Published online Sep 27, 2023. doi: 10.4240/wjgs.v15.i9.1858
Peer-review started: June 9, 2023
First decision: July 18, 2023
Revised: July 20, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: September 27, 2023
Processing time: 104 Days and 21.4 Hours
Hepatic ischemia-reperfusion syndrome has been the subject of intensive study and experimentation in recent decades since it is responsible for the outcome of several clinical entities, such as major hepatic resections and liver transplantation. In addition to the organ’s post reperfusion injury, this syndrome appears to play a central role in the dysfunction of distant tissues and systems. Thus, continuous research should be directed toward finding effective therapeutic options to improve the outcome and reduce the postoperative morbidity and mortality rates. Treprostinil is a synthetic analog of prostaglandin I2, and its experimental administration has shown encouraging results. It has already been approved by the Food and Drug Administration in the United States for pulmonary arterial hypertension and has been used in liver transplantation, where preliminary encouraging results showed its safety and feasibility by using continuous intravenous administration at a dose of 5 ng/kg/min. Treprostinil improves renal and hepatic function, diminishes hepatic oxidative stress and lipid peroxidation, reduces hepatictoll-like receptor 9 and inflammation, inhibits hepatic apoptosis and restores hepatic adenosine triphosphate (ATP) levels and ATP synthases, which is necessary for functional maintenance of mitochondria. Treprostinil exhibits vasodilatory properties and antiplatelet activity and regulates proinflammatory cytokines; therefore, it can potentially minimize ischemia-reperfusion injury. Additionally, it may have beneficial effects on cardiovascular parameters, and much current research interest is concentrated on this compound.
Core Tip: End-stage liver disease is one of the leading causes of morbidity and mortality worldwide. The role of liver transplantation and liver resection in malignant disease has changed over the last decades with the evolution of high-risk surgical techniques and the great improvement in long-term survival. However, hepatic ischemia-reperfusion syndrome remains a significant clinical problem, as it is the main reason for postoperative liver failure and multiple organ dysfunction. Treprostinil is a synthetic analog of prostaglandin I2 with potential protective effects against ischemia-reperfusion injury. We herein discuss the effect of hepatic ischemia-reperfusion syndrome on the cardiovascular system and the role of treprostinil as a new promising therapeutic option.
- Citation: Mouratidou C, Pavlidis ET, Katsanos G, Kotoulas SC, Mouloudi E, Tsoulfas G, Galanis IN, Pavlidis TE. Hepatic ischemia-reperfusion syndrome and its effect on the cardiovascular system: The role of treprostinil, a synthetic prostacyclin analog. World J Gastrointest Surg 2023; 15(9): 1858-1870
- URL: https://www.wjgnet.com/1948-9366/full/v15/i9/1858.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i9.1858
Hepatic ischemia-reperfusion syndrome has been the subject of intense study and experimentation in recent decades since it is responsible for the outcome of several clinical events, such as hemorrhagic shock, major hepatic resections, Budd-Chiari syndrome and some types of hepatotoxicity[1-3]. Worldwide, end-stage liver disease is a common cause of morbidity and mortality, and liver transplantation remains the gold standard therapy for these patients. Nevertheless, prolonged exposure of the graft to cold and warm ischemia has a direct risk of serious postoperative complications, such as poor early graft function and primary nonfunction[4,5].
The complex blood supply in combination with the increased metabolic activity of the liver and its involvement in homeostasis, detoxification, protein synthesis, energy storage and immunity processes render the organ extremely sensitive to circulatory disorders. Liver ischemia-reperfusion syndrome remains a major cause of worse postoperative clinical outcomes. The pathophysiological changes do not pertain to single organ damage but also to a complex systemic process that affects other structures and tissues, causing a cascade of multiple organ dysfunction[6-9].
The responsible mechanisms are exceedingly complicated and involve numerous factors, including mediators, cytokines, adhesion molecules, vasoactive agents and reactive oxygen species. During an ischemic period, several functional processes take place at the cellular level and stimulate cell injury[9,10]. The exposure of hepatocytes to low oxygen levels results in changes in intracellular pH and a decrease in adenosine triphosphate (ATP) production, thereby attenuating the intrahepatic energy content[11]. Excessive production of reactive oxygen species and reactive nitrogen species in mitochondria and intracellular calcium overload promote organelle destruction and cell death. Innate immunological processes involve the activation of liver Kupffer cells; the accumulation of circulating lymphocytes, neutrophils, platelets and monocytes; and hepatic macrophage polarization and differentiation[12-14]. In this respect, Kupffer cells produce reactive oxygen species, interleukin (IL)-1, and tumor necrosis factor (TNF)-α, thereby triggering the recruitment of CD4+ T lymphocytes. In turn, activated CD4+ T cells can trigger Kupffer cells, leading to aggravation of the inflammatory response. Concurrently, Kupffer cells may have a protective role by producing anti-inflammatory IL-10 and suppressing the expression of proinflammatory factors, such as TNF-α, IL-1β, interferon-γ, and IL-2, and adhesion molecules, such as intercellular adhesion molecule 1[15,16]. Disrupted liver metabolism elicits an endogenous inflammatory cascade, which includes excessive cytokine and chemokine production, the release of adhesive molecules and caspase-1 activation[17,18]. Blood flow restoration and re-exposure of ischemic hepatocytes to high oxygen level conditions contributes to further hepatocellular damage, mediated by reactive oxygen species generation[19]. An inflammatory outbreak of hepatic ischemia-reperfusion has been found to initiate a series of pleiotropic mitogen-activated protein kinase (MAPK) cascades. Among them, the activated P38 and c-Jun N-terminal kinase (JNK) cascades are most involved in the pathways of apoptotic or autophagic hepatic cell death[20,21]. Notably, current evidence suggests that the MAPK, mammalian target of rapamycin and nuclear factor kappa B (NF-κB) inflammatory signals are adjusted by tripartite motif containing protein 37, which plays important role in exacerbation of hepatic ischemia-reperfusion injury by directly interacting with TNF receptor-associated factor 6 (TRAF6)[22]. Cellular damage has been shown to be promoted by the downregulation of microRNAs (miRNAs), which are small, single-stranded, noncoding RNA molecules. Specifically, suppression of miRNA-142-3p, miRNA-146a, miRNA-200c, and miRNA-34a is suggested to worsen the condition of hepatic ischemia-reperfusion injury, while the inhibition of miR-450b-5p has the opposite response[23,24]. On the other hand, miR-125b attenuates hepatic ischemia-reperfusion injury by suppressing TRAF6 and NF-κB signal pathways[25]. In general, long non-coding RNA and miRNAs regulatory networks mediate the pathological progression of hepatic ischemia-reperfusion injury through mutual activation and interference[26].
Hepatic ischemia-reperfusion syndrome is associated with several vascular disorders, such as increased vascular permeability, endothelial cell edema and loss of homeostasis between vasoconstricting and vasodilating factors. Accumulated neutrophils form neutrophil extracellular traps (NETs) that have been shown to play a significant role in the interactions with platelets and are involved in pro-coagulation mechanisms in a variety of infectious and sterile inflammatory processes. A recent study demonstrated that hepatic ischemia-reperfusion leads to a NET-mediated hypercoagulable state and subsequent organ injury through microvascular immuno thrombi formation[27]. Further liver microcirculatory milieu obstruction results in deterioration of ischemic hepatocellular damage and cell death. Although hepatic cell injury appears to progress primarily via the lytic necrosis pathway, it seems that more complex, often complementary or overlapping mechanisms of programmed cell death occur based on the presence or absence of damage-associated molecular patterns (DAMPs). These mechanisms can be categorized into inflammatory, such as necrosis, necroptosis, pyroptosis, and ferroptosis, and noninflammatory subtypes, such as apoptosis[13,28-30]. In conclusion, the hepatic ischemia-reperfusion mechanisms are summarized in Table 1.
| Primary mechanisms | Subsequent reactions | Final outcomes |
| Metabolism disorders | Systemic inflammatory response syndrome, multiple organ dysfunction syndrome | |
| Anaerobic glycolysis | Mitochondria dysfunction | |
| ATP production | Cellular immunity | |
| Lactic acid and toxic acidic metabolites | Cell injury | |
| Reactive oxygen species | Programmed cell death and apoptosis | |
| Intracellular calcium overload | Microcirculatory dysfunction | |
| Microcirculatory system disorders | ||
| Vasoconstriction | ||
| Obstruction | Microcirculatory dysfunction | |
| Apoptosis of sinusoidal endothelial cells | Vascular permeability | |
| Expression of adhesion molecules | Endothelial cells oedema | |
| Ischemic injury | ||
| Neutrophil accumulation | ||
| Immune system disorders | ||
| Kupffer cells activation | ||
| Neutrophils activation | ||
| Production of pro- and anti-inflammatory cytokines | Excessive inflammatory process | |
| Accumulation of circulating lymphocytes, platelets and monocytes | Anti-inflammatory response | |
| Recruitment of CD4+ T lymphocytes | ||
| Gene expression | ||
| Imbalance in mRNAs expression | Cell damage | |
| Programmed cell death | Necrosis, apoptosis, necroptosis, pyroptosis, ferroptosis |
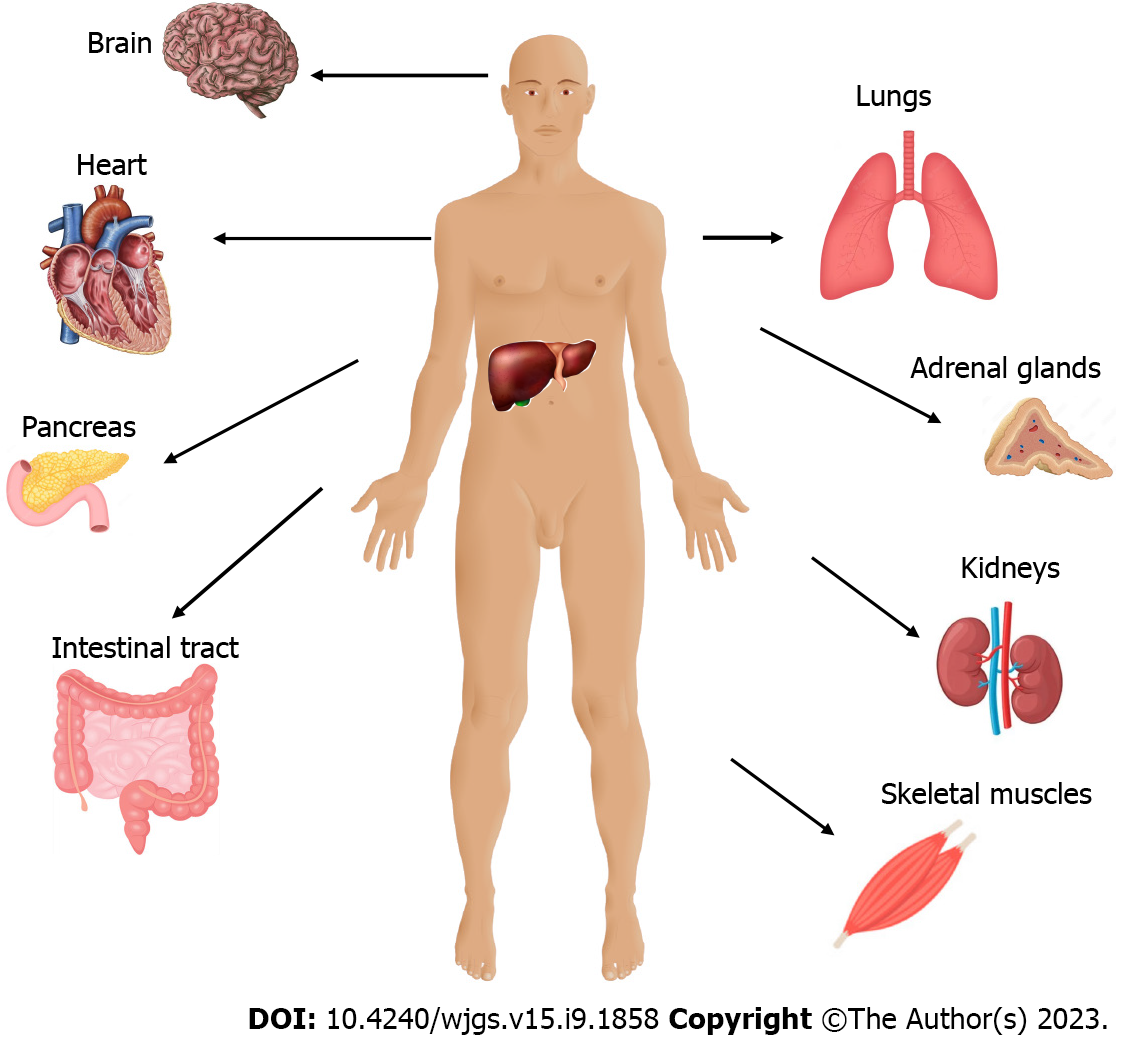
Severe hepatic ischemia-reperfusion injury does not constitute only a local phenomenon. It is characterized by a widespread systemic sterile inflammatory response with the accumulation of inflammatory cells in distant organs. Reactive oxygen radicals that are released following ischemic hepatocyte reperfusion promote systemic oxidative stress, resulting in remote organ damage[31-35]. In addition, platelet aggregation induces a procoagulant state and associated ubiquitous platelet-rich microvascular thrombus formation. Systemic NET-mediated hypercoagulability leads to remote organ injury through platelet toll-like receptor 4 (TLR4)-dependent signaling pathways[36]. These underlying mechanisms are responsible for the dysfunction of other organs, including the lung, kidney, intestine, pancreas, brain, and myocardium (as shown in Figure 1)[1,37,38]. The resulting multiple organ dysfunction syndrome occurs as a progressive, complex and dynamic process with a variable extent of organ failure and a direct deteriorating effect on survivorship[39].
Multiple organ dysfunction is a major complication of acute liver failure. The incidence of this particularly severe condition is approximately 1-8 cases per million inhabitants, and it is responsible for 6% of deaths due to liver disease and up to 7%-8% of liver transplants[40]. Although there are several reports of acute liver failure cases followed by myocardial involvement, the direct effects of hepatic ischemia-reperfusion syndrome on the myocardium have not been analyzed completely. Significantly elevated cardiac troponin I and creatine phosphokinase myocardial band (CK-MB) values have been associated with increased mortality, while the incidence of major cardiovascular events is undoubtedly higher in patients with acute liver failure[1,30,41]. Troponin I is a sensitive and myocardium-selective biomarker with both prognostic and diagnostic value. Troponin has become ingrained in the Universal Definition of Acute Myocardial Infarction but may also be detected in stable chronic conditions[42]. However, there is a high prevalence of elevated troponin in noncardiac clinical conditions, such as myocarditis, pulmonary embolism, acute heart failure, septic shock, and drug-induced cardiotoxicity, as well as after interventional procedures such as coronary angioplasty and electrical cardioversions. Thus, measurement of troponin elevation, especially with high-sensitivity assays, allows detection of clinical cases with nonacute coronary syndrome-mediated myocardial injury[43,44]. CK-MB is also preferred in particular situations, specifically in the diagnosis of acute myocardial infarction and cardiac injury evaluation. Although it has limitations in terms of early diagnosis, elevated CK-MB levels reveal myocardial damage secondary to some noncardiac conditions[45,46].
Clinical and pathophysiological variability in the remote organ impairment following acute liver failure is a result of the complicated interactions. Mitochondrial dysfunction and impaired ATP production are characteristic features and lead to energy balance disruption. As a consequence, parenchymal cells are forced to alter their metabolic activity to maintain their energy provision by enhancing proteolysis and lipolysis[47]. Pathogen-associated molecular patterns (PAMPs) and DAMPs released by damaged cells reinforce the systemic immune response and trigger cell death[48,49].
Severe circulatory disturbances are also observed in patients with acute liver failure, regardless of the cause of liver disease. Hyperdynamic circulation is characterized by markedly elevated cardiac output and low systemic vascular resistance due to peripheral vasodilation. These pathophysiological cardiovascular changes are similar to those seen in patients with septic shock[50]. Changes in the microcirculation during acute liver failure have also been described. Intrahepatic and systemic microcirculation abnormalities include vasoconstriction, precapillary shunt formation and reduced blood flow resulting in loss of multiorgan function[51].
In some experimental models, increased cardiac enzyme levels and histopathological myocardial tissue damage were not attributed only to metabolic stress and hemodynamic instability. Other complex mechanisms, such as inflammation, endothelial cell disorders and the production of reactive oxygen and nitrogen species, were also observed[41,47]. The histological examination of animal heart tissue demonstrated wavy fibers, which are consistent with myocardial infarction and the presence of microthrombi in the capillary area of the myocardium, whereas the perivascular lesions were rather unrepresentative, supporting the idea of a mechanism of injury originating from the vascular system[41].
The postischemic phase is characterized by liver parenchymal dysfunction and the secretion of proinflammatory cytokines. Excessive TNF-α and IL-6 production and the systemic inflammatory response contribute to distant organ damage. Reactive oxygen species and cytokines generated during the reperfusion phase flow from the hepatic veins directly to the right atrium. Thus, the heart is the first organ receiving blood flow from postischemic hepatic tissue, which makes it more susceptible to damage[52,53]. The reactive oxygen radicals generated at the onset of reperfusion result in both direct cellular damage (necrosis, membrane disruptions) and indirect damage through cellular signaling pathways[54,55]. In a recent study, a histopathological heart examination of animals subjected to hepatic ischemia-reperfusion demonstrated necrosis, hyperemia, hemorrhage, and edema of myocardial cells[52].
Calcineurin is a calcium- and calmodulin-dependent serine/threonine protein phosphatase that plays an important role in T-cell activation, transcription regulation, cell cycle control and apoptosis[56]. In the heart, calcineurin is primarily present in the context of the hypertrophic growth response and pathological cardiac remodeling due to its role in nuclear factor of activated T cells transcription factor activation[57,58]. The inhibition of the calcineurin signaling pathway by tacrolimus attenuates myocardial damage after total hepatic ischemia-reperfusion. Furthermore, the protective role of tacrolimus in stabilizing the mitochondrial membrane potential, avoiding impairment in mitochondrial respiration and oxidative phosphorylation, improving antioxidant capacity, and reducing calcium overload prevent the myocardium from experiencing cell injury and potentially cell death[59,60]. In general, regulation of calcium homeostasis showed effectiveness on protecting hepatocytes from ischemia-reperfusion injury, such as protection during cardiac arrhythmias. A recently discovered HBF001 heparin fragment acts on sodium-calcium exchanger, by altering peptide structure and accelerating the intracellular calcium output[61].
Hepatic ischemia may induce a series of biochemical reactions, including modifications in the interactions between factors controlling programmed cell death and apoptosis. In a recent experimental study, increased levels of the proapoptotic protein Bax and decreased levels of the antiapoptotic protein Bcl-2 were measured. According to the article, hepatic ischemia-reperfusion injury accelerated apoptosis of myocardial cells and damaged the myocardium. Likewise, based on cardiac function observations, the ventricles of animals were enlarged and thickened, and ventricular systolic function was decreased in the control group[62-64].
Occlusion of the hepatic artery and the portal vein may be necessary to avoid excessive bleeding during major hepatectomy and liver transplantation. However, total hepatic vascular exclusion is associated with profound volume shifts due to preload reduction, resulting in a decrease in cardiac output and hemodynamic instability[65,66]. Chen et al[67] showed that decreased left ventricular preload was the primary reason for the reduced cardiac output, stroke volume and ejection fraction during liver ischemia. Along with impaired cardiovascular function, the systemic inflammatory response and activated neutrophil accumulation in the myocardium are simultaneously responsible for remote organ injury induced by hepatic ischemia-reperfusion[56,57].
Myocardial injury appears to be a serious complication of hepatic ischemia-reperfusion syndrome, but the clinical manifestations in humans have not yet been established. Only a small percentage of patients who underwent liver transplantation and presented with mild hepatic ischemia-reperfusion injury (aspartate aminotransferase < 2000 IU/L) developed severe impairment of the left ventricular ejection fraction (< 35%)[68]. Despite being uncommon, post liver transplantation cardiac dysfunction remains a major clinical problem. Although the evidence supporting the idea of a direct association between hepatic ischemia-reperfusion and deterioration of left ventricular systolic function is still inconclusive, it is possible that the systemic inflammatory response and hemodynamic instability can contribute to postoperative cardiomyopathy[69]. Several studies have described an incidence of acute posttransplantation systolic heart failure of 1%-7%, frequently caused by stress-induced cardiomyopathy. However, hepatic ischemia-reperfusion syndrome was not exactly identified as an etiological underlying condition[70,71]. Intraoperative cardiovascular stress negatively affects preexisting cardiac dysfunction. Theoretically, hepatic ischemia-reperfusion syndrome presenting in the surgical postreperfusion phase may be associated with myocardial depression, pulmonary arterial hypertension, a significant reduction in systemic vascular resistance and bradycardia. Reactive oxygen species and multiple inflammatory mediators, such as cytokines and chemokines, are also responsible for the clinical phenotype of postreperfusion syndrome[72-74].
Although the link between hepatic ischemia-reperfusion syndrome and myocardial injury has been made in animal models, the consequences of this effect have yet to be defined. Myocardial damage has been described mostly as histopathological lesions and altered laboratory findings rather than serious clinical manifestations. After all, it must not be forgotten that most experimental and clinical observations are made in relatively healthy individuals and not in those whose heart is already affected by ischemia, cardiomyopathy and systolic/diastolic dysfunction[1,75,76]. Apparently, cardiac impairment following hepatic ischemia-reperfusion syndrome encompasses a large spectrum of subclinical and symptomatic conditions, which are responsible for additional short- and long-term morbidity and low survival[74]. Thus, continuous research should be directed to finding effective therapeutic options to improve the outcome and reduce the postoperative mortality rates.
The therapeutic strategies against hepatic ischemia-reperfusion syndrome mainly include protective intraoperative techniques and an adequate number of pharmacological agents. Prostaglandins are a group of physiologically active lipid compounds called eicosanoids, which consist of oxidized derivatives of 20-carbon polyunsaturated fatty acids, primarily arachidonic acid, formed due to the cyclooxygenase pathway[77-79]. Many studies have shown the liver cytoprotective ability of prostaglandins based on direct or indirect signaling pathways[80]. The effectiveness of prostaglandin analogs has been evaluated in several experimental models along with patients who underwent liver transplantation. Prostaglandin E1 (PGE1) administration has been shown to improve liver microcirculation dysfunction by the expansion of blood vessels and enhancement of perfusion status. PGE1 also downregulates the expression of adhesion molecules and inflammatory mediators, resulting in inhibition of platelet aggregation and leukocyte adherence. Furthermore, suppression of thromboxane A2 in combination with the reduction in protease release and oxygen free radical production leads to attenuation of the inflammatory cascade and minimization of the sinusoidal cell apoptosis rate[81-84]. Prostacyclin (PGI2) is another member of the prostaglandin family with potential vasodilating, antithrombotic and anti-inflammatory effects. Prostacyclin analogs have been established for decades in the treatment of patients with pulmonary arterial hypertension and remain an integral component of the current therapeutic armamentarium[85-87]. Preconditioning with beraprost sodium, a prostacyclin analog, in the experimental hepatic ischemia-reperfusion model led to suppressed production of the inflammatory mediators TNF-α and IL-1β, and attenuation of hepatic cell apoptosis in a dose-dependent manner. Through inhibition of the phosphorylation of P38 and JNK signaling cascades, beraprost sodium could ameliorate the systemic inflammatory response, apoptosis and autophagy processes of hepatic ischemia-reperfusion[21]. Although several studies have shown beneficial effects of prostaglandin therapy in the prevention of liver damage following transplantation, the clinical utility of these agents is rather limited due to their unstable structure, serious adverse reactions and very short half-lives[77,82,88,89].
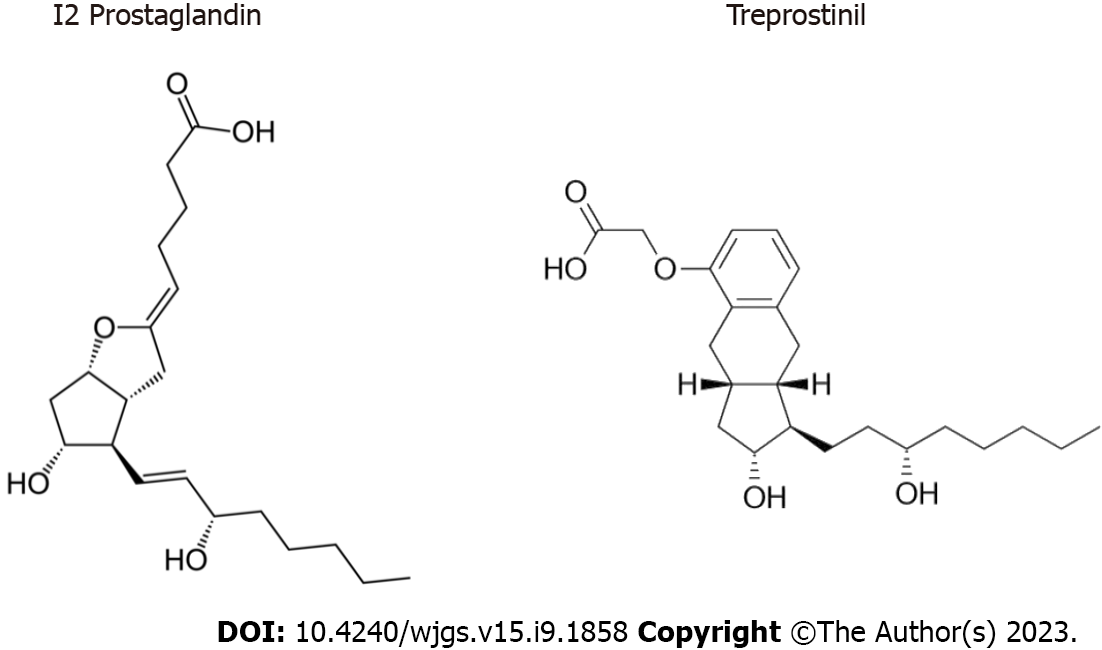
Treprostinil is a relatively new prostaglandin I2 (PGI2, prostacyclin) analog with a stable structure (as shown in Figure 2), longer half-life and improved potency that has been approved by the Food and Drug Administration (FDA) in the United States since 2002 for the treatment of patients with pulmonary arterial hypertension[86]. Treprostinil demonstrated stability for 48 h at 40 °C in different solutions and multiple beneficial effects, promoting its administration in long-term therapy[90-93]. Its binding profile and corresponding biochemical cellular response on human prostanoid receptors have been sufficiently analyzed. Treprostinil has high affinity for the DP1, EP2 and IP receptors; low affinity for EP1 and EP4 receptors; and even lower affinity for EP3, FP and TP receptors[94]. The mechanisms of action of treprostinil are summarized in Table 2. In general, the PGI2 signaling pathways are much more complex than anticipated and remain incompletely elucidated. Peroxisome proliferator-activated receptors constitute an important signaling pathway that partially explains the vasodilating effect of prostacyclin, along with its cytoprotective properties[95,96]. The effects of treprostinil on angiogenesis have also been reported, including the vascular endothelial growth factor (VEGF)/NADPH oxidase 4 signaling pathway. In vitro treprostinil administration enhanced VEGF-A synthesis by mesenchymal stem cells, resulting in activation of vessel-forming ability[97].
| Effect | Mechanism of action | Cellular response |
| Vessel tone | cAMP increased. Endothelin 1 decreased. Potassium decreased | Vasodilation. Improvement of microcirculation dysfunction |
| Antiproliferative | PPARs increased. cAMP increased. VEGF-A increased | Angiogenesis. Regulation of vascular homeostasis |
| Antithrombotic | Thromboxane A2 decreased. PDGF decreased | Inhibition of platelets aggregation. Platelets adherence decreased |
| Anti-inflammatory | P38 and JNK cascades decreased. IL-1, IL-6, TNF-α decreased. IL-10 increased. Reactive oxygen species decreased. TLR 9 decreased | Attenuation of inflammatory cascade. Apoptosis rate increased |
| Energy balance | Pgc-1α mRNA expression decreased. Cytochrome c decreased. Caspase 3 activation decreased | ATP production increased. Mitochondrial biogenesis increased |
Experimental orthotopic liver transplantation in rats with subcutaneous treprostinil administration at a dose of 100 ng/kg/min showed very encouraging results[98]. Specifically, treprostinil increased liver blood flow during the reperfusion phase while supporting the balance within the vasculature by increasing intracellular cyclic adenosine monophosphate (cAMP) levels. Furthermore, inhibition of platelet aggregation and proinflammatory cytokine production in the early posttransplantation period protected the liver graft against hepatic ischemia-reperfusion injury. Additionally, Hou et al[99] demonstrated that treprostinil improves renal and hepatic function, diminishes hepatic oxidative stress and lipid peroxidation and reduces hepatic TLR9, which is located in endosomes and triggers the inflammatory response by recognizing PAMPs and DAMPs[100]. Another recent study suggested that the presence of Gs-coupled prostanoid receptors in liver sinusoidal endothelial cells was responsible for the beneficial effect of prostaglandins. In fact, treprostinil binds and activates EP2, EP4, and IP receptors, resulting in attenuation of ischemia-induced hepatic cell injury[101].
Mitochondrial dysfunction during hepatic ischemia-reperfusion leads to increased DNA fragmentation and induction of programmed cell apoptosis. To maintain mitochondrial homeostasis and mediate acute cell injury, a complex fundamental process, named mitochondrial biogenesis, typically occurs in response to postischemic cellular stress. Induction of mitochondrial biogenesis is mediated by upregulation of the transcription factor peroxisome proliferator-activated receptor gamma coactivator 1-alpha (PGC-1α), which is considered to be the master regulator for the process and has been found to be significantly decreased in ischemia-reperfusion injury[99,102-104]. Treprostinil upregulates Pgc-1α mRNA expression, thus securing mitochondrial biogenesis and improving mitochondrial dynamics. Additionally, treprostinil inhibits hepatic apoptosis by suppressing the release of mitochondrial cytochrome c and caspase-3 activation. In general, treprostinil restores ATP production, which ameliorates hepatic mitochondrial injury and preserves cellular energy balance[99,105,106].
Several studies have shown that hepatic ischemia-reperfusion injury may cause a reduction in hepatic cytochrome P450 (CYP) levels and/or changes in enzyme activity amplitude. CYP has a broad range of functions, including drug metabolism and clearance and detoxification of pharmaceutical substances. The excessive cytokine release and systemic inflammatory response during ischemia-reperfusion injury have been associated with reduced microsomal drug metabolism, which can cause dose-dependent drug toxicity[107-109]. Treprostinil administration improved CYP mRNA expression in liver grafts after clinically relevant rat liver transplantation. In addition, treprostinil restored CYP protein expression and improved its activity in liver grafts[110]. The results showed that extended hepatic ischemia-reperfusion injury impaired CYP450 protein expression for at least 48 h post-transplantation, while treprostinil administration improved the protein expression of the three major CYP450 enzymes (CYP3A2, CYP2C11, and CYP2E1) in the liver graft and promoted CYP450-mediated drug metabolism[110].
Isolated rat liver perfusion is a widely performed ex vivo experimental model and represents a suitable tool for studying various pathological conditions, such as hepatic ischemia-reperfusion injury[111]. A recent study performed on isolated rat livers demonstrated the effect of postischemic hepatic injury on the expression of basolateral (uptake) and apical (efflux) hepatic drug transporters, which was significantly altered[112]. Importantly, treprostinil administration at a dose of 20 ng/mL during preservation and/or reperfusion reduced the ischemia-reperfusion-mediated effects on the expression of the Slc10a1/Ntcp and Slc22a1/Oct1 drug uptake transporters, similar to the expression of the apical efflux drug transporter P-gp (Mdr1a, Abcb1a). Although these findings illustrated improved liver function due to treprostinil supplementation, deeper knowledge is needed to determine the effect of the particular synthetic prostacyclin on the expression of drug-metabolizing enzymes and the regulation of drug transporters[113].
Liver graft injury post-transplantation frequently presents with elevated bilirubin and amino-transaminase serum levels during the first 24 h following transplantation. Many studies support the hypothesis of hepatic ischemia-reperfusion syndrome as the leading cause of initial poor graft dysfunction and primary graft nonfunction[114-117]. However, no pharmacological options are currently approved for the prevention of hepatic ischemia-reperfusion injury following transplantation. A prospective, pilot, single-center, open-label, nonrandomized, dose-escalation phase I/II study in liver transplant patients investigated the efficacy of intravenous treprostinil administration in the prevention of hepatic ischemia-reperfusion with some encouraging results[118]. A small group of patients who underwent liver transplantation and received perioperative intravenous treprostinil at a dose of 5 ng/kg/min followed by postoperative contentious infusion at a dose of 2.5-5 ng/kg/min for approximately 5 d showed improved liver function and 100% graft and recipient survival at six months[118]. Preliminary observations indicated a rapid reduction in transaminase plasma levels, improvement in hepatobiliary excretory function and prevention of the occurrence of acute kidney failure. Furthermore, stable hemodynamic parameters in the patients with treprostinil administration during the study period were achieved, since the mean pulmonary arterial pressure, systemic blood pressure, and cardiac index values remained within the normal range.
The initial phase of hepatic injury is characterized by ATP depletion, mitochondrial dysfunction and reactive oxygen species accumulation, followed by a systemic sterile inflammatory response. In general, oxidative and inflammatory pathways have been shown to play an important role in remote organ functional changes in a state of hepatic ischemia-reperfusion injury. Although myocardial impairment is documented mostly as a subclinical event, the general clinical status of remote organ damage in the postreperfusion phase can directly affect overall survival rates. Additionally, while a hypothesis of myocardial injury in the setting of hepatic ischemia-reperfusion has already been reported, the consequences of the particular issue remain unclear[116-118].
Over the last few years, treprostinil has become one of the key therapeutic options for the treatment of patients with pulmonary arterial hypertension[119]. Along with its beneficial influence on pulmonary vascular smooth muscle proliferation, vasoconstriction and pulmonary vascular remodeling, treprostinil also shows a direct favorable effect on cardiac function[120,121]. Experimental treprostinil administration increased stroke volume and cardiac output, leading to a stable hemodynamic state and improved cardiovascular endurance[121-123]. In addition, a broad reduction in reactive oxygen species accumulation and lipid peroxidation and a decrease in cytokine and chemokine mRNA levels during ischemia-reperfusion may protect the myocardium from postreperfusion injury. However, there are several reports of beneficial effects of prostacyclin analogs on the attenuation of myocardial ischemia-reperfusion injury via vasodilation, inhibition of platelet accumulation and anti-inflammation[124,125]. Finally, the acceleration of mitochondrial recovery due to reduced mitochondrial-mediated cell apoptosis supports the hypothesis of treprostinil-mediated organ protection against ischemia-reperfusion injury[104]. Although currently available data are not sufficient, there are several indications of the beneficial effect of treprostinil on remote organ damage in the course of hepatic ischemia-reperfusion syndrome. Recent studies with subcutaneous treprostinil administration in experimental hepatic ischemia-reperfusion models have shown very encouraging results. Furthermore, patients with pulmonary arterial hypertension treated with treprostinil demonstrated an improved hemodynamic state and stable cardiac parameters[123].
Hepatic ischemia-reperfusion syndrome is a major complication of liver surgery, including partial liver resection and liver transplantation, liver trauma, resuscitation and other clinical entities. The pathophysiological mechanisms of hepatic ischemia-reperfusion are not responsible for liver damage alone but also occur as a complex systemic process with a direct impact on the function of multiple tissues and organs. Moreover, in some cases, postreperfusion systemic injury can lead to systemic inflammatory response syndrome and/or multiorgan dysfunction syndrome, both of which have a high incidence of mortality and morbidity. Thus, therapeutic strategies, including advanced surgical techniques and pharmacological inhibitors, should be studied intensively to improve the outcome of these patients. Treprostinil is a relatively new, FDA-approved stable prostacyclin analog with potent anti-inflammatory, antifibrotic, vasodilating, antiremodeling and antiapoptotic activities. According to current knowledge, there is a positive correlation between treprostinil supplementation and the attenuation of liver ischemia-reperfusion injury. Such information may be also useful in determining the favorable effect of treprostinil on remote organ damage. Although treprostinil administration holds great promise for attenuating myocardial injury in the course of hepatic ischemia-reperfusion injury, further research is warranted.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shehta A, Egypt; Wu ZJ, China S-Editor: Wang JJ L-Editor: A P-Editor: Wu RR
| 1. | Nastos C, Kalimeris K, Papoutsidakis N, Tasoulis MK, Lykoudis PM, Theodoraki K, Nastou D, Smyrniotis V, Arkadopoulos N. Global consequences of liver ischemia/reperfusion injury. Oxid Med Cell Longev. 2014;2014:906965. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 225] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 2. | Zhai Y, Petrowsky H, Hong JC, Busuttil RW, Kupiec-Weglinski JW. Ischaemia-reperfusion injury in liver transplantation--from bench to bedside. Nat Rev Gastroenterol Hepatol. 2013;10:79-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 666] [Article Influence: 55.5] [Reference Citation Analysis (0)] |
| 3. | Konishi T, Lentsch AB. Hepatic Ischemia/Reperfusion: Mechanisms of Tissue Injury, Repair, and Regeneration. Gene Expr. 2017;17:277-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 176] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 4. | Huang DQ, Terrault NA, Tacke F, Gluud LL, Arrese M, Bugianesi E, Loomba R. Global epidemiology of cirrhosis - aetiology, trends and predictions. Nat Rev Gastroenterol Hepatol. 2023;20:388-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 368] [Article Influence: 184.0] [Reference Citation Analysis (0)] |
| 5. | Panconesi R, Carvalho MF, Muiesan P, Dutkowski P, Schlegel A. Liver perfusion strategies: what is best and do ischemia times still matter? Curr Opin Organ Transplant. 2022;27:285-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Sookoian S, Pirola CJ. Liver enzymes, metabolomics and genome-wide association studies: from systems biology to the personalized medicine. World J Gastroenterol. 2015;21:711-725. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 150] [Cited by in RCA: 209] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 7. | Lightsey JM, Rockey DC. Current concepts in ischemic hepatitis. Curr Opin Gastroenterol. 2017;33:158-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (1)] |
| 8. | Cannistrà M, Ruggiero M, Zullo A, Gallelli G, Serafini S, Maria M, Naso A, Grande R, Serra R, Nardo B. Hepatic ischemia reperfusion injury: A systematic review of literature and the role of current drugs and biomarkers. Int J Surg. 2016;33 Suppl 1:S57-S70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 257] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 9. | Montalvo-Jave EE, Escalante-Tattersfield T, Ortega-Salgado JA, Piña E, Geller DA. Factors in the pathophysiology of the liver ischemia-reperfusion injury. J Surg Res. 2008;147:153-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 291] [Cited by in RCA: 288] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 10. | Jiménez-Castro MB, Cornide-Petronio ME, Gracia-Sancho J, Peralta C. Inflammasome-Mediated Inflammation in Liver Ischemia-Reperfusion Injury. Cells. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 180] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 11. | Selzner M, Selzner N, Jochum W, Graf R, Clavien PA. Increased ischemic injury in old mouse liver: an ATP-dependent mechanism. Liver Transpl. 2007;13:382-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 12. | Guan LY, Fu PY, Li PD, Li ZN, Liu HY, Xin MG, Li W. Mechanisms of hepatic ischemia-reperfusion injury and protective effects of nitric oxide. World J Gastrointest Surg. 2014;6:122-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 121] [Cited by in RCA: 136] [Article Influence: 12.4] [Reference Citation Analysis (2)] |
| 13. | Hirao H, Nakamura K, Kupiec-Weglinski JW. Liver ischaemia-reperfusion injury: a new understanding of the role of innate immunity. Nat Rev Gastroenterol Hepatol. 2022;19:239-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 206] [Article Influence: 68.7] [Reference Citation Analysis (0)] |
| 14. | Tacke F. Targeting hepatic macrophages to treat liver diseases. J Hepatol. 2017;66:1300-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 504] [Cited by in RCA: 732] [Article Influence: 91.5] [Reference Citation Analysis (0)] |
| 15. | Hanschen M, Zahler S, Krombach F, Khandoga A. Reciprocal activation between CD4+ T cells and Kupffer cells during hepatic ischemia-reperfusion. Transplantation. 2008;86:710-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Ye L, He S, Mao X, Zhang Y, Cai Y, Li S. Effect of Hepatic Macrophage Polarization and Apoptosis on Liver Ischemia and Reperfusion Injury During Liver Transplantation. Front Immunol. 2020;11:1193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 115] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 17. | van de Poll MC, Dejong CH, Fischer MA, Bast A, Koek GH. Decreased hepatosplanchnic antioxidant uptake during hepatic ischaemia/reperfusion in patients undergoing liver resection. Clin Sci (Lond). 2008;114:553-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Li J, Ke W, Zhou Q, Wu Y, Luo H, Zhou H, Yang B, Guo Y, Zheng Q, Zhang Y. Tumour necrosis factor-α promotes liver ischaemia-reperfusion injury through the PGC-1α/Mfn2 pathway. J Cell Mol Med. 2014;18:1863-1873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Rosser BG, Gores GJ. Liver cell necrosis: cellular mechanisms and clinical implications. Gastroenterology. 1995;108:252-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 263] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 20. | Kyriakis JM, Avruch J. Mammalian MAPK signal transduction pathways activated by stress and inflammation: a 10-year update. Physiol Rev. 2012;92:689-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 873] [Cited by in RCA: 1077] [Article Influence: 82.8] [Reference Citation Analysis (0)] |
| 21. | Deng J, Feng J, Liu T, Lu X, Wang W, Liu N, Lv Y, Liu Q, Guo C, Zhou Y. Beraprost sodium preconditioning prevents inflammation, apoptosis, and autophagy during hepatic ischemia-reperfusion injury in mice via the P38 and JNK pathways. Drug Des Devel Ther. 2018;12:4067-4082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Yang H, Huang Z, Luo Y, Lei D, Yan P, Shen A, Liu W, Li D, Wu Z. TRIM37 exacerbates hepatic ischemia/reperfusion injury by facilitating IKKγ translocation. Mol Med. 2023;29:62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 23. | Pretzsch E, Nieß H, Khaled NB, Bösch F, Guba M, Werner J, Angele M, Chaudry IH. Molecular Mechanisms of Ischaemia-Reperfusion Injury and Regeneration in the Liver-Shock and Surgery-Associated Changes. Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 24. | Huang Z, Mou T, Luo Y, Pu X, Pu J, Wan L, Gong J, Yang H, Liu Y, Li Z, Shen A, Wu Z. Inhibition of miR-450b-5p ameliorates hepatic ischemia/reperfusion injury via targeting CRYAB. Cell Death Dis. 2020;11:455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 25. | Huang Z, Zheng D, Pu J, Dai J, Zhang Y, Zhang W, Wu Z. MicroRNA-125b protects liver from ischemia/reperfusion injury via inhibiting TRAF6 and NF-κB pathway. Biosci Biotechnol Biochem. 2019;83:829-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 26. | Zhu SF, Yuan W, Du YL, Wang BL. Research progress of lncRNA and miRNA in hepatic ischemia-reperfusion injury. Hepatobiliary Pancreat Dis Int. 2023;22:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Eltzschig HK, Eckle T. Ischemia and reperfusion--from mechanism to translation. Nat Med. 2011;17:1391-1401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1886] [Cited by in RCA: 2510] [Article Influence: 179.3] [Reference Citation Analysis (0)] |
| 28. | Jaeschke H, Lemasters JJ. Apoptosis versus oncotic necrosis in hepatic ischemia/reperfusion injury. Gastroenterology. 2003;125:1246-1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 441] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 29. | Schwabe RF, Luedde T. Apoptosis and necroptosis in the liver: a matter of life and death. Nat Rev Gastroenterol Hepatol. 2018;15:738-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 435] [Article Influence: 62.1] [Reference Citation Analysis (0)] |
| 30. | Papoutsidakis N, Arkadopoulos N, Smyrniotis V, Tzanatos H, Kalimeris K, Nastos K, Defterevos G, Pafiti A, Kostopanagiotou G. Early myocardial injury is an integral component of experimental acute liver failure - a study in two porcine models. Arch Med Sci. 2011;7:217-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 31. | Lee HT, Park SW, Kim M, D'Agati VD. Acute kidney injury after hepatic ischemia and reperfusion injury in mice. Lab Invest. 2009;89:196-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 95] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 32. | Oguz A, Kapan M, Kaplan I, Alabalik U, Ulger BV, Uslukaya O, Turkoglu A, Polat Y. The effects of sulforaphane on the liver and remote organ damage in hepatic ischemia-reperfusion model formed with pringle maneuver in rats. Int J Surg. 2015;18:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Kan C, Ungelenk L, Lupp A, Dirsch O, Dahmen U. Ischemia-Reperfusion Injury in Aged Livers-The Energy Metabolism, Inflammatory Response, and Autophagy. Transplantation. 2018;102:368-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 34. | Ma Z, Xin Z, Di W, Yan X, Li X, Reiter RJ, Yang Y. Melatonin and mitochondrial function during ischemia/reperfusion injury. Cell Mol Life Sci. 2017;74:3989-3998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 35. | Wu XY, Chen YJ, Liu CA, Gong JH, Xu XS. STING Induces Liver Ischemia-Reperfusion Injury by Promoting Calcium-Dependent Caspase 1-GSDMD Processing in Macrophages. Oxid Med Cell Longev. 2022;2022:8123157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 36. | Zhang H, Goswami J, Varley P, van der Windt DJ, Ren J, Loughran P, Yazdani H, Neal MD, Simmons RL, Zhang J, Tsung A, Huang H. Hepatic Surgical Stress Promotes Systemic Immunothrombosis That Results in Distant Organ Injury. Front Immunol. 2020;11:987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 37. | Xin Y, Zhang Y, Deng S, Hu X. Vagus Nerve Stimulation Attenuates Acute Skeletal Muscle Injury Induced by Hepatic Ischemia/Reperfusion Injury in Rats. Front Pharmacol. 2021;12:756997. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 38. | Zhu L, Zhou H, Xu F, Yang H, Li P, Sheng Y, Liu P, Kong W, Liu X, Yang L, Liu L. Hepatic Ischemia-Reperfusion Impairs Blood-Brain Barrier Partly Due to Release of Arginase From Injured Liver. Front Pharmacol. 2021;12:724471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 39. | Rampes S, Ma D. Hepatic ischemia-reperfusion injury in liver transplant setting: mechanisms and protective strategies. J Biomed Res. 2019;33:221-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 40. | Rovegno M, Vera M, Ruiz A, Benítez C. Current concepts in acute liver failure. Ann Hepatol. 2019;18:543-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 41. | Uhlig M, Hein M, Habigt MA, Tolba RH, Braunschweig T, Helmedag MJ, Klinge U, Koch A, Trautwein C, Mechelinck M. Acute myocardial injury secondary to severe acute liver failure: A retrospective analysis supported by animal data. PLoS One. 2021;16:e0256790. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 42. | Park KC, Gaze DC, Collinson PO, Marber MS. Cardiac troponins: from myocardial infarction to chronic disease. Cardiovasc Res. 2017;113:1708-1718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 317] [Cited by in RCA: 333] [Article Influence: 41.6] [Reference Citation Analysis (0)] |
| 43. | Hamm CW, Giannitsis E, Katus HA. Cardiac troponin elevations in patients without acute coronary syndrome. Circulation. 2002;106:2871-2872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 137] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 44. | Ahmed AN, Blonde K, Hackam D, Iansavichene A, Mrkobrada M. Prognostic significance of elevated troponin in non-cardiac hospitalized patients: a systematic review and meta-analysis. Ann Med. 2014;46:653-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 45. | Aydin S, Ugur K, Aydin S, Sahin İ, Yardim M. Biomarkers in acute myocardial infarction: current perspectives. Vasc Health Risk Manag. 2019;15:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 321] [Cited by in RCA: 266] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 46. | Kim S, Um TH, Cho CR, Jeon JS. False-positive elevation of creatine kinase MB mass concentrations caused by macromolecules in a patient who underwent nephrectomy for renal cell carcinoma. Ann Lab Med. 2014;34:405-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Engelmann C, Clària J, Szabo G, Bosch J, Bernardi M. Pathophysiology of decompensated cirrhosis: Portal hypertension, circulatory dysfunction, inflammation, metabolism and mitochondrial dysfunction. J Hepatol. 2021;75 Suppl 1:S49-S66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 218] [Article Influence: 54.5] [Reference Citation Analysis (1)] |
| 48. | Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev. 2014;94:909-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2139] [Cited by in RCA: 3814] [Article Influence: 346.7] [Reference Citation Analysis (0)] |
| 49. | Idzko M, Ferrari D, Eltzschig HK. Nucleotide signalling during inflammation. Nature. 2014;509:310-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 598] [Cited by in RCA: 737] [Article Influence: 67.0] [Reference Citation Analysis (0)] |
| 50. | Lee J, Lee S, Zhang H, Hill MA, Zhang C, Park Y. Interaction of IL-6 and TNF-α contributes to endothelial dysfunction in type 2 diabetic mouse hearts. PLoS One. 2017;12:e0187189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 91] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 51. | Brito-Azevedo A, Perez RM, Maranhão PA, Coelho HS, Fernandes ESM, Castiglione RC, de Souza MD, Villela-Nogueira CA, Bouskela E. Organ dysfunction in cirrhosis: a mechanism involving the microcirculation. Eur J Gastroenterol Hepatol. 2019;31:618-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 52. | Zabala V, Boylan JM, Thevenot P, Frank A, Senthoor D, Iyengar V, Kim H, Cohen A, Gruppuso PA, Sanders JA. Transcriptional changes during hepatic ischemia-reperfusion in the rat. PLoS One. 2019;14:e0227038. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 53. | An W, Kang JS. Effect of Metformin on Myocardial Injury Induced by Hepatic Ischemia-Reperfusion in Rats. Front Pharmacol. 2022;13:822743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 54. | Espinosa-Diez C, Miguel V, Mennerich D, Kietzmann T, Sánchez-Pérez P, Cadenas S, Lamas S. Antioxidant responses and cellular adjustments to oxidative stress. Redox Biol. 2015;6:183-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 639] [Cited by in RCA: 785] [Article Influence: 78.5] [Reference Citation Analysis (0)] |
| 55. | Granger DN, Kvietys PR. Reperfusion injury and reactive oxygen species: The evolution of a concept. Redox Biol. 2015;6:524-551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 733] [Cited by in RCA: 1047] [Article Influence: 104.7] [Reference Citation Analysis (0)] |
| 56. | Herzog CJ, Miot S, Mansuy IM, Giros B, Tzavara ET. Chronic valproate normalizes behavior in mice overexpressing calcineurin. Eur J Pharmacol. 2008;580:153-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 57. | Parra V, Rothermel BA. Calcineurin signaling in the heart: The importance of time and place. J Mol Cell Cardiol. 2017;103:121-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 58. | Chaklader M, Rothermel BA. Calcineurin in the heart: New horizons for an old friend. Cell Signal. 2021;87:110134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 59. | Chen Y, Xie X. Tacrolimus attenuates myocardium damage to the total hepatic ischemia-reperfusion via regulation of the mitochondrial function. J Surg Res. 2012;172:e47-e54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 60. | Diotte NM, Xiong Y, Gao J, Chua BH, Ho YS. Attenuation of doxorubicin-induced cardiac injury by mitochondrial glutaredoxin 2. Biochim Biophys Acta. 2009;1793:427-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 61. | Vasques ER, Figueira ER, Rocha-Filho JA, Lanchotte C, Ximenes JL, Nader HB, Tersariol IL, Lima MA, Rodrigues T, Cunha JE, Chaib E, D'Albuquerque LA, Galvão FH. A new heparin fragment decreases liver ischemia-reperfusion injury. Hepatobiliary Pancreat Dis Int. 2022;21:190-192. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 62. | Megyesi J, Tarcsafalvi A, Seng N, Hodeify R, Price PM. Cdk2 phosphorylation of Bcl-xL after stress converts it to a pro-apoptotic protein mimicking Bax/Bak. Cell Death Discov. 2016;2:15066-15066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 63. | Ashkenazi A, Fairbrother WJ, Leverson JD, Souers AJ. From basic apoptosis discoveries to advanced selective BCL-2 family inhibitors. Nat Rev Drug Discov. 2017;16:273-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 476] [Cited by in RCA: 650] [Article Influence: 81.3] [Reference Citation Analysis (0)] |
| 64. | Lv J, Zou X, Yu C, Ou W, Sun C. Effects of propofol on cardiac function and miR-494 expression in rats with hepatic ischemia/reperfusion injury. J Int Med Res. 2021;49:300060521990988. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 65. | Søreide JA, Deshpande R. Post hepatectomy liver failure (PHLF) - Recent advances in prevention and clinical management. Eur J Surg Oncol. 2021;47:216-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 140] [Article Influence: 28.0] [Reference Citation Analysis (1)] |
| 66. | Chen Y, Liu Z, Xie X. Hydrogen sulphide attenuates renal and cardiac injury after total hepatic ischemia and reperfusion. J Surg Res. 2010;164:e305-e313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 67. | Chen TH, Chen KH, Wang JJ. Preischemic treatment with melatonin attenuates liver reperfusion-induced impairment of cardiac function. Transplant Proc. 2012;44:970-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 68. | Rokop ZP, Frick K, Zenisek J, Kroepfl E, Mihaylov P, Patidar KR, Nephew L, Mangus RS, Kubal C. Hepatic Ischemia/Reperfusion Injury After Liver Transplantation Is Not Associated with Early Impairment of Left Ventricular Ejection Fraction. Ann Transplant. 2022;27:e938105. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 69. | Manning MW, Kumar PA, Maheshwari K, Arora H. Post-Reperfusion Syndrome in Liver Transplantation-An Overview. J Cardiothorac Vasc Anesth. 2020;34:501-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 70. | Sonny A, Govindarajan SR, Jaber WA, Cywinski JB. Systolic heart failure after liver transplantation: Incidence, predictors, and outcome. Clin Transplant. 2018;32:e13199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 71. | Sakr AE, Fraser GE, Doctorian TP, Kim HB, Narasimha D, Abudayyeh I, Hilliard AD, Shih W, de Vera ME, Baron PW, Volk ML, Stoletniy LN. Predictors of Systolic Heart Failure and Mortality Following Orthotopic Liver Transplantation: a Single-Center Cohort. Transplant Proc. 2019;51:1950-1955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 72. | Paugam-Burtz C, Kavafyan J, Merckx P, Dahmani S, Sommacale D, Ramsay M, Belghiti J, Mantz J. Postreperfusion syndrome during liver transplantation for cirrhosis: outcome and predictors. Liver Transpl. 2009;15:522-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 177] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 73. | Girn HR, Ahilathirunayagam S, Mavor AI, Homer-Vanniasinkam S. Reperfusion syndrome: cellular mechanisms of microvascular dysfunction and potential therapeutic strategies. Vasc Endovascular Surg. 2007;41:277-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 74. | Zaky A, Bendjelid K. Appraising cardiac dysfunction in liver transplantation: an ongoing challenge. Liver Int. 2015;35:12-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 75. | Jaber S, Paugam-Burtz C. Acute liver failure and elevated troponin-I: controversial results and significance? Crit Care. 2013;17:102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 76. | Audimooolam VK, McPhail MJ, Sherwood R, Willars C, Bernal W, Wendon JA, Auzinger G. Elevated troponin I and its prognostic significance in acute liver failure. Crit Care. 2012;16:R228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 77. | Hossain MA, Wakabayashi H, Izuishi K, Okano K, Yachida S, Maeta H. The role of prostaglandins in liver ischemia-reperfusion injury. Curr Pharm Des. 2006;12:2935-2951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 78. | Calder PC. Eicosanoids. Essays Biochem. 2020;64:423-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 176] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 79. | Liu H, Man K. New Insights in Mechanisms and Therapeutics for Short- and Long-Term Impacts of Hepatic Ischemia Reperfusion Injury Post Liver Transplantation. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 80. | Yamanaka K, Houben P, Bruns H, Schultze D, Hatano E, Schemmer P. A systematic review of pharmacological treatment options used to reduce ischemia reperfusion injury in rat liver transplantation. PLoS One. 2014;10:e0122214. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 81. | Liu Y, Ren H, Wang J, Yang F, Li J, Zhou Y, Yuan X, Zhu W, Shi X. Prostaglandin E(2) secreted by mesenchymal stem cells protects against acute liver failure via enhancing hepatocyte proliferation. FASEB J. 2019;33:2514-2525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 82. | Hafez T, Moussa M, Nesim I, Baligh N, Davidson B, Abdul-Hadi A. The effect of intraportal prostaglandin E1 on adhesion molecule expression, inflammatory modulator function, and histology in canine hepatic ischemia/reperfusion injury. J Surg Res. 2007;138:88-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 83. | Maida K, Akamatsu Y, Hara Y, Tokodai K, Miyagi S, Kashiwadate T, Miyazawa K, Kawagishi N, Ohuchi N. Short Oxygenated Warm Perfusion With Prostaglandin E1 Administration Before Cold Preservation as a Novel Resuscitation Method for Liver Grafts From Donors After Cardiac Death in a Rat In Vivo Model. Transplantation. 2016;100:1052-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 84. | Hanazaki K, Kuroda T, Kajikawa S, Amano J. Prostaglandin E1 reduces thromboxane A2 in hepatic ischemia-reperfusion. Hepatogastroenterology. 2000;47:807-811. [PubMed] |
| 85. | Misawa H, Ohashi W, Tomita K, Hattori K, Shimada Y, Hattori Y. Prostacyclin mimetics afford protection against lipopolysaccharide/d-galactosamine-induced acute liver injury in mice. Toxicol Appl Pharmacol. 2017;334:55-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 86. | Stubbe B, Opitz CF, Halank M, Habedank D, Ewert R. Intravenous prostacyclin-analogue therapy in pulmonary arterial hypertension - A review of the past, present and future. Respir Med. 2021;179:106336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 87. | Hoeper MM, McLaughlin VV, Dalaan AM, Satoh T, Galiè N. Treatment of pulmonary hypertension. Lancet Respir Med. 2016;4:323-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 88. | Chen HM, Chen MF, Shyr MH. Prostacyclin analogue (OP-2507) attenuates hepatic microcirculatory derangement, energy depletion, and lipid peroxidation in a rat model of reperfusion injury. J Surg Res. 1998;80:333-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 89. | Cavalcanti AB, De Vasconcelos CP, Perroni de Oliveira M, Rother ET, Ferraz L Jr. Prostaglandins for adult liver transplanted patients. Cochrane Database Syst Rev. 2011;CD006006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 90. | Phares KR, Weiser WE, Miller SP, Myers MA, Wade M. Stability and preservative effectiveness of treprostinil sodium after dilution in common intravenous diluents. Am J Health Syst Pharm. 2003;60:916-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 91. | Kolb M, Orfanos SE, Lambers C, Flaherty K, Masters A, Lancaster L, Silverstein A, Nathan SD. The Antifibrotic Effects of Inhaled Treprostinil: An Emerging Option for ILD. Adv Ther. 2022;39:3881-3895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 92. | Leifer FG, Konicek DM, Chen KJ, Plaunt AJ, Salvail D, Laurent CE, Corboz MR, Li Z, Chapman RW, Perkins WR, S Malinin V. Inhaled Treprostinil-Prodrug Lipid Nanoparticle Formulations Provide Long-Acting Pulmonary Vasodilation. Drug Res (Stuttg). 2018;68:605-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 93. | Lambers C, Kornauth C, Oberndorfer F, Boehm PM, Tamm M, Klepetko W, Roth M. Mechanism of anti-remodelling action of treprostinil in human pulmonary arterial smooth muscle cells. PLoS One. 2018;13:e0205195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 94. | Whittle BJ, Silverstein AM, Mottola DM, Clapp LH. Binding and activity of the prostacyclin receptor (IP) agonists, treprostinil and iloprost, at human prostanoid receptors: treprostinil is a potent DP1 and EP2 agonist. Biochem Pharmacol. 2012;84:68-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 95. | Pluchart H, Khouri C, Blaise S, Roustit M, Cracowski JL. Targeting the Prostacyclin Pathway: Beyond Pulmonary Arterial Hypertension. Trends Pharmacol Sci. 2017;38:512-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 96. | Falcetti E, Flavell DM, Staels B, Tinker A, Haworth SG, Clapp LH. IP receptor-dependent activation of PPARgamma by stable prostacyclin analogues. Biochem Biophys Res Commun. 2007;360:821-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 97. | Smadja DM, Levy M, Huang L, Rossi E, Blandinières A, Israel-Biet D, Gaussem P, Bischoff J. Treprostinil indirectly regulates endothelial colony forming cell angiogenic properties by increasing VEGF-A produced by mesenchymal stem cells. Thromb Haemost. 2015;114:735-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 98. | Ghonem N, Yoshida J, Stolz DB, Humar A, Starzl TE, Murase N, Venkataramanan R. Treprostinil, a prostacyclin analog, ameliorates ischemia-reperfusion injury in rat orthotopic liver transplantation. Am J Transplant. 2011;11:2508-2516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 99. | Hou J, Tolbert E, Birkenbach M, Ghonem NS. Treprostinil alleviates hepatic mitochondrial injury during rat renal ischemia-reperfusion injury. Biomed Pharmacother. 2021;143:112172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 100. | Anders HJ. Toll-like receptors and danger signaling in kidney injury. J Am Soc Nephrol. 2010;21:1270-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 101. | Themanns M, Koban F, Bergmayr C, Chrzan A, Strohmaier W, Haybaeck J, Freissmuth M, Zebedin-Brandl E. Treprostinil reduces endothelial damage in murine sinusoidal obstruction syndrome. J Mol Med (Berl). 2019;97:201-213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 102. | Hasnat M, Yuan Z, Ullah A, Naveed M, Raza F, Baig MMFA, Khan A, Xu D, Su Y, Sun L, Zhang L, Jiang Z. Mitochondria-dependent apoptosis in triptolide-induced hepatotoxicity is associated with the Drp1 activation. Toxicol Mech Methods. 2020;30:124-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 103. | Ramachandran A, Umbaugh DS, Jaeschke H. Mitochondrial Dynamics in Drug-Induced Liver Injury. Livers. 2021;1:102-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 104. | Ding M, Tolbert E, Birkenbach M, Gohh R, Akhlaghi F, Ghonem NS. Treprostinil reduces mitochondrial injury during rat renal ischemia-reperfusion injury. Biomed Pharmacother. 2021;141:111912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 105. | Ow YP, Green DR, Hao Z, Mak TW. Cytochrome c: functions beyond respiration. Nat Rev Mol Cell Biol. 2008;9:532-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 648] [Cited by in RCA: 812] [Article Influence: 47.8] [Reference Citation Analysis (0)] |
| 106. | Asadi M, Taghizadeh S, Kaviani E, Vakili O, Taheri-Anganeh M, Tahamtan M, Savardashtaki A. Caspase-3: Structure, function, and biotechnological aspects. Biotechnol Appl Biochem. 2022;69:1633-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 257] [Article Influence: 64.3] [Reference Citation Analysis (0)] |
| 107. | Ogaki S, Taguchi K, Maeda H, Watanabe H, Ishima Y, Otagiri M, Maruyama T. Kupffer cell inactivation by carbon monoxide bound to red blood cells preserves hepatic cytochrome P450 via anti-oxidant and anti-inflammatory effects exerted through the HMGB1/TLR-4 pathway during resuscitation from hemorrhagic shock. Biochem Pharmacol. 2015;97:310-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 108. | Iber H, Sewer MB, Barclay TB, Mitchell SR, Li T, Morgan ET. Modulation of drug metabolism in infectious and inflammatory diseases. Drug Metab Rev. 1999;31:29-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 109. | Zhao M, Ma J, Li M, Zhang Y, Jiang B, Zhao X, Huai C, Shen L, Zhang N, He L, Qin S. Cytochrome P450 Enzymes and Drug Metabolism in Humans. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 435] [Article Influence: 108.8] [Reference Citation Analysis (0)] |
| 110. | Ghonem N, Yoshida J, Murase N, Strom SC, Venkataramanan R. Treprostinil Improves Hepatic Cytochrome P450 Activity during Rat Liver Transplantation. J Clin Exp Hepatol. 2012;2:323-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 111. | Ferrigno A, Richelmi P, Vairetti M. Troubleshooting and improving the mouse and rat isolated perfused liver preparation. J Pharmacol Toxicol Methods. 2013;67:107-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 112. | Almazroo OA, Shaik IH, Hughes CB, Humar A, Venkataramanan R. Treprostinil Supplementation Ameliorates Hepatic Ischemia Reperfusion Injury and Regulates Expression of Hepatic Drug Transporters: An Isolated Perfused Rat Liver (IPRL) Study. Pharm Res. 2022;39:2979-2990. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 113. | Hollatz TJ, Musat A, Westphal S, Decker C, D'Alessandro AM, Keevil J, Zhanhai L, Runo JR. Treatment with sildenafil and treprostinil allows successful liver transplantation of patients with moderate to severe portopulmonary hypertension. Liver Transpl. 2012;18:686-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 114. | Chen XB, Xu MQ. Primary graft dysfunction after liver transplantation. Hepatobiliary Pancreat Dis Int. 2014;13:125-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 93] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 115. | Goldaracena N, Cullen JM, Kim DS, Ekser B, Halazun KJ. Expanding the donor pool for liver transplantation with marginal donors. Int J Surg. 2020;82S:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (1)] |
| 116. | Kok B, Dong V, Karvellas CJ. Graft Dysfunction and Management in Liver Transplantation. Crit Care Clin. 2019;35:117-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 117. | Liu J, Man K. Mechanistic Insight and Clinical Implications of Ischemia/Reperfusion Injury Post Liver Transplantation. Cell Mol Gastroenterol Hepatol. 2023;15:1463-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 44] [Reference Citation Analysis (0)] |
| 118. | Almazroo OA, Miah MK, Pillai VC, Shaik IH, Xu R, Dharmayan S, Johnson HJ, Ganesh S, Planinsic RM, Demetris AJ, Al-Khafaji A, Lopez R, Molinari M, Tevar AD, Hughes C, Humar A, Venkataramanan R. An evaluation of the safety and preliminary efficacy of peri- and post-operative treprostinil in preventing ischemia and reperfusion injury in adult orthotopic liver transplant recipients. Clin Transplant. 2021;35:e14298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 119. | Feldman J, Habib N, Fann J, Radosevich JJ. Treprostinil in the treatment of pulmonary arterial hypertension. Future Cardiol. 2020;16:547-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 120. | Chaudhary KR, Deng Y, Suen CM, Taha M, Petersen TH, Mei SHJ, Stewart DJ. Efficacy of treprostinil in the SU5416-hypoxia model of severe pulmonary arterial hypertension: haemodynamic benefits are not associated with improvements in arterial remodelling. Br J Pharmacol. 2018;175:3976-3989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 121. | Corboz MR, Plaunt AJ, Malinin V, Li Z, Gauani H, Chun D, Cipolla D, Perkins WR, Chapman RW. Treprostinil palmitil inhibits the hemodynamic and histopathological changes in the pulmonary vasculature and heart in an animal model of pulmonary arterial hypertension. Eur J Pharmacol. 2022;916:174484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 122. | Huang ST, Xu N, Sun KP, Chen Q, Cao H. Effect of Treprostinil on the Early Postoperative Prognosis of Patients with Severe Left Heart Valvular Disease Combined with Severe Pulmonary Hypertension. Ann Thorac Cardiovasc Surg. 2021;27:18-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 123. | Khan A, White RJ, Meyer G, Pulido Zamudio TR, Jerjes-Sanchez C, Johnson D, Grover R, Broderick M, Ousmanou A, Holdstock L, Michelakis E. Oral treprostinil improves pulmonary vascular compliance in pulmonary arterial hypertension. Respir Med. 2022;193:106744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 124. | Ding M, Tolbert E, Birkenbach M, Akhlaghi F, Gohh R, Ghonem NS. Treprostinil, a prostacyclin analog, ameliorates renal ischemia-reperfusion injury: preclinical studies in a rat model of acute kidney injury. Nephrol Dial Transplant. 2021;36:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 125. | Yajima S, Miyagawa S, Fukushima S, Sakai Y, Iseoka H, Harada A, Isohashi K, Horitsugi G, Mori Y, Shiozaki M, Ohkawara H, Sakaniwa R, Hatazawa J, Yoshioka Y, Sawa Y. Prostacyclin Analogue-Loaded Nanoparticles Attenuate Myocardial Ischemia/Reperfusion Injury in Rats. JACC Basic Transl Sci. 2019;4:318-331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |