Published online Sep 27, 2023. doi: 10.4240/wjgs.v15.i9.2083
Peer-review started: May 25, 2023
First decision: June 19, 2023
Revised: June 27, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: September 27, 2023
Processing time: 120 Days and 0.2 Hours
Gallstone ileus following one anastomosis gastric bypass (OAGB) is an exceptionally rare complication. The presented case report aims to highlight the unique occurrence of this condition and its surgical management. Understanding the clinical presentation, diagnostic challenges and successful surgical inter
We present a case report of gallstone ileus following OAGB and discuss its diagnosis and surgical management. A 66-year-old female with a history of OAGB presented to the emergency room with symptoms of small bowel obstru
Gallstone ileus should be considered as a possible complication after OAGB, and prompt surgical intervention is usually required for its management. This case report contributes to the limited existing literature, providing insights into the management of this uncommon complication.
Core Tip: Gallstone ileus is a rare but serious complication that can occur after bariatric surgery, including one anastomosis gastric bypass (OAGB). Prompt diagnosis and appropriate surgical management are crucial for successful outcomes. In this case report, we present a rare instance of gallstone ileus after OAGB, highlighting the importance of considering this condition in patients presenting with small bowel obstruction symptoms post-bariatric surgery. A laparoscopically assisted enterolithotomy was performed, leading to the successful extraction of the gallstone and subsequent resolution of symptoms. Surgeons should be aware of the increased risk of cholelithiasis after bariatric surgery and consider preventive measures or early intervention to minimize the occurrence of gallstone-related complications.
- Citation: El Feghali E, Akel R, Chamaa B, Kazan D, Chakhtoura G. Surgical management of gallstone ileus after one anastomosis gastric bypass: A case report. World J Gastrointest Surg 2023; 15(9): 2083-2088
- URL: https://www.wjgnet.com/1948-9366/full/v15/i9/2083.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i9.2083
One anastomosis gastric bypass (OAGB) or mini bypass was first performed by Dr. Robert Rutledge in 1997[1]. It is both a restrictive and malabsorptive bariatric surgical procedure for the treatment of morbid obesity. It was developed as a faster and simpler alternative to the Roux en Y gastric bypass and is the fourth most performed bariatric technique in Europe and in Asia[2]. It is an effective surgical technique in terms of both weight loss and the resolution of comorbidities[3]. Nevertheless, like any other surgical procedure, OAGB can be associated with potential complications such as anastomotic leaks in 0.5 to 5.0 percent of cases, bleeding 0.2 to 2.0 per cent, nutritional deficiencies 5 to 50 per cent[4]. In addition, intestinal obstruction or occlusion is a possible complication after the OAGB with an incidence of 1 to 10 per cent[5] causing symptoms such as abdominal pain, nausea and vomiting and constipation. The most common etiologies of intestinal occlusion post-OAGB include internal hernias, adhesions, strictures and bowel kinking and/or twisting. In our case report, we are going to be present a rare cause of intestinal occlusion post-OAGB, the gallstone ileus (GI).
A 66-year-old female presented to the ER for abdominal pain and vomitting.
She had a 4-d history of food intolerance with post-prandial vomiting and diffuse colic type abdominal pain, her bowel movements were maintained. She denied having previously experienced similar symptoms or symptoms suggesting of cholecystitis during her post-operative interval.
She is known to have bipolar disease treated with Perphrenazine 8 mg and known to be a 5 pack/year smoker. She was operated of OAGB 6 years ago for morbid obesity [body mass index (BMI): 66.7 kg/m2]. Previous comorbidities that included hypertension and diabetes mellitus were rectified after her weight loss of 90 Kg (BMI: 26.66 kg/m2). Previous surgical interventions include 2 C-section deliveries.
She has no significant family history.
On physical examination, her abdomen was soft with mild tenderness in the lower right quadrant. She had a supra-umbilical hernia from her previous intervention.
Her labs showed a mild hyper-leukocytosis white blood cell 12000 and C-reactive protein level was 80.8, her liver enzymes were in the normal range.
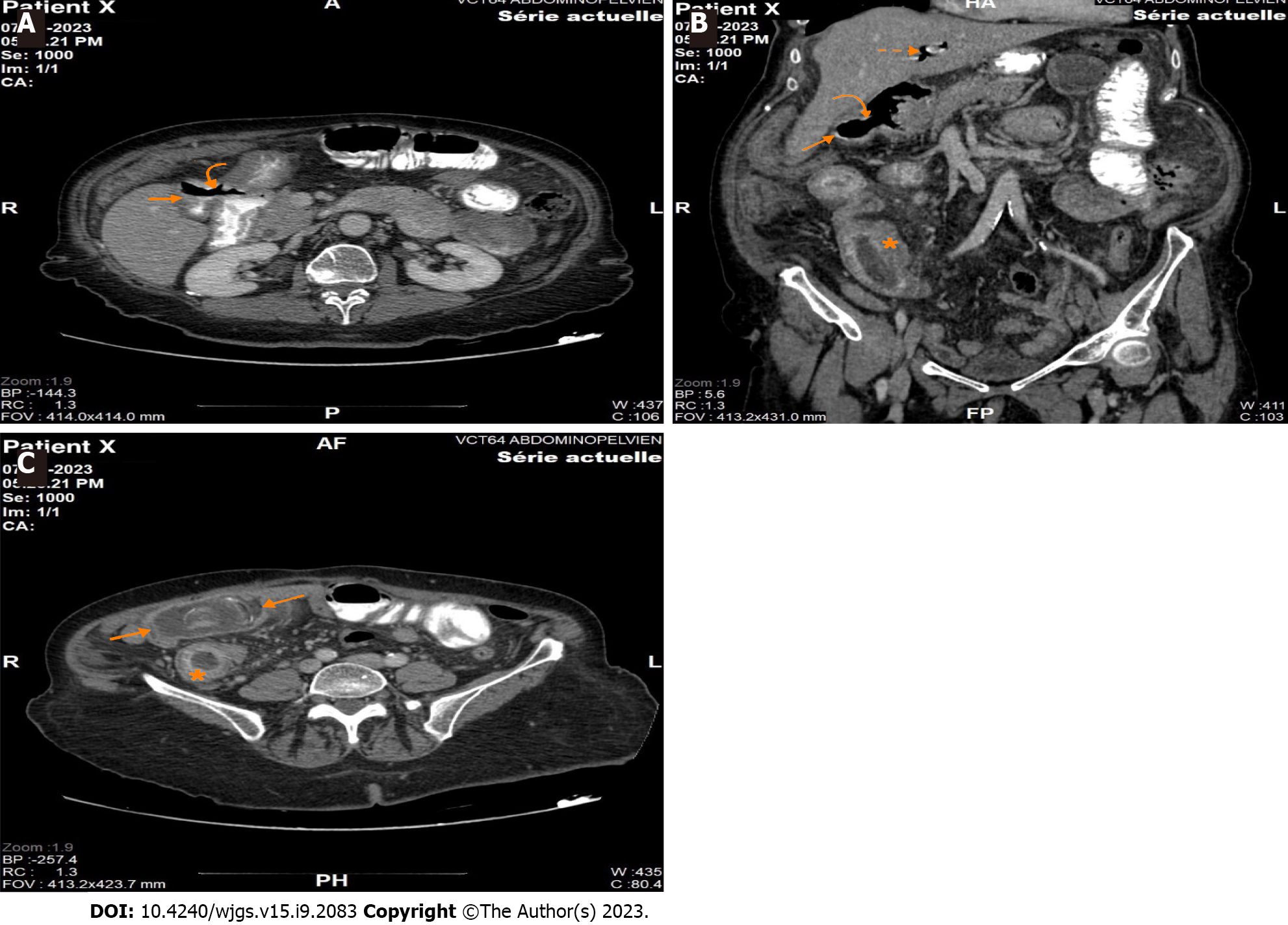
An abdomino-pelvic computed tomography scan with injection and ingestion of contrast was ordered (Figure 1). It showed a fistulous tract between the gallbladder and the duodenal bulb, extending over 15 mm. The fistula was confirmed with the leakage of the ingested contrast in the lumen of the gallbladder, which was not distended and contained an air-fluid level. It was associated with pneumobilia and small bowel dilation of 42 mm in diameter, with an intestinal segment in the right lower quadrant showing parietal thickening and submucosal edema upstream of a transition zone located at the level of the right iliac fossa, downstream of a probable oval intraluminal calculus of 45 mm. The previous findings evoking a GI with a probable gallstone located at the level of the efferent alimentary loop. It is associated with a trabeculation of the fat at the level of the two flanks, especially on the right, with perihepatic and pelvic ascites of low abundance. Sequelae of gastric surgery with gastro-jejunal anastomosis (Roux en Omega) was identified.
She was thus admitted for adequate treatment of her GI.
After establishing the diagnosis of GI and acquiring the written consent of the patient, she was transferred to the operating room for a diagnostic laparoscopy and subsequent enterolithotomy. A nasogastric tube was inserted and she was adequately hydrated.
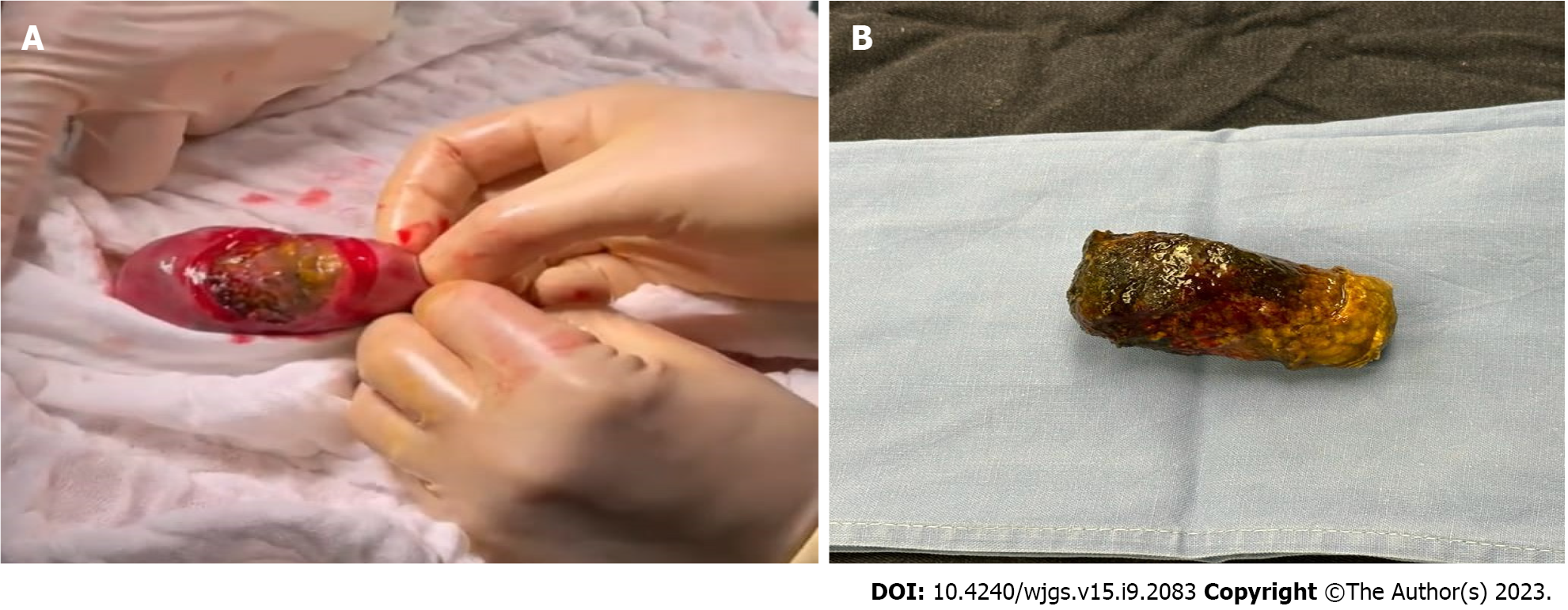
Open coelioscopy was performed and a 10 mm port was introduced. Pneumoperitoneum was created with a PCO2 of 12 mmHg. Two para-umbilical 5 mm ports were introduced under vision. There were multiple adhesions over the previous gastro-jejunal anastomosis and over the gallblader. The entero-biliary fistulae were not visualized, even after adhesyolysis. The afferent biliopancreatic loop was normal in diameter whereas the efferent alimentary loop was distended. The small bowel was run downwards until the obstructed ileal loop was identified. A 5 cm para-umbilical midline incision was made and the bowel segment was exteriorized. A horizontal enterotomy was performed to allow the extraction of an ovoid shaped yellow-brown stone measuring 5 cm × 3 cm × 1 cm approximately (Figure 2). The enterotomy was closed transversely with a double layer of absorbable sutures, and the small bowel was returned to the abdomen. The incision was approximated with non-absorbable monofilament sutures.
The patient’s recovery was uneventful with return of bowel function on postoperative day two and diet advanced as tolerated. The patient was discharged home in improved condition on postoperative day four.
Rapid weight loss after bariatric surgery is associated with an increase in cholelithiasis, especially when the weight loss is greater than 25 per cent of the preoperative weight[6] with 38 per cent of patients developing gallstones within 6 mo, of which, 41 per cent will ultimately develop symptomatic cholelithiasis[7].
Gallstone ileus or Bouveret’s Syndrome is a rare but serious complication of cholelithiasis as it occurs in 0.3 per cent of patients[8,9]. It results when a supracentimetric gallstone, which was formed during a medically treated or neglected cholecystitis, migrates from the gallbladder to the bowel through a biliary enteric fistula, the most common being a cholecystoduodenal fistula, and causes an obstruction, in more than 70% of cases at the level of the terminal ileum[10].
GI is considered to be implicated in 1 to 4 per cent of mechanical bowel obstruction, and accounts for a quarter of non-strangulated small bowel obstruction in patients above the age of 65 years, with a mortality rate between 15 to 18 per cent[9] with a female to male ratio of 3.5-6.1[11].
The diagnosis of GI is both clinical and radiological. GI has nonspecific symptoms such as nausea and/or vomiting associated with abdominal pain, bloating and constipation. The abdominal computed-tomography scan is the gold standard to establish the diagnosis. Rigler’s triad of pneumobilia with small bowel obstruction caused by an ectopic gallstone within the bowel is observed in 40 to 50 per cent of cases[12].
Conservative measures such as nil per os status, nasogastric tube decompression with adequate intravenous hydration may be sufficient in select clinically stable patients with partial bowel obstruction and stones < 2 cm in size[8]. However, GI often requires urgent surgical management, laparoscopically in 10% of cases[13], which allows delineation of the anatomy with decreased bowel manipulation and subsequent safe stone extraction and reduced risk of intestinal content spillage.
The choice of surgical intervention is a subject of controversy[14]. A one or two stage procedure may be proposed: either enterolithotomy alone or enterolithotomy with cholecystectomy and eventual repair of the biliary fistula[15]. Nevertheless, the one stage approach is discouraged in view of the significant mortality (16.9%) compared with the two staged procedure (11.7%)[9]. In addition, laparoscopically assisted enterolithotomy has been credited with a favorable impact as it can be recommended for both diagnosis and treatment[16]. Prevention of symptomatic cholelithiasis after gastric bypass could be achieved by either prophylactic cholecystectomy or administration of ursodiol. In the one hand, prophylactic cholecystectomy during gastric bypass is a debatable subject. Its supporters argue that it is safe and would prevent both the morbidity associated with symptomatic cholelithiasis and a subsequent operation. Those who oppose to it cite that the safety of secondary cholecystectomy with an increase in operative time and length of stay do not justify the prophylactic cholecystectomy[17]. In the other hand, administration of a daily dose of 600 mg of ursodiol after gastric bypass was associated with a significant reduction in the incidence of cholelithiasis compared with placebo at 6 mo (2% vs 32%)[18].
To our knowledge, this is the first documented report of GI in a patient after OAGB. The GI diagnosis was established after correlation of the clinical and radiological findings of the patient. The fact that the patient presented to the emergency department with small bowel obstruction symptoms and the CT-scan confirmed the GI diagnosis with the presence of Rigler’s triad previously discussed. The decision was to perform a two-staged procedure. Laparoscopically assisted enterolithotomy was preformed because it is in our opinion the safest and fastest therapeutic modality. At our institution, our current practice is to perform the OAGB without prophylactic cholecystectomy given that, if needed, a laparoscopic cholecystectomy is feasible in the case of a symptomatic cholelithiasis.
In conclusion, the incidence of cholelithiasis significantly increases after bariatric surgery and may lead to serious complications such as gallstone ileus, which require further operations.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Lebanon
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dilek ON, Turkey; Wang ZF, China S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 420] [Cited by in RCA: 428] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 2. | Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obes Surg. 2015;25:1822-1832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1221] [Cited by in RCA: 1165] [Article Influence: 116.5] [Reference Citation Analysis (1)] |
| 3. | Abou Ghazaleh R, Bruzzi M, Bertrand K, M'harzi L, Zinzindohoue F, Douard R, Berger A, Czernichow S, Carette C, Chevallier JM. Is Mini-Gastric Bypass a Rational Approach for Type-2 Diabetes? Curr Atheroscler Rep. 2017;19:51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Musella M, Susa A, Manno E, De Luca M, Greco F, Raffaelli M, Cristiano S, Milone M, Bianco P, Vilardi A, Damiano I, Segato G, Pedretti L, Giustacchini P, Fico D, Veroux G, Piazza L. Complications Following the Mini/One Anastomosis Gastric Bypass (MGB/OAGB): a Multi-institutional Survey on 2678 Patients with a Mid-term (5 Years) Follow-up. Obes Surg. 2017;27:2956-2967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 127] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 5. | Scavone G, Caltabiano DC, Gulino F, Raciti MV, Giarrizzo A, Biondi A, Piazza L, Scavone A. Laparoscopic mini/one anastomosis gastric bypass: anatomic features, imaging, efficacy and postoperative complications. Updates Surg. 2020;72:493-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Li VK, Pulido N, Fajnwaks P, Szomstein S, Rosenthal R, Martinez-Duartez P. Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc. 2009;23:1640-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 141] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 7. | Karadeniz M, Görgün M, Kara C. The evaluation of gallstone formation in patients undergoing Roux-en-Y gastric bypass due to morbid obesity. Ulus Cerrahi Derg. 2014;30:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Duzgun AP, Ozmen MM, Ozer MV, Coskun F. Internal biliary fistula due to cholelithiasis: a single-centre experience. World J Gastroenterol. 2007;13:4606-4609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | BUETOW GW, CRAMPTON RS. Gallstone ileus. A report of 23 cases. Arch Surg. 1963;86:504-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Trump D. Commentary on: "Randomized, controlled, double-blind, cross-over trial assessing treatment preference for pazopanib versus sunitinib in patients with metastatic renal cell carcinoma: PISCES study." Escudier B, Porta C, Bono P, Powles T, Eisen T, Sternberg CN, Gschwend JE, De Giorgi U, Parikh O, Hawkins R, Sevin E, Négrier S, Khan S, Diaz J, Redhu S, Mehmud F, Cella D. Bernard Escudier, Institut Gustave Roussy, Villejuif; Emmanuel Sevin, Centre François Baclesse, Caen; Sylvie Négrier, Leon Berard Cancer Center, Lyon, France; Camillo Porta, Fondazione Istituto di Ricovero e Cura a Carattere Scientifico (IRCCS) Policlinico S. Matteo, Pavia; Cora N Sternberg, San Camillo Forlanini Hospital, Rome; Ugo De Giorgi, IRCCS Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori, Meldola, Italy; Petri Bono, Helsinki University Central Hospital, Helsinki, Finland; Thomas Powles, Barts Experimental Cancer Medicine Centre, Barts Cancer Institute, Queen Mary University of London, London; Tim Eisen, Cambridge University Health Partners, Cambridge; Omi Parikh, Royal Preston Hospital, Lancashire; Robert Hawkins, Christie Cancer Research UK, Manchester; Sadya Khan, Jose Diaz, and Faisal Mehmud, GlaxoSmithKline, Uxbridge, United Kingdom; Jürgen E Gschwend, Klinikum Rechts der Isar der Technischen Universität München, Munich, Germany; Suman Redhu, GlaxoSmithKline, Collegeville, PA; David Cella, Northwestern University Feinberg School of Medicine, Chicago, IL.: J Clin Oncol. 2014 May 10;32(14):1412-1418; doi: 10.1200/JCO.2013.50.8267. [Epub 2014 Mar 31]. Urol Oncol. 2016;34:251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Micheletto G, Danelli P, Morandi A, Panizzo V, Montorsi M. Gallstone ileus after biliointestinal bypass: report of two cases. J Gastrointest Surg. 2013;17:2162-2165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Yu CY, Lin CC, Shyu RY, Hsieh CB, Wu HS, Tyan YS, Hwang JI, Liou CH, Chang WC, Chen CY. Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol. 2005;11:2142-2147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 115] [Cited by in RCA: 126] [Article Influence: 6.3] [Reference Citation Analysis (2)] |
| 13. | Nuño-Guzmán CM, Marín-Contreras ME, Figueroa-Sánchez M, Corona JL. Gallstone ileus, clinical presentation, diagnostic and treatment approach. World J Gastrointest Surg. 2016;8:65-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 130] [Cited by in RCA: 153] [Article Influence: 17.0] [Reference Citation Analysis (3)] |
| 14. | Lê P, Chambon H, Madeuf E. [Gallstone ileus]. J Chir (Paris). 2003;140:169-170. [PubMed] |
| 15. | Doko M, Zovak M, Kopljar M, Glavan E, Ljubicic N, Hochstädter H. Comparison of surgical treatments of gallstone ileus: preliminary report. World J Surg. 2003;27:400-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Moberg AC, Montgomery A. Laparoscopically assisted or open enterolithotomy for gallstone ileus. Br J Surg. 2007;94:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Hamad GG, Ikramuddin S, Gourash WF, Schauer PR. Elective cholecystectomy during laparoscopic Roux-en-Y gastric bypass: is it worth the wait? Obes Surg. 2003;13:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 18. | Sugerman HJ, Brewer WH, Shiffman ML, Brolin RE, Fobi MA, Linner JH, MacDonald KG, MacGregor AM, Martin LF, Oram-Smith JC. A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Am J Surg. 1995;169:91-6; discussion 96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 226] [Article Influence: 7.5] [Reference Citation Analysis (0)] |