Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.546
Peer-review started: November 6, 2023
First decision: December 6, 2023
Revised: January 2, 2024
Accepted: January 30, 2024
Article in press: January 30, 2024
Published online: February 27, 2024
Processing time: 110 Days and 23.3 Hours
Laparoscopic surgery has reduced morbidity and mortality rates, shorter post
To report the challenges and benefits of introducing laparoscopic surgery in LMIC as well as to identify solutions to these challenges for countries with limited finances and resources.
MEDLINE, EMBASE and Cochrane databases were searched for studies reporting first experience in laparoscopic surgery in LMIC. Included studies were published between 1996 and 2022 with full text available in English. Exclusion criteria were studies considering only open surgery, ear, nose, and throat, endoscopy, arthro
Ten studies out of 3409 screened papers, from eight LMIC were eligible for inclusion in the final analysis, totaling 2497 patients. Most reported challenges were related to costs of equipment and training programmes, equipment pro
Despite financial and technical challenges, many studies emphasise the overall benefit of introducing laparoscopic surgery in LMICs such as reduced hospital stay and the related lower cost for patients. While many of the clinical centres in LMICs have proposed practical solutions to the challenges reported, more support is critically required, in particular regarding training.
Core Tip: While laparoscopic surgery could have major positive effects on patients in low and middle income countries, this type of operation is not widely accessible in many parts of the world. The aim of this study was a systematic review of the literature on laparoscopic surgery in low in middle income countries in order to get a better understanding of first experiences made with minimal invasive surgical techniques and equipment. Out of over 3400 screened papers, 10 studies were selected and analised. We report on common challenges as well as on possible ways to overcome them.
- Citation: Troller R, Bawa J, Baker O, Ashcroft J. First experience in laparoscopic surgery in low and middle income countries: A systematic review. World J Gastrointest Surg 2024; 16(2): 546-553
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/546.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.546
Laparoscopic surgery has become routine practice in many places in the world and has numerous benefits when compared to open surgery, including: Reduced morbidity and mortality, length of hospital stay, blood loss, infection rate and postoperative pain[1-3]. However, laparoscopic surgery is still not routine in many low- and middle income countries (LMICs).
The term LMIC includes low, lower-middle, and upper-middle income countries, defined by their gross national income (GNI). The GNI fluctuates every year, and as of 2022 a LMIC is defined by a GNI per capita of less than $12695[4] (Unless otherwise stated, all monetary values in this paper are in American Dollars: $). This economic deficit can limit access to high-cost technology and its support and represents a great challenge to introduce laparoscopic surgery.
LMICs perform a greater number of procedures with an open approach, rather than a laparoscopic approach. Access to laparoscopic surgery in LMICs is difficult and thus much of the developing world cannot benefit from minimal invasive surgery. Introducing laparoscopic surgical services requires a range of specialist input necessitating that surgical teams are constituted from a broad multidisciplinary background.
This systematic review aims to assess the challenges in introducing laparoscopic surgery service in LMICs and to produce a consensus regarding commencing a high quality, replicable, and collaborative laparoscopic service.
This Systematic Review utilised the preferred reporting items for systematic reviews and meta-analyses statement (PRISMA Statement) to guide all methodology and write up. Before undertaking this review, inclusion criteria were predetermined. Reports met inclusion criteria if they described: (1) A report of first experience in laparoscopic surgery; (2) performed in a low-and-middle income country; (3) were reported in the English language or had an English language translation; and (4) were published after 1996.
Exclusion criteria defined were as follows: (1) Studies focused on open surgery, endoscopy, arthroscopy, cystoscopy, hysteroscopy, hand-assisted surgery, ear, nose, and throat surgery, bariatric surgery, breast surgery, thoracic surgery, robotic surgery, transplant surgery, obstetric; (2) reviews, case reports, letters to the editor or conference abstracts; (3) studies where the patient cohort was equal or smaller than ten; and (4) studies which reported advanced laparoscopic techniques. Studies for which the online full-text was not available were also excluded.
A systematic search of MEDLINE, EMBASE and Cochrane was undertaken until November 2022. An initial search for the identification of laparoscopic surgical reports in LMIC utilised the search terms: “laparoscopic”, “laparoscopy”, and “hand-assisted laparoscopy” in addition to the terms “LMIC” or “developed/developing country”. This broad search strategy generated 4026 articles.
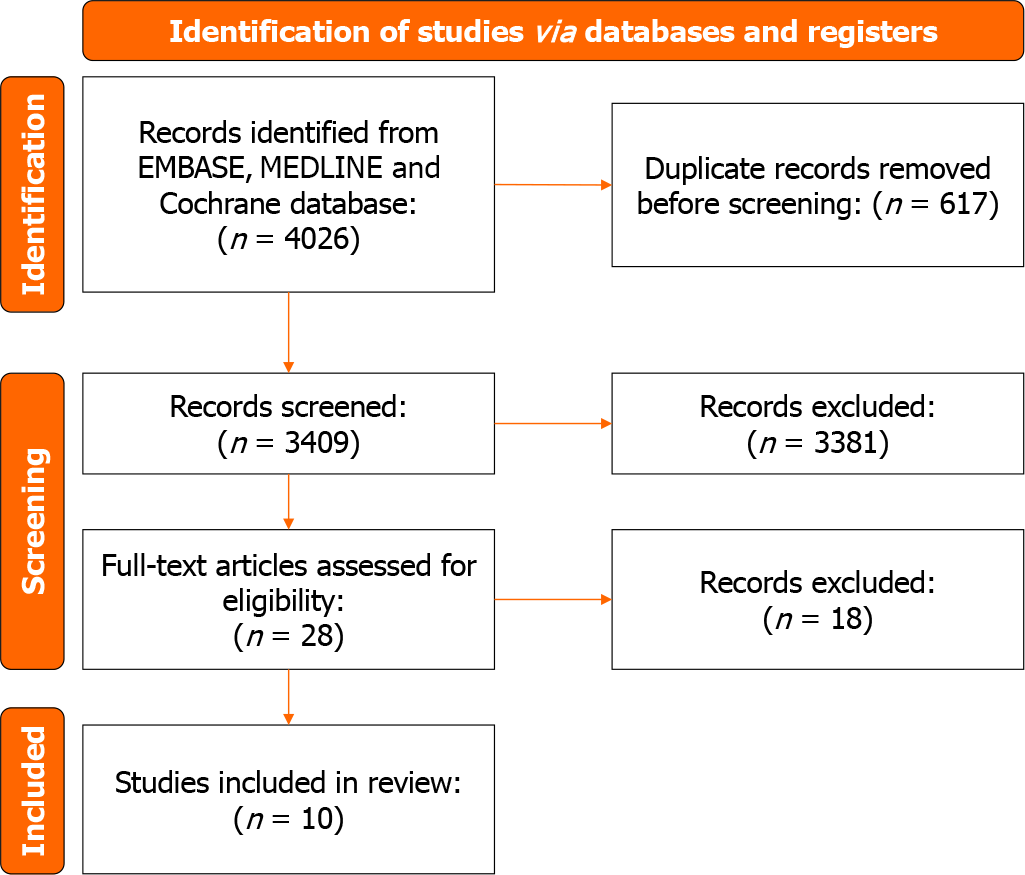
Duplicates were removed (n = 617) and 4 reviewers independently screened abstracts and/or full texts of 3409 publications in reference to study design, study population, and study location as outlined in the inclusion and exclusion criteria. Full screening resulted in the capture of 10 articles which met the predetermined criteria for inclusion into the systematic review. This process is displayed in full in Figure 1. Prior to data extraction it was decided that a meta-analysis would not be undertaken due to the heterogeneity of both laparoscopic implementations and outcome measurements.
Three reviewers independently extracted relevant information from each laparoscopic report using a standardised data extraction method. One author with surgical training expertise reviewed all extracted data. This review captured: Cost, equipment, training, clinical-, economic- and systemic details in addition to quantitative and qualitative outcome measures.
The process of identification, detailing the search and screening strategy is shown in the PRISMA flow diagram (Figure 1).
Ten studies were identified as meeting the inclusion criteria. The majority of these studies were conducted in Africa (n = 9) with four studies being conducted in Nigeria (Table 1)[5-14]. The studies were conducted between 1999 and 2018 and had a study duration of 2.8 years on average. Half were retrospective studies (n = 5), the remainder were prospective (n = 4) and one case series (n = 1). A total of 2497 patients were eligible for inclusion in the final analysis. No multinational studies were identified for inclusion during the screening process.
| Ref. | Country | Year published | Study duration | Specialty | Study design | No. cases |
| Bendinelli et al[5] | Senegal | 2002 | 5 years | Various | Retrospective | 826 |
| Parkar et al[6] | Kenya | 2003 | 2 years | Gynae and general | Retrospective | 408 |
| Patel et al[7] | Kenya | 2003 | 6 years | General | Case series | 106 |
| Raiga et al[8] | Cameroon | 1999 | 4 years | Gynae | Retrospective | 735 |
| Arung et al[9] | Democratic Republic of Congo | 2015 | 10 months | General | Prospective | 75 |
| Adisa et al[10] | Nigeria | 2013 | 2 years | General | Retrospective | 175 |
| Ray-Offor et al[11] | Nigeria | 2014 | 17 months | General and paediatric | Prospective | 15 |
| Onoh et al[12] | Nigeria | 2018 | 2 years | Gynae | Prospective | 36 |
| Ishaq et al[13] | Pakistan | 2016 | 31 months | Paediatric | Retrospective | 100 |
| Ismaila et al[14] | Nigeria | 2013 | 12 months | General | Prospective | 21 |
There were three common themes for the challenges faced when introducing laparoscopic surgery; these related to training, costs and equipment (Table 2)[5-14].
Minimal access surgery requires additional training and skills and this can be challenging in many LMICs[11,12]. As laparoscopic surgery is less often practised, the result is that junior surgeons have poor knowledge of laparoscopy and lack the confidence to use laparoscopy outside of normal working hours, even for emergency cases, such as for appendicitis[7]. Once more surgeons develop an interest and improve skills in laparoscopic surgery, the operating time will reduce[6].
In a study defining the learning curve for laparoscopic colorectal resections in the United States, it was felt that a minimum of 30 procedures was required for laparoscopic colorectal resection in an expert unit, with early cases being associated with higher conversion to open, operative time, and post-operative stay[15].
Apart from the additional training for surgeons, many centres found it challenging to introduce laparoscopic surgery because they did not have adequately trained staff such as theatre nurses, technicians and scrub nurses[6,7,9,11]. As laparoscopic surgery is not widely practised in LMICs, it may be that these skills are not taught to trainees[16] and in turn there is no motivation for training support staff in these skills.
Some studies reported on the training of local staff either abroad or in their hospital by surgeons from abroad. Training was provided not only for the surgeons, but also the theatre staff, nurses and paramedics[9]. A gynaecology team from Cameroon were trained over seven years by a surgeon from France[8]. The anaesthetists and theatre staff of the same team also benefited from several months of training[8]. In some cases, it falls on the operating surgeon to train the entire team (endoscopy nurses and technicians) as there is inadequate training of support staff[11].
Some centres are struggling with a complete absence of basic training in laparoscopic surgery resulting in underperformance and a very slow learning curve[12]. Once more surgeons develop an interest and improve their skills in laparoscopic surgery, a reduction in operating time can be achieved[6]. This is reflected in the units that were only able to perform laparoscopic procedures intermittently, yet still reported reduced operation times and improvement of surgical skills[9,12].
Training is not only an issue for clinical teams, but also for the engineering teams that maintain the laparoscopic equipment. Local biometric engineers are often not knowledgeable about the endoscopic instruments or trained to fix them[12,14]. Maintenance of laparoscopic equipment by untrained staff can lead to malfunction and contribute to equipment problems encountered during surgery[17]. To reduce cost, reusable instruments are used and therefore careful sterilisation is necessary which requires advanced know-how[14].
While the long term costs of laparoscopic surgery are comparable or even cheaper than the ones of open surgery, the initial investment for equipment, training and infrastructure can pose a problem. In one of the first studies introducing laparoscopic appendicectomy in the United States, it was found that laparoscopic surgery required a significant increase in intraoperative equipment charge ($125.32 ± $3.99 open vs $1078.70 ± $24.06 Lap), operative time charge ($3022.16 ± $57.51 vs $4065.24 ± $122.64), and total hospital charge ($12310 ± $772 vs $16773 ± $1319)[18].
Six studies report the cost to acquire laparoscopic equipment and consumables in LMICs as an issue to establish a laparoscopic surgery service in their respective hospitals. The main challenge in LMICs is the high initial costs to acquire laparoscopic equipment and consumables[9]. This is in part due to the absence of local production companies resulting in a lack of supply of instruments on demand and in part due to fewer alternative options being available to purchase affordable equipment[12].
Regarding the operational costs, Ray-Offor et al[11] reported that after the initial setup, which includes training of personnel, acquisition of equipment and building the relevant infrastructure, the operational costs for laparoscopic surgery is not huge (though without exact specification or comparison to open surgery)[11]. Similarly, Bendinelli et al[5] reported that the hospital could recover more than 87% of its investment in 6 years and the higher surgical charges were compensated by reduced hospitalisation costs postoperatively[5].
Adisa et al[10] and other centres described how they were able to reduce costs with local adaptations like investing in reusable instruments, which helped to reduce the cost per patient[10,11]. They also made camera covers using drapes that can be washed and sterilised and limited the use of retrieval bags for purulent appendix specimens. No advanced energy devices such as harmonic or Ligasure were used[10].
Depending on the pricing model of the hospital laparoscopic surgery can even be more financially viable than open surgery. For example, Bendinelli et al[5] report that in hospitals with fixed charges per surgery and per day, the costs for patients in the laparoscopic surgery group were lower when compared to the open surgery group, due to shorter length of hospital stay and fewer complications[5].
Another barrier to introducing laparoscopic surgery in LMICs is the lack of a well established healthcare system with insurance where patients must pay for the surgery and hospital stay themselves[10,12]. In these settings, hospitals often operate with extremely low margins and generate very little profit. As a result, for a long time, laparoscopic surgery in LMICs was only offered in private hospitals who historically have been more likely to be able to afford the higher upfront investment cost required for modern equipment and training[9,10].
One of the overall benefits of laparoscopic surgery compared to open surgery is the reduced hospital stay which means lower costs for patients in LMICs[5,7,10,12]. Diagnostic laparoscopy is one of the most convenient procedures; it is simple, cost-effective and avoids an unnecessary laparotomy which leads to a shorter postoperative stay and lower costs[5,9,12].
Equipment challenges evolve mostly around the acquisition of equipment and the reliability of equipment and infrastructure[5,6]. Most of the hospitals received donations of endoscopic instruments from corporations, companies or visiting surgeons[5,8,12,14]. Relying on such donations and investing in reusable equipment were two methods to achieve cost effectiveness.
Some studies noted that the costs for laparoscopic surgery are not much higher than conventional surgery after the initial set-up, training of staff and acquisition of relevant infrastructure[11,19]. For the initial set-up, cooperation with developed countries and public institutions can be helpful to obtain laparoscopic supplies[5]. However, the lack of local companies producing laparoscopic equipment can lead to maintenance problems. Maintenance of laparoscopic equipment by untrained staff contributes to some problems encountered during surgery as well as challenges with effective sterilisation and care of the instruments[14].
Another commonly reported challenge is unreliable infrastructure which can lead to power outages or unreliable power supplies[11,12,14], which creates a huge problem as laparoscopic surgery requires a reliable source of electricity. Introduction of solar power or electricity by a generator or an alternate power supply during surgeries could provide a solution to the power outages[11].
Adisa et al[10] introduced laparoscopic surgery with a basic setup using regular TV manual carbon dioxide insufflations. They reported four conversions due to equipment failure and technical difficulties[10]. In two cases loss of view due to a faulty cable that could not be immediately resolved and two conversions happened due to excessive intraoperative bleeding. This study highlighted how the costs and difficulties of replacing damaged laparoscopic equipment can be a limiting factor to continuing minimally invasive surgery[12].
Specific issues with equipment such as diathermy malfunctioning, faulty suction, gas leak from a malfunctioning port, and a non-functioning clip applicator were reported by Ismaila et al[14].
One study reported lack of acceptance of laparoscopic surgery being a challenge; surgeons had a preference for non-endoscopic techniques and were not keen on trying a new technique[12]. In addition, the initial set-up for laparoscopic surgery can be time-consuming, which can prolong operating time and cause problems in view of competing theatre usage[11].
Bureaucratic issues regarding procurement and approving endoscopic equipment can be another challenge in introducing minimally invasive surgery[12,14].
Most authors looked at complication and conversion rates. Complication rate is known to be related to the level of training and experience in laparoscopic surgery[20]. As Parkar et al[6] pointed out, laparoscopic training and collaboration with local trainers or those from overseas is crucial for the development of minimal invasive surgery[5,12].
An increased conversion rate related to inadequate equipment, malfunction and poor patient selection was reported by Onoh et al[12]. One hospital reported a conversion rate of 38% (16 conversions of 42 Laparoscopic appendicectomy), most of them due to intraoperative difficulties such as retrocaecal appendix, necrosed fragmented appendix or adhesions[7]. That being said, most authors reported a conversion rate comparable to the number in developed countries[21] between 1 and 10%[5,6].
One study reported six port site complications (1.47%) of which two needed subsequent laparotomy only seven days post laparoscopic surgery[6]. This is comparable to the other studies reporting port site complications between 3% and 9% within three months after surgery[22,23].
A number of studies highlighted the reduction in operating time with experience[6,9,10] as well as shorter postoperative stay and less pain after laparoscopic surgery[5,9,10].
Diagnostic laparoscopy is one of the most convenient procedures and can avoid an unnecessary laparotomy which leads to reduced wound infection rates[7,9,10], minimises scar formation[7], allows earlier return to normal activities[7,12], less pain[9] and reduces postoperative adhesions[7,8]. The routine use of diagnostic laparoscopy can also reduce morbidity and mortality for patients with suspected intra-abdominal malignancies compared to diagnostic laparotomies for these patients[10].
Laparoscopic surgery presents significant opportunities for enhancing healthcare delivery in low and middle-income countries (LMICs). Its advantages, including shorter hospital stays, improved patient outcomes due to lower infection rates and fewer laparotomies which enable a quicker return to work, highlight the potentially transformative impact on healthcare systems in resource-limited settings.
While these opportunities are promising, numerous challenges must be addressed to fully realise the benefits of laparoscopic surgery in LMICs.
Costs for equipment, training and infrastructure are a major barrier due to low income and the associated low economic development in LMICs. The economic difficulties that face many LMICs may have been a result of conflicts, inequality, lack of education and poor basic infrastructure. Therefore, support of LMICs in introducing laparoscopic surgery and training needs to be built and adapted to local practice to be sustainable.
One of the primary hurdles is the substantial initial investment required for acquiring and maintaining laparoscopic equipment. The higher acquisition and maintenance costs, and limited financial resources in LMICs, pose a significant barrier to widespread adoption. Moreover, the absence of skilled local labour for equipment maintenance aggravate these challenges, leading to potential equipment downtime and reduced accessibility to laparoscopic equipment.
The absence of a local support industry further complicates the sustainability of laparoscopic surgery in LMICs. Inadequate infrastructure, including unstable power and water supply, presents operational difficulties and jeopardises the continuity of surgical procedures. The need for larger sterilisation equipment adds to the infrastructure demands, requiring substantial modifications that may not align with existing healthcare facilities in these regions.
A critical challenge remains the scarcity of trained surgeons in laparoscopic surgery in LMICs associated with a lack of local surgical training opportunities and educational resources. Efforts to establish comprehensive training programs tailored to the specific needs of these regions are imperative to overcome this limitation. Collaborations between local and international medical institutions could facilitate knowledge transfer and skill development, ultimately empowering local healthcare professionals. Previous reports have documented successful introduction of a laparoscopic surgical service, such as the Ministry of Health in Botswana where 12 surgeons were trained through a combination of hands-on teaching, tele-simulation, workshops and mentorship to begin a laparoscopic cholecystectomy program[24].
Strategies to address these challenges should focus not only on infrastructure shortcomings but also establishing sustainable training programs and support systems for equipment maintenance. Innovative financing models and technology-sharing initiatives could alleviate the financial burden associated with the adoption and maintenance of laparoscopic surgery in LMICs.
On the whole, laparoscopic surgery could have a huge potential in LMICs. Collaborative efforts between international surgeons, companies, and local units emerge as a cornerstone for success in navigating the challenges.
Identification of essential equipment needs and skill gaps, coupled with comprehensive training programs for both clinical staff and equipment engineers, are needed for a sustainable implementation. Reusable equipment not only addresses financial constraints but also aligns with the principles of resource efficiency which is crucial in resource-limited settings. Given the lack of local resources and skills, the use of remote technology, such as video-based training materials or remote video-assistance to train and mentor local teams could also be considered.
The introduction of solar electricity or alternative power supplies could enable better coping with disruptions posed by unreliable power supply, ensuring uninterrupted surgical procedures.
Further studies around the cost-effectiveness of laparoscopic surgery in LMICs are required, to evaluate approaches that might enable LMICs to benefit from minimal invasive surgery. Lastly, a future survey which also includes studies from less economically prosperous areas within otherwise more developed countries, might help yield a larger number of studies and hence increase the validity of the review.
Laparoscopic surgery has become routine practice in many places in the world and has numerous benefits when compared to open surgery, including: Reduced morbidity and mortality, length of hospital stay, blood loss, infection rate and postoperative pain. However, laparoscopic surgery is still not routine in many low- and middle income countries (LMIC) as introducing minimal invasive surgery can be expensive and requires resources. The economic deficit in low-and middle income countries can limit access to high-cost technology and its support and represents a great challenge to introduce laparoscopic surgery. In low-and middle income countries most surgeries are performed with an open approach, rather than a laparoscopically. Access to laparoscopic surgery in LMICs is difficult and thus much of the developing world cannot benefit from minimal invasive surgery. Introducing laparoscopic surgical services requires a range of specialist input necessitating that surgical teams are constituted from a broad multidisciplinary background.
This systematic review aims to assess the challenges in introducing laparoscopic surgery service in LMICs and to produce a consensus regarding commencing a high quality, replicable, and collaborative laparoscopic service.
The main objective was to assess the challenges in surgical services in Low- and middle-income countries. We could identify the main gaps and problems and analysed potential solutions. But also identified the need for future studies addressing certain questions and design.
Systematic review of MEDLINE, EMBASE and Cochrane databases.
Ten studies have been included in this systematic review. They main challenges found were related to costs, training and equipment. Lack of training opportunities, faulty equipment or access to equipment and the associated costs. Some studies highlighted the benefits of introducing laparoscopic surgery, particularly the reduction in hospital stay, lower complications and lower morbidity and mortality.
Identification of essential equipment needs and skill gaps, coupled with comprehensive training programs for both clinical staff and equipment engineers, are needed for a sustainable implementation. Reusable equipment, the use of remote technology, such as video-based training materials or remote video-assistance to train and mentor local teams, introduction of solar electricity or alternative power supplies should be considered. Further studies to assess cost-effectiveness of laparoscopic surgery and studies which also includes papers from less economically prosperous areas within developed countries might help to increase the validity of the review.
Further studies to assess cost-effectiveness of laparoscopic surgery and studies which also includes papers from less economically prosperous areas within developed countries might help to increase the validity of the review.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Navarrete Arellano M, Mexico S-Editor: Li L L-Editor: A P-Editor: Yuan YY
| 1. | Buia A, Stockhausen F, Hanisch E. Laparoscopic surgery: A qualified systematic review. World J Methodol. 2015;5:238-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 143] [Article Influence: 14.3] [Reference Citation Analysis (4)] |
| 2. | Braga M, Vignali A, Zuliani W, Frasson M, Di Serio C, Di Carlo V. Laparoscopic vs open colorectal surgery: cost-benefit analysis in a single-center randomized trial. Ann Surg. 2005;242:890-895, discussion 895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Jaschinski T, Mosch CG, Eikermann M, Neugebauer EA, Sauerland S. Laparoscopic vs open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;11:CD001546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 122] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 4. | Worldbank, World Bank GNI per capita in middle income countries, 2022. Aug 29, 2022. [cited 13 January 2024]. Available from: https://www.worldbank.org/en/country/mic/overview#1. |
| 5. | Bendinelli C, Leal T, Moncade F, Dieng M, Toure CT, Miccoli P. Endoscopic surgery in Senegal. Benefits, costs and limits. Surg Endosc. 2002;16:1488-1492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Parkar RB, Thagana NG, Baraza R, Otieno D. Experience with laparoscopic surgery at the Aga Khan Hospital, Nairobi. East Afr Med J. 2003;80:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Patel SC, Jumba GF, Akmal S. Laparoscopic appendicectomy at the Aga Khan Hospital, Nairobi. East Afr Med J. 2003;80:447-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Raiga J, Kasia JM, Bruhat MA. Laparoscopic surgery in the Cameroon. Int J Gynaecol Obstet. 1999;65:65-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Arung W, Dinganga N, Ngoie E, Odimba E, Detry O. First steps of laparoscopic surgery in Lubumbashi: problems encountered and preliminary results. Pan Afr Med J. 2015;21:210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Adisa AO, Lawal OO, Arowolo OA, Alatise OI. Local adaptations aid establishment of laparoscopic surgery in a semiurban Nigerian hospital. Surg Endosc. 2013;27:390-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Ray-Offor E, Okoro P, Gbobo I, Allison A. Pilot study on laparoscopic surgery in port-harcourt, Nigeria. Niger J Surg. 2014;20:23-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Onoh RC, Ezeonu PO, Lawani LO, Ajah LO, Ezegwui HU, Ejikeme BN. Experiences and challenges of gynecological endoscopy in a low-resource setting, Southeast Nigeria. Trop J Obstet Gynaecol. 2018;35:30-37. [RCA] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 13. | Ishaq H, Qazi SH, Dogar S, Khan Durrani MY, Faruque AV. Pediatric laparoscopic surgery; initial experience from Pakistan; first 100 cases in single center. J Pak Med Assoc. 2016;66:S116-S118. [PubMed] |
| 14. | Ismaila BO, Shuaibu SI, Ale AA. Laparoscopic surgery in a Nigerian teaching hospital for 1 year: challenges and effect on outcomes. Niger J Med. 2013;22:134-137. [PubMed] |
| 15. | Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC. Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum. 2001;44:217-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 305] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 16. | Wilkinson E, Aruparayil N, Gnanaraj J, Brown J, Jayne D. Barriers to training in laparoscopic surgery in low- and middle-income countries: A systematic review. Trop Doct. 2021;51:408-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 17. | Asbun HJ, Berguer R, Altamirano R, Castellanos H. Successfully establishing laparoscopic surgery programs in developing countries. Clinical results and lessons learned. Surg Endosc. 1996;10:1000-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Cothren CC, Moore EE, Johnson JL, Moore JB, Ciesla DJ, Burch JM. Can we afford to do laparoscopic appendectomy in an academic hospital? Am J Surg. 2005;190:950-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Gehrman J, Angenete E, Björholt I, Lesén E, Haglind E. Cost-effectiveness analysis of laparoscopic and open surgery in routine Swedish care for colorectal cancer. Surg Endosc. 2020;34:4403-4412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Brosens I, Gordon A, Campo R, Gordts S. Bowel injury in gynecologic laparoscopy. J Am Assoc Gynecol Laparosc. 2003;10:9-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Moghadamyeghaneh Z, Masoomi H, Mills SD, Carmichael JC, Pigazzi A, Nguyen NT, Stamos MJ. Outcomes of conversion of laparoscopic colorectal surgery to open surgery. JSLS. 2014;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Madan Mohan Mudgal, Pradeep Kumar Kothiya, Naveen Kushwah, Raghvendra Singh. Port site complications following laparoscopic surgeries: a prospective study. Int Surg J. 2018;5:598-601. [DOI] [Full Text] |
| 23. | Karthik S, Augustine AJ, Shibumon MM, Pai MV. Analysis of laparoscopic port site complications: A descriptive study. J Minim Access Surg. 2013;9:59-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 24. | Bedada AG, Hsiao M, Bakanisi B, Motsumi M, Azzie G. Establishing a contextually appropriate laparoscopic program in resource-restricted environments: experience in Botswana. Ann Surg. 2015;261:807-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |