Published online Oct 27, 2024. doi: 10.4240/wjgs.v16.i10.3163
Revised: August 22, 2024
Accepted: August 30, 2024
Published online: October 27, 2024
Processing time: 141 Days and 23.8 Hours
The spleen is the most commonly injured solid organ in blunt abdominal trauma, and splenic pseudoaneurysm rupture is associated with a high risk of mortality. Nonoperative management has become the standard treatment for hemodynamically stable patients with splenic injuries. On the other hand, delayed splenic pseudoaneurysms can develop in any patient, and at present, there are no known risk factors that may reliably predict their occurrence. Furthermore, there is a lack of consensus regarding the most appropriate strategies for monitoring and mana
To determine the predictors of pseudo-aneurysm formation following splenic injury and develop follow-up strategies for early detection of pseudoaneurysms.
We retrospectively analyzed patients who visited the Level I Trauma Center bet
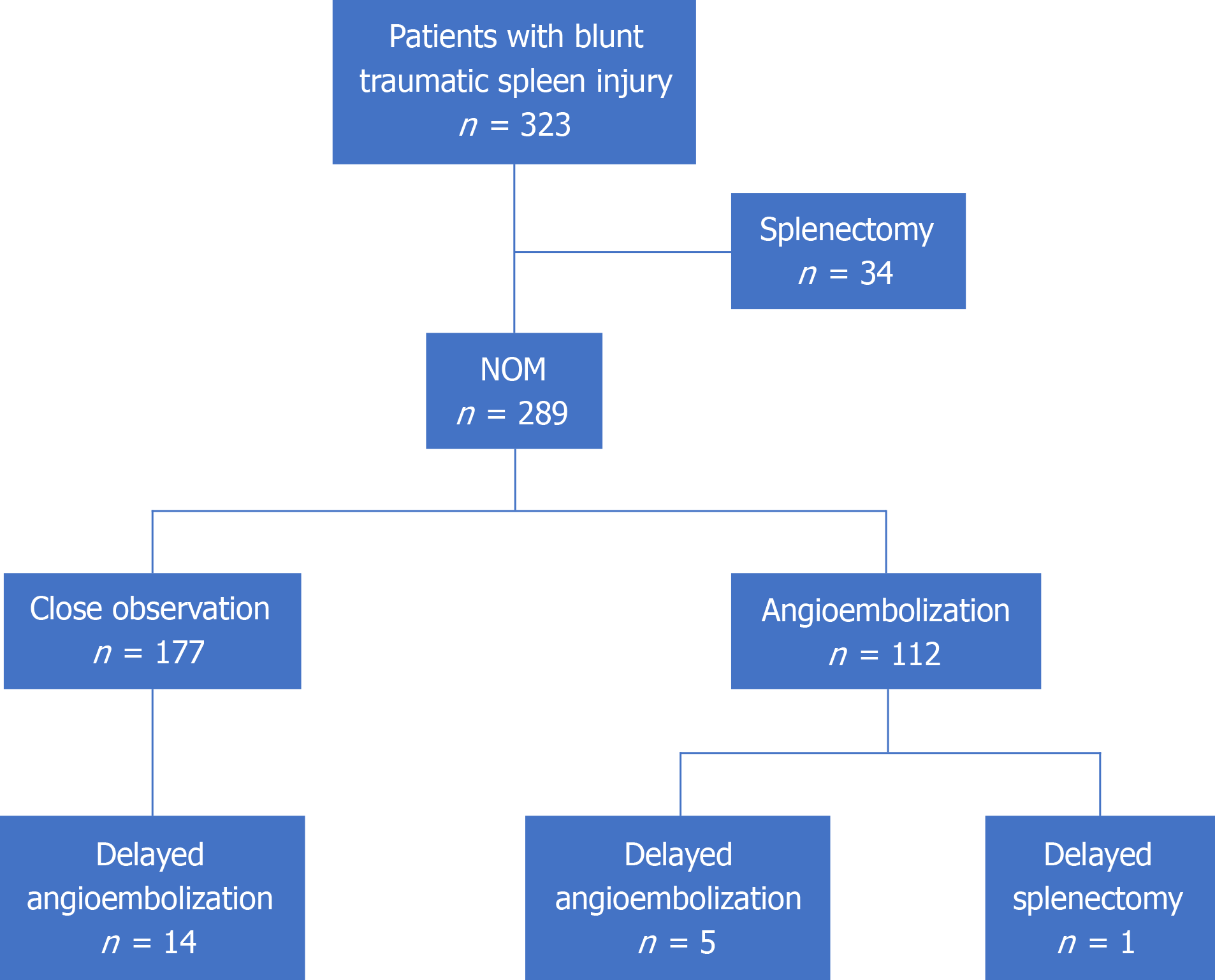
Using the American Association for the Surgery of Trauma spleen injury scale, the splenic injuries were categorized into the following order based on severity: Grade I (n = 57, 17.6%), grade II (n = 114, 35.3%), grade III (n = 89, 27.6%), grade IV (n = 50, 15.5%), and grade V (n = 13, 4.0%). Of a total of 323 patients, 35 underwent splenectomy and 126 underwent angioembolization. 19 underwent delayed angioembolization, and 5 under-went both initial and delayed angioembolization. In 14 patients who had undergone delayed angioembolization, no extravasation or pseudoaneurysm was observed on the initial computed tomography scan. There are no particular patient-related risk factors for the formation of a delayed splenic pseudoaneurysm, which can occur even in a grade I spleen injury or even 21 days after the injury. The mean detection time for a delayed pseudoaneurysm was 6.26 ± 5.4 (1-21, median: 6, inter
We recommend regular follow-up computed tomography scans, including an arterial and portal venous phase, at least 1 week and 1 month after injury in any grade of blunt traumatic spleen injury for the timely detection of delayed pseudoaneurysms.
Core Tip: Nonoperative management has become the standard treatment for hemodynamically stable patients with splenic injuries. On the other hand, delayed splenic pseudoaneurysms can develop in any patient, and at present, there are no known risk factors that may reliably predict their occurrence. There were also no statistically significant risk factors for delayed pseudoaneurysm formation in our study. We recommend regular follow-up computed tomography scans at least 1 week and 1 month after injury in any grade of blunt traumatic spleen injury.
- Citation: Cho SH, Kim GW, Hwang S, Lim KH. Follow-up strategy for early detection of delayed pseudoaneurysms in patients with blunt traumatic spleen injury: A single-center retrospective study. World J Gastrointest Surg 2024; 16(10): 3163-3170
- URL: https://www.wjgnet.com/1948-9366/full/v16/i10/3163.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i10.3163
The spleen is the most commonly injured solid organ in blunt abdominal trauma[1,2]. In addition, it is an organ with high vascularity, and splenic pseudoaneurysm rupture is associated with a high mortality rate[3]. With technological advan
The World Society of Emergency Surgery recommends splenic artery angioembolization to be performed as the first-line intervention for patients who have sustained splenic trauma and were treated with NOM, are hemodynamically stable, and have a CT scan showing arterial blush[1]. Moreover, World Society of Emergency Surgery recommends sele
Notably, delayed splenic pseudoaneurysms can develop in any patient, and at present, there are no known risk factors that may reliably predict their occurrence. Furthermore, there is a lack of consensus regarding the most appropriate strategies for monitoring and managing splenic injuries, especially lower-grade. Therefore, this study aimed to determine the predictors of pseudoaneurysm formation following splenic injury and develop follow-up strategies for early detection of pseudoaneurysms.
We retrospectively analyzed patients who visited the Level I Trauma Center between January 2013 and December 2022 and were diagnosed with spleen injuries after blunt abdominal trauma. All enrolled patients were diagnosed with splenic injury based on contrast-enhanced CT scan performed on the day of the hospital visit. The splenic injury grade was classified according to the American Association for the Surgery of Trauma (AAST) spleen injury scale, which is currently the most widely used grading system for splenic trauma[5].
The selected patients were divided into a splenectomy group and an NOM group according to the treatment used. The NOM group was further divided into a close observation group and an angioembolization group based on the immediate treatment used. In the NOM group, some patients underwent delayed splenectomy or angioembolization. The flowchart for the group classification of enrolled patients is shown in Figure 1. Data regarding the following characteristics for all patients were obtained from the hospital’s electronic medical records: Age, sex, injury severity score (ISS), AAST spleen injury scale, and the number of follow-up days to the CT scan. The study was reviewed and approved by the Institutional Review Board of the Kyungpook National University Hospital (Approval No. 2023-12-016).
Angioembolization was performed immediately when vascular lesions, such as blushing or pseudoaneurysms, were identified on the initial CT scan. If the patient’s hemodynamic status impeded angioembolization or surgery was wa
Patients were admitted to the trauma intensive care unit or general ward depending on their condition. Follow-up CT scans were routinely performed 1 week and 1 month later; occasionally, additional scans were performed at the phy
Initial blushing and initial pseudoaneurysm were defined as blood extravasation and pseudoaneurysm formation within the spleen on the first CT scan at admission. Initial angioembolization was defined as a procedure that was performed immediately after diagnosis. A delayed pseudoaneurysm was defined as a pseudoaneurysm that was not observed on the first CT scan but became visible on a CT scan performed after the first 24 hours. Similarly, angioembolization performed after 24 hours was defined as delayed angioembolization.
Categorical variables (sex and the AAST spleen injury scale) were presented as frequencies and percentages and com
Between January 2013 and December 2022, 323 patients, including 247 (76.5%) male and 76 (23.5%) female patients, were diagnosed with blunt traumatic spleen injuries. The mean age of these patients was 46.69 ± 21.16 (2-93) years. The most common causes of trauma were falls, motorcycle crash and motor vehicle crash (Table 1). Using the AAST spleen injury scale, the splenic injuries were categorized into the following order based on severity: Grade I (n = 57, 17.6%), grade II (n = 114, 35.3%), grade III (n = 89, 27.6%), grade IV (n = 50, 15.5%), and grade V (n = 13, 4.0%). As the AAST spleen injury scale increased, the ISS and the rates of angioembolization and splenectomy also increased gradually. However, in grade V patients, the rate of angioembolization and splenectomy was rather low. Out of 323 patients, angioembolization was performed in 126 (39%) patients and splenectomy was performed in 35 (10.8%) patients. The splenectomy group included patients in whom splenectomy was performed concomitantly with surgery because of other abdominal injuries (Table 2).
| Cause of trauma | Number of patients, n |
| Fall | 69 |
| Motorcycle crash | 69 |
| MVC | 63 |
| Pedestrian accident | 40 |
| Passenger injury | 32 |
| Bicycle crash | 18 |
| ETC | 32 |
| AAST grade | Number of patients, n | ISS, mean ± SD | NOM | Splenectomy, n (%) | |
| Close observation, n (%) | Angioembolization, n (%) | ||||
| I | 57 | 18.39 ± 9.96 | 47 (82.5) | 5 (8.8) | 5 (8.8) |
| II | 114 | 18.80 ± 10.7 | 84 (73.7) | 23 (20.2) | 7 (6.1) |
| III | 89 | 17.80 ± 10.22 | 25 (28.1) | 59 (66.3) | 5 (5.62) |
| IV | 50 | 21.60 ± 8.01 | 4 (8) | 36 (72) | 11 (22) |
| V | 13 | 27.23 ± 5.53 | 3 (23.1) | 3 (23.1) | 7 (53.85) |
Of the 126 patients who underwent angioembolization, 112 patients were performed as an initial angioembolization because they showed contrast blushing or pseudoaneurysm on their initial CT scan. Delayed angioembolization was performed in 19 patients. Among them, two patients had grade I injury, 6 had grade II, 8 had grade III, and 3 had grade IV injury. 14 of these patients had delayed pseudoaneurysm formation, although their first CT scans showed no contrast blushing, pseudoaneurysms, or arteriovenous fistulas. In addition, new bleeding lesions, which were identified during follow-up and required delayed angioembolization, were observed in five patients who had previously undergone initial angioembolization. Table 3 presents the characteristics of the 19 patients who developed delayed pseudoaneurysm.
| Age | Sex | AAST grade | ISS | Trauma cause | DPA, detection time, day |
| 33 | Female | I | 33 | Passenger injury | 16 |
| 42 | Male | I | 24 | Motorcycle crash | 8 |
| 34 | Female | II | 14 | MVC | 10 |
| 55 | Male | II | 22 | MVC | 5 |
| 55 | Female | II | 4 | Assault | 1 |
| 58 | Female | II | 6 | MVC | 3 |
| 64 | Male | II | 18 | Fall | 2 |
| 74 | Female | II | 22 | Passenger injury | 21 |
| 13 | Male | III | 13 | Pedestrian accident | 10 |
| 18 | Male | III | 5 | Passenger accident | 6 |
| 24 | Male | III | 14 | MVC | 2 |
| 37 | Male | III | 4 | Bicycle crash | 9 |
| 46 | Female | III | 25 | Passenger injury | 1 |
| 52 | Male | III | 8 | Motorcycle crash | 1 |
| 64 | Female | III | 22 | MVC | 6 |
| 66 | Male | III | 9 | Fall | 8 |
| 27 | Male | IV | 43 | Bicycle crash | 3 |
| 46 | Male | IV | 29 | Motorcycle crash | 6 |
| 66 | Male | IV | 27 | Pedestrian accident | 1 |
Statistical analysis was performed on 288 patients to determine the risk factors associated with the development of delayed pseudoaneurysms; 35 patients who had undergone an initial and delayed splenectomy were excluded. There was no statistically significant correlation between sex, the AAST spleen injury scale, and delayed pseudoaneurysm occur
| Delayed pseudoaneurysm | P value | |||
| None | Occurrence | |||
| Sex, n (%) | Male | 207 (94.5) | 12 (5.5) | 0.173 |
| Female | 62 (89.9) | 7 (10.1) | ||
| AAST grade, n (%) | I | 50 (96.2) | 2 (3.8) | 0.649 |
| II | 101 (94.4) | 6 (5.6) | ||
| III | 76 (90.5) | 8 (9.5) | ||
| IV | 36 (92.3) | 3 (7.7) | ||
| V | 6 (100) | 0 (0) | ||
| Age, years (mean ± SD) | 46.86 ± 21.51 | 46.00 ± 17.8 | 0.865 | |
| ISS (mean ± SD) | 18.62 ± 10.09 | 18.00 ± 10.87 | 0.798 | |
The spleen is the most commonly injured solid organ in blunt abdominal trauma[1,2]. Over the past few decades, subs
Contrast blushing is an important indication of angioembolization. However, even if contrast blushing is not noted on the first CT scan of a high-grade splenic injury, surgeons must not exclude the possibility of current bleeding[6]. There
The pathophysiology of delayed splenic pseudoaneurysm formation is unclear; however, it is believed that since the spleen is a hyper-vascular organ, the weakening of a vessel wall within the spleen caused by blunt trauma causes aneu
Currently, contrast-enhanced CT scan is the gold standard for diagnosing splenic pseudoaneurysms because of its sensitivity and widespread usage[3,4,9]. In particular, delayed-phase CT scan helps in differentiating patients with active bleeding from those with confined vascular injuries[6,13]. However, there is still a lack of comprehensive knowledge on the incidence and timing of pseudoaneurysm formation as well as the most optimum time to perform a follow-up CT scan[3,4,6,9,13-15]. Some reports recommend that a follow-up CT scan is not necessary in patients with low-grade splenic injuries[4,9]. Fata et al[16] reported that 85% of surgeons do not routinely perform follow-up CT scans on outpatients with spleen injuries. In contrast, some surgeons advocate that selective imaging follow-up must be practiced after discharge for patients with blunt splenic injuries treated with NOM only in the presence of risk factors for long-term complications and depending on the level of activity[1,4]. Although CT provides high-quality diagnostic information, many surgeons oppose routine CT repetition because it can be expensive, depending on the country’s environment, and involves expo
On the other hand, Savage et al[2] recommended that follow-up imaging should be performed even in patients with mild splenic injuries because some patients who did not undergo imaging follow-up had required a splenectomy. Mo
In our study, the splenic injury grade and delayed pseudoaneurysm occurrence showed no correlation. Therefore, we concur that imaging follow-up must be performed until the splenic injury is completely resolved, even in cases of low-grade spleen injuries. Muroya et al[9] published a retrospective review of patients with blunt injuries of the spleen treated with NOM between 2003 and 2010 at five trauma and critical care centers in Japan. Their study revealed the occurrence of delayed pseudoaneurysm in 16 out of 104 patients (15%); of these 16 patients, 7 had grade II splenic injury and 9 had grade III injury. The authors recommended that follow-up CT scan must be performed approximately 1 week after injury (the pseudoaneurysm was detected within a week in 15 out of 16 patients) and even in low-grade splenic injury (all delayed pseudoaneurysms were found in patients with a splenic injury grade of II or III)[9]. In our study, the higher the splenic injury grade, the higher the rate of initial angioembolization or splenectomy. Because almost all patients in grades IV and V either underwent angioembolization/splenectomy or were deceased, most delayed pseudoaneurysms were detected in splenic injury grades II and III. Weinberg et al[18] reported an incidence of 7.1% for delayed pseudoaneurysm formation after NOM in patients with splenic injuries, while Davis et al[19] reported this incidence to be 7.7%; in our study, this incidence was 6.6%.
Furthermore, Crawford et al[20] reported a case of delayed rupture of the spleen in a 22-year-old man 22 days after injury. Davies et al[21] also reported the case of a 15-year-old boy who died due to delayed splenic bleeding 18 days after being discharged because a pseudoaneurysm was not detected initially. In our study, 12 of the 19 patients were dia
First, this study used a retrospective study design to analyze patients with blunt traumatic splenic injury from a single trauma center. Second, we did not analyze the causality between injured spleen pathophysiology and delayed pseudoaneurysm formation. Third, the length of time to detect a delayed pseudoaneurysm does not exactly represent the timing of its formation. In addition, follow-up CT scans were not performed at the same time and for all patients. Lastly, angioembolization was performed in all delayed pseudoaneurysm cases considering that pseudoaneurysm would grow in size over time and the vessel wall would weaken, thereby increasing the possibility of rupture. Consequently, the prognosis of NOM for delayed pseudoaneurysm remains uncertain.
We recommend regular follow-up CT scans, including an arterial and portal venous phase, at least 1 week and 1 month after injury in any grade of blunt traumatic spleen injury for the timely detection of delayed pseudoaneurysms.
| 1. | Podda M, De Simone B, Ceresoli M, Virdis F, Favi F, Wiik Larsen J, Coccolini F, Sartelli M, Pararas N, Beka SG, Bonavina L, Bova R, Pisanu A, Abu-Zidan F, Balogh Z, Chiara O, Wani I, Stahel P, Di Saverio S, Scalea T, Soreide K, Sakakushev B, Amico F, Martino C, Hecker A, de'Angelis N, Chirica M, Galante J, Kirkpatrick A, Pikoulis E, Kluger Y, Bensard D, Ansaloni L, Fraga G, Civil I, Tebala GD, Di Carlo I, Cui Y, Coimbra R, Agnoletti V, Sall I, Tan E, Picetti E, Litvin A, Damaskos D, Inaba K, Leung J, Maier R, Biffl W, Leppaniemi A, Moore E, Gurusamy K, Catena F. Follow-up strategies for patients with splenic trauma managed non-operatively: the 2022 World Society of Emergency Surgery consensus document. World J Emerg Surg. 2022;17:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 2. | Savage SA, Zarzaur BL, Magnotti LJ, Weinberg JA, Maish GO, Bee TK, Minard G, Schroeppel T, Croce MA, Fabian TC. The evolution of blunt splenic injury: resolution and progression. J Trauma. 2008;64:1085-91; discussion 1091. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Corvino F, Giurazza F, Ierardi AM, Lucatelli P, Basile A, Corvino A, Niola R. Splenic Artery Pseudoaneurysms: The Role of ce-CT for Diagnosis and Treatment Planning. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 4. | Malloum Boukar K, Moore L, Tardif PA, Soltana K, Yanchar N, Kortbeek J, Champion H, Clement J. Value of repeat CT for nonoperative management of patients with blunt liver and spleen injury: a systematic review. Eur J Trauma Emerg Surg. 2021;47:1753-1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, Kaups K, Schuster K, Tominaga GT; AAST Patient Assessment Committee. Organ injury scaling 2018 update: Spleen, liver, and kidney. J Trauma Acute Care Surg. 2018;85:1119-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 307] [Article Influence: 51.2] [Reference Citation Analysis (0)] |
| 6. | Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, Moore EE, Reva V, Bing C, Bala M, Fugazzola P, Bahouth H, Marzi I, Velmahos G, Ivatury R, Soreide K, Horer T, Ten Broek R, Pereira BM, Fraga GP, Inaba K, Kashuk J, Parry N, Masiakos PT, Mylonas KS, Kirkpatrick A, Abu-Zidan F, Gomes CA, Benatti SV, Naidoo N, Salvetti F, Maccatrozzo S, Agnoletti V, Gamberini E, Solaini L, Costanzo A, Celotti A, Tomasoni M, Khokha V, Arvieux C, Napolitano L, Handolin L, Pisano M, Magnone S, Spain DA, de Moya M, Davis KA, De Angelis N, Leppaniemi A, Ferrada P, Latifi R, Navarro DC, Otomo Y, Coimbra R, Maier RV, Moore F, Rizoli S, Sakakushev B, Galante JM, Chiara O, Cimbanassi S, Mefire AC, Weber D, Ceresoli M, Peitzman AB, Wehlie L, Sartelli M, Di Saverio S, Ansaloni L. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg. 2017;12:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 271] [Cited by in RCA: 220] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 7. | Coccolini F, Fugazzola P, Morganti L, Ceresoli M, Magnone S, Montori G, Tomasoni M, Maccatrozzo S, Allievi N, Occhionorelli S, Kluger Y, Sartelli M, Baiocchi GL, Ansaloni L, Catena F. The World Society of Emergency Surgery (WSES) spleen trauma classification: a useful tool in the management of splenic trauma. World J Emerg Surg. 2019;14:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Sugg SL, Gerndt SJ, Hamilton BJ, Francis IR, Taheri PA, Rodriguez JL. Pseudoaneurysms of the intraparenchymal splenic artery after blunt abdominal trauma: a complication of nonoperative therapy and its management. J Trauma. 1995;39:593-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Muroya T, Ogura H, Shimizu K, Tasaki O, Kuwagata Y, Fuse T, Nakamori Y, Ito Y, Hino H, Shimazu T. Delayed formation of splenic pseudoaneurysm following nonoperative management in blunt splenic injury: multi-institutional study in Osaka, Japan. J Trauma Acute Care Surg. 2013;75:417-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Talwar A, Knight G, Al Asadi A, Entezari P, Chen R, Resnick S, Komanduri S, Gabr A, Thornburg B, Salem R, Riaz A. Post-embolization outcomes of splenic artery pseudoaneurysms: A single-center experience. Clin Imaging. 2021;80:160-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Therakathu J, Panwala HK, Bhargava S, Eapen A, Keshava SN, David D. Contrast-enhanced Computed Tomography Imaging of Splenic Artery Aneurysms and Pseudoaneurysms: A Single-center Experience. J Clin Imaging Sci. 2018;8:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Lim HJ. A review of management options for splenic artery aneurysms and pseudoaneurysms. Ann Med Surg (Lond). 2020;59:48-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Anderson SW, Varghese JC, Lucey BC, Burke PA, Hirsch EF, Soto JA. Blunt splenic trauma: delayed-phase CT for differentiation of active hemorrhage from contained vascular injury in patients. Radiology. 2007;243:88-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 14. | Boscak AR, Shanmuganathan K, Mirvis SE, Fleiter TR, Miller LA, Sliker CW, Steenburg SD, Alexander M. Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology. 2013;268:79-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 15. | Schellenberg M, Owattanapanich N, Emigh B, Nichols C, Dilday J, Ugarte C, Onogawa A, Matsushima K, Martin MJ, Inaba K. Pseudoaneurysms after high-grade blunt solid organ injury and the utility of delayed computed tomography angiography. Eur J Trauma Emerg Surg. 2023;49:1315-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Fata P, Robinson L, Fakhry SM. A survey of EAST member practices in blunt splenic injury: a description of current trends and opportunities for improvement. J Trauma. 2005;59:836-41; discussion 841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Norotsky MC, Rogers FB, Shackford SR. Delayed presentation of splenic artery pseudoaneurysms following blunt abdominal trauma: case reports. J Trauma. 1995;38:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Weinberg JA, Lockhart ME, Parmar AD, Griffin RL, Melton SM, Vandromme MJ, McGwin G Jr, Rue LW 3rd. Computed tomography identification of latent pseudoaneurysm after blunt splenic injury: pathology or technology? J Trauma. 2010;68:1112-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Davis KA, Fabian TC, Croce MA, Gavant ML, Flick PA, Minard G, Kudsk KA, Pritchard FE. Improved success in nonoperative management of blunt splenic injuries: embolization of splenic artery pseudoaneurysms. J Trauma. 1998;44:1008-13; discussion 1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 213] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 20. | Crawford RS, Tabbara M, Sheridan R, Spaniolas K, Velmahos GC. Early discharge after nonoperative management for splenic injuries: increased patient risk caused by late failure? Surgery. 2007;142:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Davies DA, Fecteau A, Himidan S, Mikrogianakis A, Wales PW. What's the incidence of delayed splenic bleeding in children after blunt trauma? An institutional experience and review of the literature. J Trauma. 2009;67:573-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |