Published online Aug 27, 2023. doi: 10.4240/wjgs.v15.i8.1712
Peer-review started: May 6, 2023
First decision: May 19, 2023
Revised: May 26, 2023
Accepted: June 21, 2023
Article in press: June 21, 2023
Published online: August 27, 2023
Processing time: 111 Days and 8 Hours
There are many risk factors for severe acute pancreatitis (SAP) complicated with acute gastrointestinal injury (AGI), but few reports on the interaction between these risk factors.
To analyze the risk factors for SAP complicated with AGI and their interactive effects.
We selected 168 SAP patients admitted to our hospital between December 2019 and June 2022. They were divided into AGI group and non-AGI group according to whether AGI was present. Demographic data and laboratory test data were compared between the two groups. The risk factors for SAP with concomitant AGI were analyzed using multifactorial logistic regression, and an analysis of the interaction of the risk factors was performed.
The percentage of patients with multiple organ dysfunction syndrome, acute physiological and chronic health scoring system II (APACHE II) score, white blood cell count and creatinine (CRE) level was higher in the AGI group than in the non-AGI group. There was a statistically significant difference between the two groups (P < 0.05). Logistic regression analysis indicated that an APACHE II score > 15 and CRE > 100 µmol/L were risk factors for SAP complicating AGI. The interaction index of APACHE II score and CRE level was 3.123.
An APACHE II score > 15 and CRE level > 100 µmol/L are independent risk factors for SAP complicated with AGI, and there is a positive interaction between them.
Core Tip: Acute gastrointestinal injury (AGI) is a common complication of severe acute pancreatitis (SAP). Patients with AGI are prone to gastrointestinal dysfunction and mucosal injury, aggravating the degree of pancreatic inflammation, causing multiple organ dysfunction and endangering patients' lives. In this study, 168 patients with SAP were divided into the AGI group and non-AGI group. The risk factors of SAP complicated with AGI were analyzed, and the interaction of these risk factors was analyzed. The study findings have guiding value for controlling the development of AGI and improving the prognosis of SAP.
- Citation: Chen JH, Zhang MF, Du WC, Zhang YA. Risk factors and their interactive effects on severe acute pancreatitis complicated with acute gastrointestinal injury. World J Gastrointest Surg 2023; 15(8): 1712-1718
- URL: https://www.wjgnet.com/1948-9366/full/v15/i8/1712.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i8.1712
Severe acute pancreatitis (SAP) refers to a disease in which pancreatic enzymes are activated due to a variety of reasons, resulting in a local inflammatory response. This disease is a common critical condition of the digestive system[1,2]. Statistically, the death rate due to SAP is up to 10%-30%[3], and has been on the rise in recent years, which seriously endangers the life and health of patients. Acute gastrointestinal injury (AGI) is a common complication of SAP. AGI patients have gastrointestinal dysfunction and mucosal injury, which can cause gastrointestinal motility slowing, intestinal obstruction, intestinal flora shift, impaired immune function, ulcer, gastrointestinal bleeding, etc., which aggravates the degree of pancreatitis, causes multiple organ dysfunction, and endangers the life of patients[4]. AGI is an important prognostic factor for SAP patients. Relevant studies have found that when AGI occurs in SAP patients, the mortality and incidence of complications are significantly increased[5]. However, there are numerous risk factors for AGI[6,7]. Therefore, examining the risk factors for AGI is of great significance for controlling the development of AGI, improving the prognosis of SAP, and taking effective intervention measures to improve the treatment of patients. However, most studies have investigated the risk factors for AGI, while reports on the interaction between risk factors are few. Therefore, the present study aimed to analyze the risk factors for AGI and determine their interactive effects on SAP to provide a rationale for clinical treatment.
A retrospective analysis of 168 patients with SAP treated in our hospital, and enrolled between December 2019 and June 2022 was conducted. Inclusion criteria were as follows: (1) According to the "Guidelines for the diagnosis and treatment of acute pancreatitis in China (2021)"[8], all patients were diagnosed by abdominal color Doppler ultrasound, CT or MRI; and (2) The age of patients ranged from 18 to 65 years. Exclusion criteria were: (1) Patients with gastrointestinal bleeding and complete intestinal obstruction; (2) Severe heart, kidney or other important organ dysfunction; and (3) Long-term use of corticosteroids or immunosuppressants. According to the AGI diagnostic criteria "European Society for the Critical Care Medicine (2012) Consensus on Acute Gastrointestinal Injury"[9], patients were divided into the AGI group (n = 64) and non-AGI group (n = 104).
Clinical data were collected from the patients. These data included gender, age, comorbidities (hypertension, diabetes, coronary heart disease), smoking history, acute physiological and chronic health scoring system II (APACHE II) score, and multiple organ dysfunction syndrome (MODS). Admission laboratory indicators included white blood cell (WBC) count in peripheral blood, hemoglobin, total bilirubin, creatinine (CRE), and serum amylase.
The SPSS 23.0 software was applied for analysis and processing. Quantitative data that conformed to a normal distribution are shown as mean ± SD, and t-tests were used for comparisons between the groups. Count data are expressed as n (%), and the χ2 test was used for comparisons between the groups. Logistic regression was applied to analyze the associated risk factors. The interaction of two factors was investigated using regression models. The attributable proportion of interaction (API), relative excess risk of interaction (RERI) and the synergy index (S) were calculated. P < 0.05 was considered statistically significant.
Univariate analysis showed that the percentage of patients with MODS, APACHE II score and CRE level were higher in the AGI group than in the non-AGI group, with a significant difference between the two groups (P < 0.05), as shown in Table 1.
| Influencing factors | AGI group (n = 64) | Non-AGI group (n = 104) | χ2/t | P value |
| Gender | 0.464 | 0.496 | ||
| Male | 31 (48.44) | 56 (53.85) | ||
| Female | 33 (51.56) | 48 (4 6.15) | ||
| Age (mean ± SD, yr) | 50.16 ± 7.56 | 49.42 ± 8.12 | 0.583 | 0.560 |
| Hypertension | 0.168 | 0.682 | ||
| Yes | 31 (48.44) | 47 (45.19) | ||
| No | 33 (51.56) | 57 (54.81) | ||
| Diabetes | 0.101 | 0.751 | ||
| Yes | 33 (51.56) | 51 (49.04) | ||
| No | 31 (48.44) | 53 (50.96) | ||
| Coronary heart disease | 0.008 | 0.927 | ||
| Yes | 34 (53.13) | 56 (53.85) | ||
| No | 30 (46.87) | 48 (46.15) | ||
| Smoking | 0.059 | 0.809 | ||
| Yes | 32 (50.00) | 54 (51.92) | ||
| No | 32 (50.00) | 50 (48.08) | ||
| MODS | 21.263 | < 0.001 | ||
| Yes | 43 (67.19) | 32 (30.77) | ||
| No | 21 (32.81) | 72 (69.23) | ||
| APACHE II score (mean ± SD) | 17.45 ± 4.74 | 10.79 ± 3.95 | -9.836 | < 0.001 |
| Leukocytes (mean ± SD, × 109/L) | 15.12 ± 3.03 | 13.87 ± 2.27 | -2.834 | 0.006 |
| Hemoglobin (mean ± SD, g/L) | 140.87 ± 14.93 | 144.50 ± 15.87 | 1.470 | 0.143 |
| Creatinine (mean ± SD, µmol/L) | 115.15 ± 12.18 | 93.07 ± 10.22 | -12.116 | < 0.001 |
| Amylase (mean ± SD, U/L) | 761.43 ± 73.90 | 751.20 ± 70.95 | -0.894 | 0.373 |
| Total bilirubin (mean ± SD, µmol/L) | 22.09 ± 3.68 | 21.78 ± 3.61 | -0.529 | 0.597 |
Variables that were statistically significant in univariate analysis were included as independent variables, and the influencing factor variable assignment is shown in Table 2. The results of the multifactorial regression analysis indicated that an APACHE II score > 15 and CRE > 100 µmol/L were risk factors for complications of AGI in patients with SAP (P < 0.05), as shown in Table 3.
| Influencing factors | Assignment of factors |
| Presence or absence of AGI | 0 = Non-AGI group, 1 = AGI group |
| MODS | 0 = no, 1 = yes |
| APACHE II | ≤ 15 points = 0, > 15 points = 1 |
| Creatinine | ≤ 100 µmol/L = 0, > 100 µmol/L = 1 |
| Leukocytes | Original value input |
| Influencing factors | B value | SE value | Wald value | P value | OR (95%CI) |
| APACHE II | 1.716 | 0.613 | 7.820 | 0.005 | 5.560 (1.671-18.502) |
| MODS | -0.398 | 0.598 | 0.442 | 0.506 | 0.672 (0.208-2.169) |
| Leukocytes | 0.196 | 0.101 | 3.769 | 0.052 | 1.216 (0.998-1.482) |
| Creatinine | 3.380 | 0.553 | 37.366 | < 0.001 | 29.365 (9.936-86.788) |
The RERI of the interaction between the increase in APACHE II score and the increase in CRE level was 220.059, the API was 0.678%, and the S was 3.123. This indicated that there was a positive interaction between the two factors, as shown in Table 4.
| APACHE II | Creatinine | AGI group | Non-AGI group | OR | 95%CI | RERI | API | S |
| 1 | 79 | 1.00 | 220.059 | 0.678 | 3.123 | |||
| + | 5 | 4 | 98.75 | 9.228-1056.778 | ||||
| + | 21 | 12 | 138.25 | 16.998-1124.444 | ||||
| + | + | 37 | 9 | 0.024 | 0.002-0.314 |
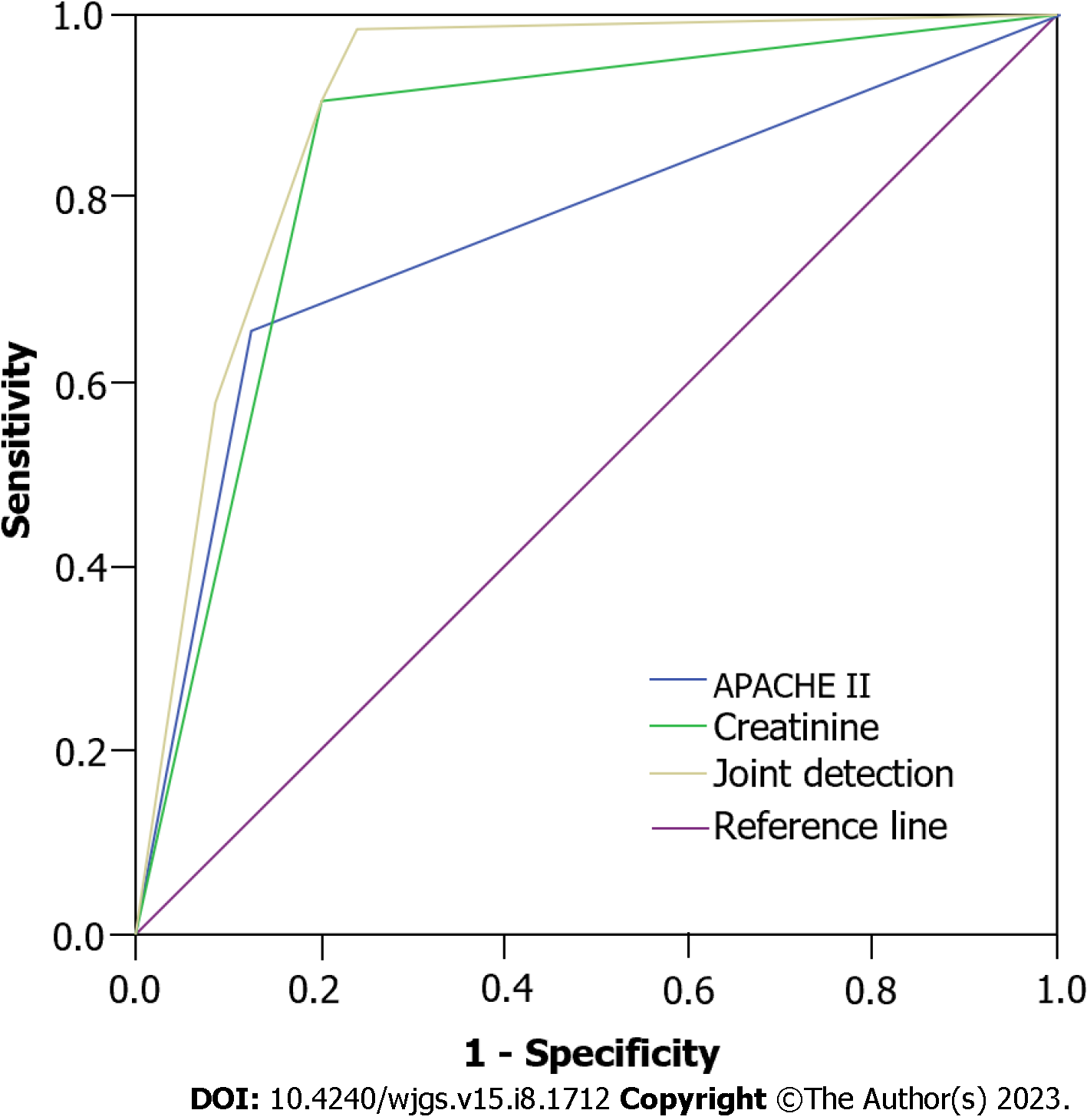
Receiver operating characteristic (ROC) curve analysis showed that the predictive value of joint detection of APACHE II and CRE was better than that of single detection (P < 0.001). The ROC curves of the three were significantly different (P < 0.05) (Figure 1).
SAP is a special type of acute pancreatitis, which is caused by biliary tract disease, overeating, and heavy drinking, which leads to the activation of pancreatic enzymes and an acute chemical inflammatory reaction of pancreatic tissue[10]. In the early stage of SAP, a large number of inflammatory mediators, cytokines and bacterial toxins are produced, which lead to hemodynamic abnormalities and damage to organs such as heart, liver, kidney and the gastrointestinal tract, and in severe cases, organ failure[11]. AGI is one of the most common complications in SAP patients. As the gastrointestinal tract is the reservoir for systemic flora, it has functions such as regulating immune and inflammatory functions. When AGI occurs, it causes intestinal flora shift, gastrointestinal ulcer, gastrointestinal nutrition disorders, etc., which aggravate the inflammatory response, induce multiple organ failure in patients, prolong the length of hospital stay, and increase patient mortality[12]. Wang et al[13] found that AGI was an independent risk factor for SAP. Therefore, active treatment of AGI to promote the recovery of gastrointestinal function is the key to alleviating SAP, reducing mortality, and improving prognosis.
The results of this study indicated that patients with SAP complicated by AGI had a significantly higher MODS ratio, leukocyte level, CRE level, and APACHE II score compared to the non-AGI group, with significant differences. Logistic regression analysis indicated that APACHE II scores > 15 and increased CRE levels were the main risk factors for complications of AGI in SAP. Targeted measures should be taken against the above factors to strengthen prevention. The gastrointestinal tract plays an important role in the human body. Various injuries, surgeries, severe infections, massive bleeding and so on can promote the release of inflammatory factors. These inflammatory factors can activate the signal transduction of nuclear factors in gastrointestinal mucosal epithelium, causing microcirculation disorders in the gastrointestinal tract resulting in impaired gastrointestinal function[14]. The findings in the present study indicate that AGI patients have higher levels of WBCs than non-AGI patients. It is suggested that the increase in these indices may be the risk factors of SAP complicated by AGI. CRE is a product of human muscle metabolism, and increased CRE will have a considerable impact on the body. When the CRE level increases, this indicates that the body's metabolism is abnormal, and a large amount of toxins and waste are accumulated, which results in disordered human functions and leads to various metabolic imbalances[15]. In addition, increased CRE level will accumulate in the heart, respiratory system, gastrointestinal system, etc., and will indirectly reflect glomerular and gastrointestinal system dysfunction, which will lead to gastrointestinal injury and systemic injury[16]. Jin et al[17] found that elevated serum CRE level was a risk factor for gastrointestinal failure, and the results of this study were consistent with these findings.
The APACHE II scoring system consists of a total score of three components: Acute physiology, age, and chronic health status. It is widely applied in the assessment of critically ill patients, and is also a commonly used scoring system to judge the severity of acute pancreatitis[18,19]. An APACHE II score > 15 indicates a poor prognosis, and patients with higher scores have severe disease[20]. Greenberg et al[21] showed that the higher the APACHE II score within 72 h of admission in SAP patients, the higher the death rate. The findings of the present research indicated that patients in the AGI group had higher APACHE II scores than those in the non-AGI group. It is suggested that SAP patients with AGI are more critically ill and have a higher risk of death. The complexity of gastrointestinal function also lies in its internal dynamic changes. Disorder and translocation of intestinal flora is another potential mechanism for the occurrence of AGI. Intestinal flora activate the immune response through the lymphatic system, leading to the occurrence and even deterioration of MODS[22]. This research found a higher percentage of patients with AGI than with non-AGI, which was similar to the findings of Laterre et al[23]. It is suggested that MODS is closely related to SAP complicated by AGI.
From the interaction study of risk factors, it was found that there was a statistically positive interaction between the APACHE II score and CRE level in SAP patients with AGI. The RERI of the interaction effect between high APACHE II score and elevated CRE level was 220.059, indicating that the risk of AGI increased by 220.059 times. The API was 0.678% and S was 3.123, indicating that 0.678% of AGI in these patients was caused by the coexistence of increased APACHE II score and increased CRE level, and the coexistence of both was 3.123 times that of AGI induced by the existence of either factor alone. Therefore, APACHE II score > 15 and CRE level > 100 µmol/L can lead to AGI in SAP patients. The changes in gastrointestinal function should be closely monitored, and timely and effective treatment should be provided to control the development of the patient's disease, reduce the body's inflammatory response, and avoid the involvement of other organs.
The present research was conducted to investigate the risk factors of SAP complicated by AGI and analyze the interaction between these risk factors. In this way, measures to prevent the incidence of AGI were implemented to improve the prognostic outcome of patients with SAP. However, the sample size in this study was limited, and the results may be biased to some extent. It is necessary to expand the sample and conduct a multicenter study to further confirm the risk factors of AGI in SAP patients.
An APACHE II score > 15 and CRE level > 100 µmol/L are both independent risk factors for SAP complicated with AGI, and there is a positive interaction between them. Therefore, in SAP patients with AGI, attention should be paid to managing the risk factors of AGI in SAP patients, and timely and effective interventions should be carried out to reduce the incidence of AGI and to improve the prognosis of SAP patients.
Acute gastrointestinal injury (AGI) patients are prone to gastrointestinal dysfunction and mucosal injury, aggravating the degree of pancreatic inflammation and causing multiple organ dysfunction.
Examining the risk factors of AGI is of great significance for controlling the development of AGI and improving the prognosis of severe acute pancreatitis (SAP).
The purpose of this study was to analyze the risk factors of SAP complicated by AGI and their interaction.
This study retrospectively analyzed SAP patients admitted to our hospital and divided them into the AGI group and non-AGI group to analyze the risk factors of SAP complicated with AGI and their interaction.
An acute physiological and chronic health scoring system II score > 15 and creatinine level > 100 μmol/L were independent risk factors for SAP complicated with AGI, and there was a positive interaction between them.
When risk factors of SAP complicated with AGI are found, timely effective measures should be taken to improve the prognosis of SAP patients.
In SAP patients with AGI, attention should be paid to managing the risk factors of AGI in SAP patients, and timely and effective interventions should be carried out to reduce the incidence of AGI and to improve the prognosis of SAP patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pedziwiatr M, Poland; Sherf-Dagan S, Israel S-Editor: Wang JL L-Editor: A P-Editor: Ji MX
| 1. | Mederos MA, Reber HA, Girgis MD. Acute Pancreatitis: A Review. JAMA. 2021;325:382-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 491] [Article Influence: 122.8] [Reference Citation Analysis (1)] |
| 2. | James TW, Crockett SD. Management of acute pancreatitis in the first 72 hours. Curr Opin Gastroenterol. 2018;34:330-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Liang X, Zhang B, Chen Q, Zhang J, Lei B, Li B, Wei Y, Zhai R, Liang Z, He S, Tang B. The mechanism underlying alpinetin-mediated alleviation of pancreatitis-associated lung injury through upregulating aquaporin-1. Drug Des Devel Ther. 2016;10:841-850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Zhang D, Li Y, Ding L, Fu Y, Dong X, Li H. Prevalence and outcome of acute gastrointestinal injury in critically ill patients: A systematic review and meta-analysis. Medicine (Baltimore). 2018;97:e12970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Hua Z, Su Y, Huang X, Zhang K, Yin Z, Wang X, Liu P. Analysis of risk factors related to gastrointestinal fistula in patients with severe acute pancreatitis: a retrospective study of 344 cases in a single Chinese center. BMC Gastroenterol. 2017;17:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Sun JK, Mu XW, Li WQ, Tong ZH, Li J, Zheng SY. Effects of early enteral nutrition on immune function of severe acute pancreatitis patients. World J Gastroenterol. 2013;19:917-922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 90] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (1)] |
| 7. | Li H, Yang Z, Tian F. Risk factors associated with intolerance to enteral nutrition in moderately severe acute pancreatitis: A retrospective study of 568 patients. Saudi J Gastroenterol. 2019;25:362-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Chinese Pancreatic Surgery Association; Chinese Society of Surgery; Chinese Medical Association. [Guidelines for diagnosis and treatment of acute pancreatitis in China (2021)]. Zhonghua Wai Ke Za Zhi. 2021;59:578-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 9. | Reintam Blaser A, Malbrain ML, Starkopf J, Fruhwald S, Jakob SM, De Waele J, Braun JP, Poeze M, Spies C. Gastrointestinal function in intensive care patients: terminology, definitions and management. Recommendations of the ESICM Working Group on Abdominal Problems. Intensive Care Med. 2012;38:384-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 372] [Cited by in RCA: 364] [Article Influence: 28.0] [Reference Citation Analysis (1)] |
| 10. | Fonseca Sepúlveda EV, Guerrero-Lozano R. Acute pancreatitis and recurrent acute pancreatitis: an exploration of clinical and etiologic factors and outcomes. J Pediatr (Rio J). 2019;95:713-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 11. | Garg PK, Singh VP. Organ Failure Due to Systemic Injury in Acute Pancreatitis. Gastroenterology. 2019;156:2008-2023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 376] [Article Influence: 62.7] [Reference Citation Analysis (0)] |
| 12. | Fu W, Shi N, Wan Y, Mei F, Qiu B, Bao Y, Zhang Y, Hao J, He J, Peng X. Risk Factors of Acute Gastrointestinal Failure in Critically Ill Patients With Traumatic Brain Injury. J Craniofac Surg. 2020;31:e176-e179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Wang M, Lei R. Organ Dysfunction in the Course of Severe Acute Pancreatitis. Pancreas. 2016;45:e5-e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Besterman HS, Mallinson CN, Modigliani R, Christofides ND, Pera A, Ponti V, Sarson DL, Bloom SR. Gut hormones in inflammatory bowel disease. Scand J Gastroenterol. 1983;18:845-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Diago CAA, Señaris JAA. Should we pay more attention to low creatinine levels? Endocrinol Diabetes Nutr (Engl Ed). 2020;67:486-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Levey AS, James MT. Acute Kidney Injury. Ann Intern Med. 2017;167:ITC66-ITC80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 381] [Article Influence: 47.6] [Reference Citation Analysis (0)] |
| 17. | Jin M, Zhang HM, Chen XF, Wu MX, Wang Z, Guo MY, Bai XY, Yang H, Qian JM. [Evaluation and Early Diagnosis of Gastrointestinal Failure in Acute Pancreatitis]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2020;42:47-54. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Tang W, Zha ML, Zhang WQ, Hu SQ, Chen HL. APACHE scoring system and pressure injury risk for intensive care patients: A systematic review and meta-analysis. Wound Repair Regen. 2022;30:498-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Niewiński G, Starczewska M, Kański A. Prognostic scoring systems for mortality in intensive care units--the APACHE model. Anaesthesiol Intensive Ther. 2014;46:46-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Søvik S, Isachsen MS, Nordhuus KM, Tveiten CK, Eken T, Sunde K, Brurberg KG, Beitland S. Acute kidney injury in trauma patients admitted to the ICU: a systematic review and meta-analysis. Intensive Care Med. 2019;45:407-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 21. | Greenberg JA, Hsu J, Bawazeer M, Marshall J, Friedrich JO, Nathens A, Coburn N, May GR, Pearsall E, McLeod RS. Clinical practice guideline: management of acute pancreatitis. Can J Surg. 2016;59:128-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 237] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 22. | Li XY, He C, Zhu Y, Lu NH. Role of gut microbiota on intestinal barrier function in acute pancreatitis. World J Gastroenterol. 2020;26:2187-2193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 69] [Cited by in RCA: 133] [Article Influence: 26.6] [Reference Citation Analysis (3)] |
| 23. | Laterre PF, Collienne C. Improving the management of severe acute pancreatitis: The new guidelines from the French Society of Anaesthesia and Intensive Care Medicine. Anaesth Crit Care Pain Med. 2022;41:101103. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |