Surgery: Results From First Prospective Clinical Trial in 50 Patients. Ann Surg. 2018;267:88-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 16. | Dominguez G, Durand L, De Rosa J, Danguise E, Arozamena C, Ferraina PA. Retraction and triangulation with neodymium magnetic forceps for single-port laparoscopic cholecystectomy. Surg Endosc. 2009;23:1660-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 91] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Ng WT, Kong CK, Wong YT. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:1627. [PubMed] |
| 18. | Li Y, Zhang M, Shi A, Liu P, Zhang H, Zhang Y, Lyu Y, Yan X. Magnetic anchor technique-assisted thoracoscopic lobectomy in beagles. Sci Rep. 2022;12:11916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Chen W, Li Y, Qian R, Jiang M, Lv L, Ren S, Shi A, Yan X, Fu J, Wang H, Ma F, Lv Y, Zhang Y. Application of a novel magnetic anchoring and traction technique in thoracoscopic esophagectomy: a swine experiment. Ann Transl Med. 2021;9:1663. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Zhang L, Wang L, Zhao L, Wang Y, Zhang K, Feng X, Yan X, Lv Y, Li Q. Internal Grasper and Magnetic Anchoring Guidance System in Gynecologic Laparoendoscopic Single-site Surgery: A Case Series. J Minim Invasive Gynecol. 2021;28:1066-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Matsuzaki I, Isobe S, Hirose K, Marukawa T, Esaki M. Magnetic anchor-guided endoscopic submucosal dissection for colonic tumor. Gastrointest Endosc. 2017;85:1111-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Mortagy M, Mehta N, Parsi MA, Abe S, Stevens T, Vargo JJ, Saito Y, Bhatt A. Magnetic anchor guidance for endoscopic submucosal dissection and other endoscopic procedures. World J Gastroenterol. 2017;23:2883-2890. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |