Published online Feb 27, 2024. doi: 10.4240/wjgs.v16.i2.539
Peer-review started: October 15, 2023
First decision: December 6, 2023
Revised: December 20, 2023
Accepted: January 9, 2024
Article in press: January 9, 2024
Published online: February 27, 2024
Processing time: 133 Days and 2.1 Hours
To avoid acute variceal bleeding in cirrhosis, current guidelines recommend screening for high-risk esophageal varices (EVs) by determining variceal size and identifying red wale markings. However, visual measurements of EV during routine endoscopy are often inaccurate.
To determine whether biopsy forceps (BF) could be used as a reference to improve the accuracy of binary classification of variceal size.
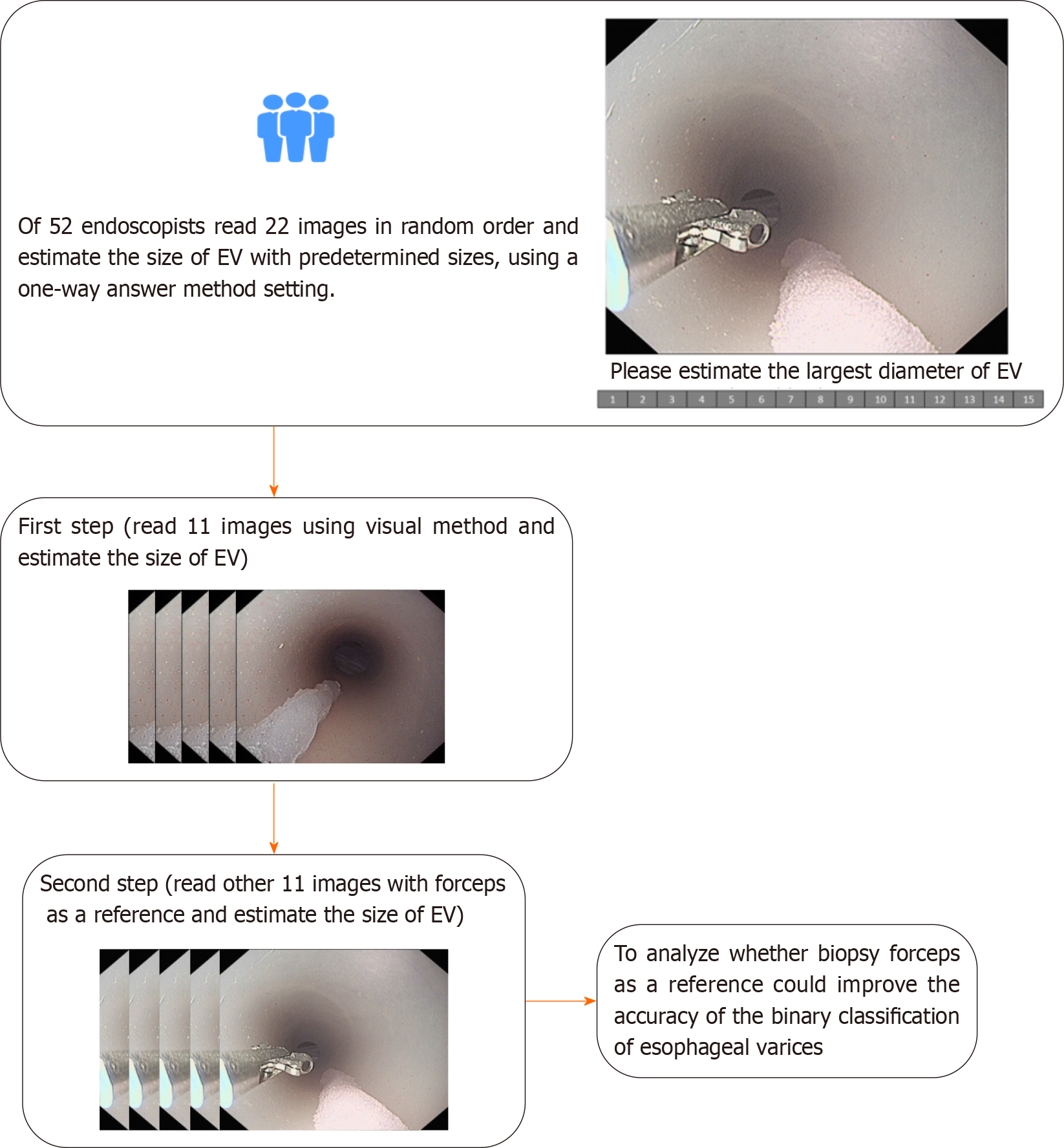
An in vitro self-made EV model with sizes ranging from 2 to 12 mm in diameter was constructed. An online image-based survey comprising 11 endoscopic images of simulated EV without BF and 11 endoscopic images of EV with BF was assembled and sent to 84 endoscopists. The endoscopists were blinded to the actual EV size and evaluated the 22 images in random order.
The respondents included 48 academic and four private endoscopists. The accuracy of EV size estimation was low in both the visual (13.81%) and BF-based (20.28%) groups. The use of open forceps improved the ability of the endoscopists to correctly classify the varices by size (small ≤ 5 mm, large > 5 mm) from 71.85% to 82.17% (P < 0.001).
BF may improve the accuracy of EV size assessment, and its use in clinical practice should be investigated.
Core tip: This study explored whether biopsy forceps (BF) could be used as a reference to improve the accuracy of binary classification of variceal size. Our results showed that visual estimation was insufficient for accurate classification of esophageal varices according to size, and the ability of endoscopists to correctly classify the varices by size improved significantly with the use of BF.
- Citation: Duan ZH, Zhou SY. Biopsy forceps are useful for measuring esophageal varices in vitro. World J Gastrointest Surg 2024; 16(2): 539-545
- URL: https://www.wjgnet.com/1948-9366/full/v16/i2/539.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i2.539
Accurate size estimation of esophageal varices (EVs) is essential for determining the exact diagnostic category, appropriate therapy, and observational intervals for patients with liver cirrhosis[1-3]. Visual estimation is currently the most commonly used method, but the estimation of EV size during endoscopy is highly inconsistent among different endoscopists[4-6], with only fair to moderate interobserver agreements reflected by kappa values of 0.38–0.59. In clinical practice, a cut-off diameter of 5 mm is used to classify varices as large or small. However, misclassification of variceal size may occur due to the lack of a reference during endoscopy and variable degrees of air insufflation[7]. As inaccurate assessment of variceal size may negatively influence the management of liver cirrhosis, the development of a method for accurate variceal size measurement has received much attention in recent years. Although the use of biopsy forceps (BF) has been advocated as a reference to improve the accuracy of variceal size classification, there are currently no reported validity data. We therefore aimed to investigate whether the use of BF improves the accuracy of variceal size estimation. Since accurate measurement of exact EV diameter is difficult in clinical practice, we constructed an in vitro EV model with a known variceal size as the gold standard for this simulation study.
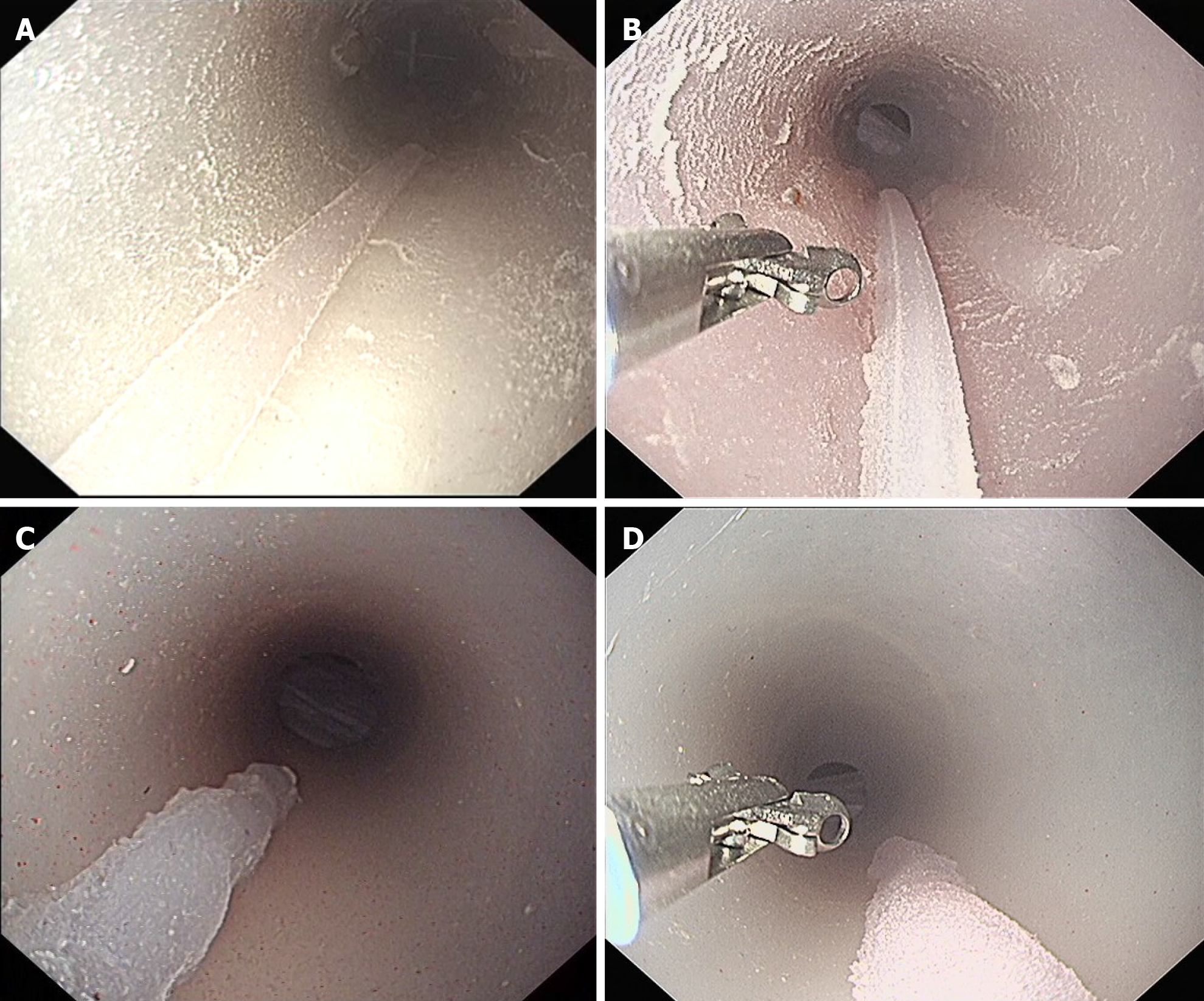
An in vitro esophagus model was constructed and modified by affixing 22 silicone varices (Figures 1 and 2). A common type of BF (Model 220824, Hangzhou Kangsheng Medical Equipment Corporation, Hangzhou, China) was used. The maximum opening distance between the two cups of the BF was approximately 6 mm. The exact EV size was determined by manually measuring the varices using calipers and calculating the average of three measurements using the rounding-off method. An Olympus GIF H260 gastroscope (Olympus, Tokyo, Japan) was used. The simulated EV with known exact variceal size was then used to evaluate the potential of BF for improving the accuracy of EV size estimation. An image-based online test was compiled and completed by 52 endoscopists to compare the accuracy of conventional visual estimation with estimations using BF as a reference point.
An experienced endoscopist (Duan ZH) performed all the gastroscopic procedures and high-definition endoscopic images were saved. Eleven varices with known sizes, ranging from 2 to 12 mm in diameter, were photographed using a gastroscope without BF as a reference. The varices were subsequently photographed using BF as a reference during endoscopy. The BF were viewed at approximately the same length and location in all the images (Figure 2).
A total of 84 endoscopists were invited to participate in this study by Wechat, as per Wenjuanxing, an online survey platform. Inclusion criteria for the endoscopists included voluntary participation in an anonymous, online image-based test and submission after completing all answers. Each endoscopist completed a questionnaire that included 30 questions on age, sex, professional experience, type of practice setting, and number of gastroscopies performed per year. All the participants were blinded to the actual sizes of the simulated varices and were asked to assess the largest diameter of each of the 11 artificial varices, first without BF and then with BF as a reference. For each EV, the participants had to choose the size as a whole number ranging from 2 to 15 mm. The images were shown to the participants in random order and participants could not go back to revise previous answers.
The study was approved by the Institutional Review Board of Xingtai People’s Hospital on June 28, 2023 (approval No. 2023046). Patient consent was not required as no patient data were collected. Each participant volunteered for the study and provided informed consent for participation in this anonymous online survey.
To date, the accuracy of open BF-based estimation of EV size compared with visual estimation has not been reported. A minimum of 499 measurements were needed in both the visual estimation and open BF-based estimation groups for an independent test with a power of 80%, α = 0.05. This study included 572 measurement datapoints for each of the two groups.
The measurement error was calculated by subtracting the gold standard from the corresponding estimation result. Continuous variables were expressed as mean ± SD, and categorical variables were expressed as frequencies and percentages. Student’s t test was used to compare differences in measurement error of the two estimation methods. The overall accuracy of classifying variceal size categories was compared using the χ2 test. Statistical significance was set at
Fifty-two endoscopists, including 48 academic and four private endoscopists, responded and completed the online survey. The average gastroscopic experience was 11.0 ± 6.9 years, and 37 participants performed > 500 gastroscopies yearly (Table 1). The endoscopists first performed a visual evaluation of 11 images of simulated varices with known exact sizes, then they evaluated the images using BF as a reference. A total of 1144 measurements were collected (572 in the visual group and 572 in the open BF group).
| Participants’ characteristics | n (%) |
| No. of participants | 52 |
| Practice setting (all) | 52 |
| Academic | 48 (92.3) |
| Private | 4 (7.7) |
| Age, yr (mean, SD) | 39.9 (6.6) |
| Gender (male) | 26 (50) |
| Years in practice (mean, SD) | 11.0 (6.9) |
| No. of gastroscopies/year | |
| < 500 | 15 (28.9) |
| 501-1000 | 9 (17.3) |
| 1001-1500 | 5 (9.6) |
| 1501-2000 | 7 (13.5) |
| > 2000 | 16 (30.8) |
The exact measurement accuracies using the visual and open BF-based estimation methods were 13.81% and 20.28%, respectively (P=0.004) (Table 2). The use of open BF significantly improved the accuracy of correctly classifying large varices (> 5 mm), but did not improve the accuracy of classifying small varices (≤ 5 mm) (Table 2). Table 3 shows the number of exact classifications of simulated EV with actual diameters ranging from 2 mm to 12 mm by visual or open BF-based estimation.
| Visual method | Biopsy forceps | P value | |
| All varices | |||
| Accuracy (exact) | 13.81% | 20.28% | 0.004 |
| Actual size ≤ 5 mm | |||
| Accuracy (exact) | 22.12% | 34.62% | 0.005 |
| Actual size > 5 mm | |||
| Accuracy (exact) | 9.07% | 12.09% | 0.185 |
| Correct classification | |||
| ≤ 5 mm (category A) | 84.62% | 87.98% | 0.996 |
| > 5 mm (category B) | 64.56% | 78.85% | < 0.0001 |
| Actual size ≤ 5 mm (4 varices) | Actual size > 5 mm (7 varices) | |
| Visual method | ||
| Size estimate ≤ 5 mm | 176 | 129 |
| Size estimate > 5 mm | 32 | 235 |
| Accuracy | 84.62% | 64.56% |
| Biopsy forceps | ||
| Size estimate ≤ 5 mm | 183 | 77 |
| Size estimate > 5 mm | 25 | 287 |
| Accuracy | 87.98% | 78.85% |
When the varices were classified as small (≤ 5 mm) or large (> 5mm), the use of open BF improved the accuracy of the estimated sizes (percentage of measurements where the varices were classified correctly into the correct size category) (P < 0.001) (Table 3). When data from participants with less experience (< 500 gastroscopies per year, n = 15) were analyzed separately, the use of BF improved the overall accuracy of categorizing the size from 75.15% to 85.45%(P=0.019).The greatest improvement was observed for large varices, with the classification accuracy of all 52 endoscopists improving from 64.56% to 78.85% (P < 0.001) (Tables 2 and 3).
Upper gastrointestinal bleeding due to EVs in patients with portal hypertension is associated with high morbidity and mortality rates[1]. As the risk of variceal bleeding is assessed by variceal size[1], accurate measurement of EV size is important. We therefore aimed to improve the accuracy of endoscopists to estimate EV size. Comparison of the accuracy of open BF-based estimation with visual estimation of EV size in a simulated esophagus model revealed that the ability of endoscopists to correctly classify varices by size (small vs large) is significantly improved by the use of open BF. A previous study by Li et al[8] evaluated the efficacy of an endoscopic diameter ruler in vitro; however, handling of the endoscopic ruler was complex and increased the cost. A study by Jin et al[9] reported that a virtual ruler based on artificial intelligence was more accurate in measuring variceal diameter in clinical practice; however, the sample size of the study was small (n = 7), and the gold standard for variceal diameter was unknown. Notably, both the virtual and endoscopic rulers[8,9] require placement of external devices that are not used in routine endoscopic practice. In contrast, BF are used in routine endoscopic procedures, and two studies[10,11] have confirmed that BF-based estimation is more accurate than visual estimation, which is consistent with our results.
Although previous studies show that endoscopists often estimate the size of esophageal lesions inaccurately when using conventional endoscopy, with an overall incorrect estimation rate of 67.9%[12], there are few studies on the accuracy of EV size determination that report the actual EV size[8]. An in vitro study by Li et al[8] used columnar objects that mimicked varices, but their shapes were dissimilar to those of the human esophagus and varices. In contrast, our silicone EV model exhibited greater similarity to these structures.
This study had some limitations. First, it was limited by the use of a simulation model, which was required as measuring the actual sizes of EV in clinical practice is difficult. To validate BF measurements in humans in follow-up studies, we will select physicians who demonstrated a high accuracy in variceal size measurement when participating in this study. Second, the shape of the varices in our model differed from the shape of human varices. However, as our preclinical study focused primarily on the maximum diameter of the veins, it is reasonable to assume that the use of BF may be feasible in future studies in humans.
This study had several strengths. First, we introduced a self-made, simple, low-cost, artificial EV model with specified variceal sizes. Second, we used still images with similar viewing distances and angles when taking photographs during endoscopy to strictly control the experimental conditions, such as image distortion from the eye lens of the gastroscope[13]. Third, the sample size was large, including 52 participants and 1144 measurements; this exceeded the sample size of a previous study (680 measurements)[14], and thus represented the largest study to date to evaluate endoscopic and BF-based estimation of variceal size.
The use of open BF can significantly improve EV binary classification accuracy. Additional clinical studies using BF during gastroscopy are needed to validate our results.
Accurate estimation of esophageal varices (EVs) is essential because variceal diameter is used to determine the exact diagnostic category, appropriate therapy, and observational intervals for patients with liver cirrhosis. However, visual estimation of EV size by endoscopists are often inaccurate.
Upper gastrointestinal bleeding due to EVs is associated with high morbidity and mortality rates. As the risk of variceal bleeding is assessed by variceal size, accurate measurement of EV size is important. We therefore need to improve the accuracy of endoscopists to estimate EV size.
We aimed to evaluate whether open biopsy forceps (BF) can be used to improve the accuracy of binary classification of EV size.
A simulated EV model with known EV sizes was constructed. An online image-based test comprising 11 endoscopic images of simulated EV without BF and 11 endoscopic images of EV with BF was evaluated in random order by 52 endoscopists.
The ability of endoscopists to correctly classify the varices according to size (small, ≤ 5 mm vs large, > 5 mm) was improved from 71.85% to 82.17% with the use of open BF (P < 0.001).
This study showed that using open BF as a reference may improve the assessment of variceal size. However, its use in clinical endoscopy practice requires further investigation.
Using open BF as a reference may significantly improve the accuracy of esophageal variceal size binary classification. Additional clinical studies using BF during gastroscopy are required to confirm our findings.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aydin S, Turkey; Martino A, Italy S-Editor: Wang JJ L-Editor: Kerr C P-Editor: Zhao YQ
| 1. | Masood I, Moshksar A, Wong B, Khan H, Saleem A. A comprehensive review of transvenous obliteration techniques in the management of gastric varices. DiagnInterv Radiol. 2023;29:146-154. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C; Baveno VII Faculty. Baveno VII – Renewing consensus in portal hypertension. J Hepatol. 2022;76:959-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1537] [Cited by in RCA: 1505] [Article Influence: 501.7] [Reference Citation Analysis (2)] |
| 3. | Gralnek IM, Camus Duboc M, Garcia-Pagan JC, Fuccio L, Karstensen JG, Hucl T, Jovanovic I, Awadie H, Hernandez-Gea V, Tantau M, Ebigbo A, Ibrahim M, Vlachogiannakos J, Burgmans MC, Rosasco R, Triantafyllou K. Endoscopic diagnosis and management of esophagogastric variceal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2022;54:1094-1120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 125] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 4. | Calès P, Zabotto B, Meskens C, Caucanas JP, Vinel JP, Desmorat H, Fermanian J, Pascal JP. Gastroesophageal endoscopic features in cirrhosis. Observer variability, interassociations, and relationship to hepatic dysfunction. Gastroenterology. 1990;98:156-162. [PubMed] |
| 5. | Bendtsen F, Skovgaard LT, Sørensen TI, Matzen P. Agreement among multiple observers on endoscopic diagnosis of esophageal varices before bleeding. Hepatology. 1990;11:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | D’Antiga L, Betalli P, De Angelis P, Davenport M, Di Giorgio A, McKiernan PJ, McLin V, Ravelli P, Durmaz O, Talbotec C, Sturm E, Woynarowski M, Burroughs AK. Interobserver Agreement on Endoscopic Classification of Oesophageal Varices in Children. J Pediatr Gastroenterol Nutr. 2015;61:176-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Fateen W, Ragunath K, White J, Khanna A, Coletta M, Samuel S, Ortiz J, James M, Wilkes E, Aithal GP, Guha IN, Sami SS. Validation of the AASLD recommendations for classification of oesophageal varices in clinical practice. Liver Int. 2020;40:905-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Li ZQ, Linghu EQ, Hu M, Wang XD, Wang HB, Meng JY, Du H. Endoscopic measurement of variceal diameter. World J Gastroenterol. 2015;21:2140-2146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Jin J, Dong B, Ye C, Zhang Q, Wu A, Dong L, Kong D. A Noninvasive Technology Using Artificial Intelligence to Measure the Diameter of Esophageal Varices Under Endoscopy. Surg Laparosc Endosc Percutan Tech. 2023;33:282-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 10. | Sudarevic B, Sodmann P, Kafetzis I, Troya J, Lux TJ, Saßmannshausen Z, Herlod K, Schmidt SA, Brand M, Schöttker K, Zoller WG, Meining A, Hann A. Artificial intelligence-based polyp size measurement in gastrointestinal endoscopy using the auxiliary waterjet as a reference. Endoscopy. 2023;55:871-876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 11. | Jin HY, Leng Q. Use of disposable graduated biopsy forceps improves accuracy of polyp size measurements during endoscopy. World J Gastroenterol. 2015;21:623-628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Polymeros D, Triantafyllou K, Tzathas C, Emmanuel T, Tsironi E, Ladas SD. Accuracy of measurements of the length of esophageal lesions: an experimental study. Endoscopy. 2007;39:948-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Sakata S, McIvor F, Klein K, Stevenson ARL, Hewett DG. Measurement of polyp size at colonoscopy: a proof-of-concept simulation study to address technology bias. Gut. 2018;67:206-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Kaz AM, Anwar A, O’Neill DR, Dominitz JA. Use of a novel polyp “ruler snare” improves estimation of colon polyp size. Gastrointest Endosc. 2016;83:812-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |