Published online Aug 27, 2023. doi: 10.4240/wjgs.v15.i8.1693
Peer-review started: April 11, 2023
First decision: April 26, 2023
Revised: May 5, 2023
Accepted: June 13, 2023
Article in press: June 13, 2023
Published online: August 27, 2023
Processing time: 136 Days and 10.8 Hours
For treatment of hilar cholangiocarcinoma (HCCA), the rate of radical resection is low and prognosis is poor, and preoperative evaluation is not sufficiently accurate. 3D visualization has the advantage of giving a stereoscopic view, which makes accurate resection of HCCA possible.
To establish precise resection of HCCA based on eOrganmap 3D reconstruction and full quantification technology.
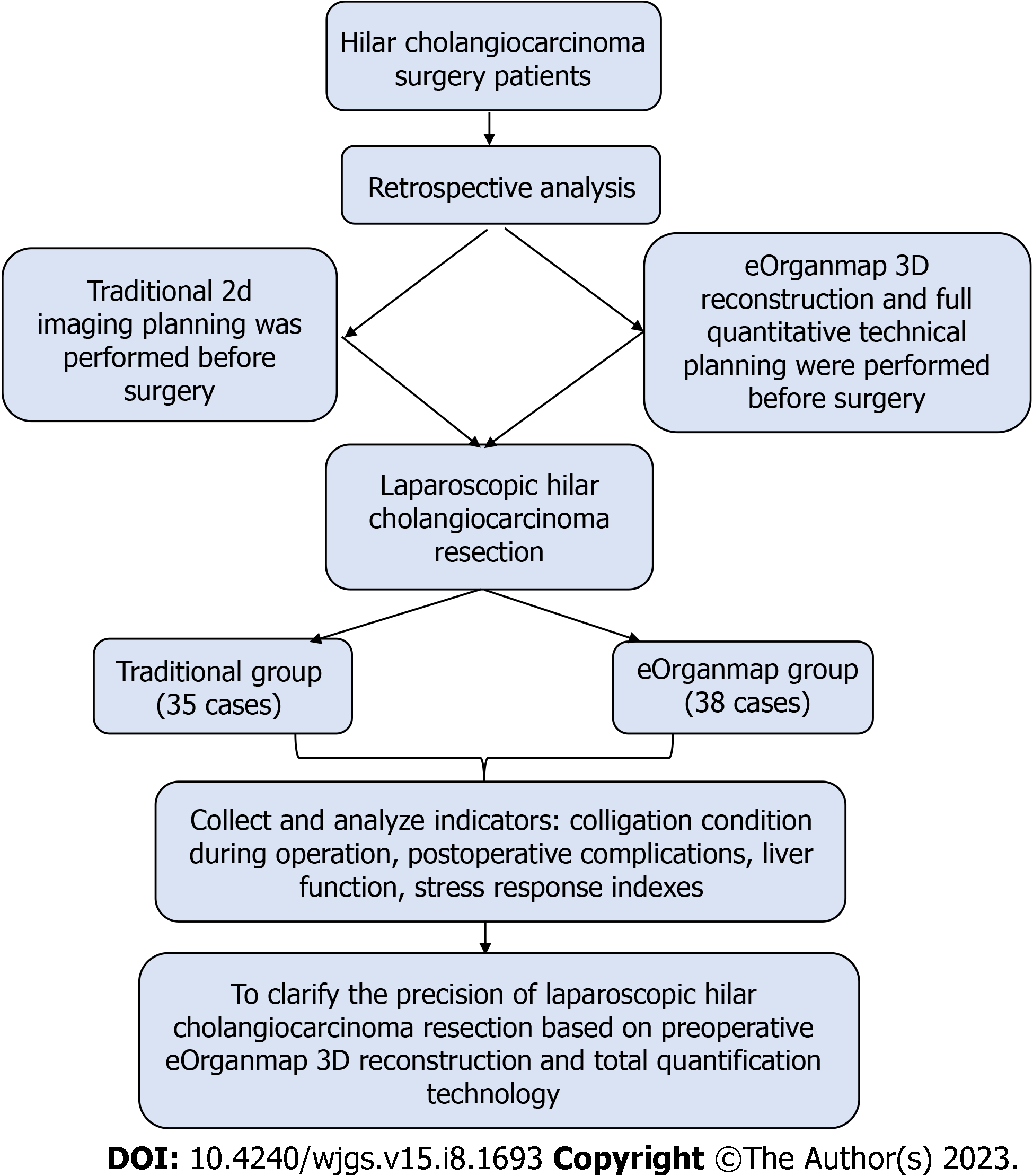
We retrospectively analyzed the clinical data of 73 patients who underwent HCCA surgery. All patients were assigned to two groups. The traditional group received traditional 2D imaging planning before surgery (n = 35). The eOrganmap group underwent 3D reconstruction and full quantitative technical planning before surgery (n = 38). The preoperative evaluation, anatomical classification of hilar hepatic vessels, indicators associated with surgery, postoperative complications, liver function, and stress response indexes were compared between the groups.
Compared with the traditional group, the amount of intraoperative blood loss in the eOrganmap group was lower, the operating time and postoperative intestinal ventilation time were shorter, and R0 resection rate and lymph node dissection number were higher (P < 0.05). The total complication rate in the eOrganmap group was 21.05% compared with 25.71% in the traditional group (P > 0.05). The levels of total bilirubin, Albumin (ALB) , aspartate transaminase, and alanine transaminase in the eOrganmap group were significantly different from those in the traditional group (intergroup effect: F = 450.400, 79.120, 95.730, and 13.240, respectively; all P < 0.001). Total bilirubin, aspartate transaminase, and alanine transaminase in both groups showed a decreasing trend with time (time effect: F = 30.270, 17.340, and 13.380, respectively; all P < 0.001). There was an interaction between patient group and time (interaction effect: F = 3.072, 2.965, and 2.703, respectively; P = 0.0282, 0.032, and 0.046, respectively); ALB levels in both groups tended to increase with time (time effect: F = 22.490, P < 0.001), and there was an interaction effect between groups and time (interaction effect: F = 4.607, P = 0.004). In the eOrganmap group, there was a high correlation between the actual volume of intraoperative liver specimen resection and the volume of preoperative virtual liver resection (t = 0.916, P < 0.001).
The establishment of accurate laparoscopic resection of hilar cholangiocarcinoma based on preoperative eOrganmap 3D reconstruction and full quantization technology can make laparoscopic resection of hilar cholangiocarcinoma more accurate and safe.
Core Tip: The surgical resection rate of hilar cholangiocarcinoma (HCCA) is low, and the overall prognosis is poor. We analyzed 73 patients who underwent HCCA surgery using traditional 2D imaging planning or eOrganmap 3D reconstruction and full quantitative technical planning before surgery. By comparing the preoperative evaluation, anatomical classification of hilar hepatic vessels, indicators associated with surgery, postoperative complications, liver function, and stress response indexes of the two groups of patients, we resolved the problem of poor treatment.
- Citation: Cui DP, Fan S, Guo YX, Zhao QW, Qiao YX, Fei JD. Accurate resection of hilar cholangiocarcinoma using eOrganmap 3D reconstruction and full quantization technique. World J Gastrointest Surg 2023; 15(8): 1693-1702
- URL: https://www.wjgnet.com/1948-9366/full/v15/i8/1693.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i8.1693
Hilar cholangiocarcinoma (HCCA) is a mucosal carcinoma of the common hepatic duct, the left and right hepatic ducts, or the confluence of the left and right hepatic ducts[1]. Although the global incidence of this disease is low, between 1 and 2 per 100000, it shows a significant increasing trend[2]. Radical surgery has made long-term survival and even cure possible for HCCA[3]. However, a variety of factors such as complex anatomical structures and high probability of variation of hilar bile ducts and blood vessels, invasion of tumor adjacent blood vessels, combined with obstructive jaundice, and impaired liver function limit the scope of resection and may lead to low resection rate and poor overall prognosis[4]. At present, there are modified liver dissection, associating liver partition and portal vein ligation for staged hepatectomy, and selective portal vein embolization, but a unified surgical selection strategy has not been formed. From the perspective of surgical anatomy, it is important to study the structure of hilum hepatis and find a reasonable surgical plan for treatment of HCCA. Accurate preoperative evaluation is an important basis for improving the surgical resection rate of HCCA and reducing the risk of surgical mortality[5]. At present, preoperative evaluation of HCCA mainly relies on traditional computed tomography (CT) and magnetic resonance imaging (MRI). Surgeons need to construct 3D models from 2D images in their minds according to clinical experience and anatomical knowledge, which is subjective and will affect the formulation of surgical plans. At the same time, this imaging evaluation method lacks an overall and 3D sense; therefore, it can lead to differences in image interpretation among surgeons[6]. In recent years, 3D visualization has been gradually applied in clinical practice with the advantages of stereoscopic and intuitive vision, and has shown high clinical value and application in preliminary studies on preoperative evaluation of HCCA[7]. However, its reliability still needs the support of more clinical data. In this study, we retrospectively analyzed the clinical data of 73 patients undergoing HCCA surgery in The First Affiliated Hospital of Hebei North University, to explore the application of laparoscopic precise resection of HCCA based on preoperative eOrganmap 3D reconstruction and full quantification.
We retrospectively analyzed clinical data of 73 patients undergoing HCCA surgery in The First Affiliated Hospital of Hebei North University from February 2019 to January 2022. All patients were assigned to two groups. The traditional group received 2D imaging planning before surgery (n = 35). The EOrganmap group underwent 3D reconstruction and full quantitative technical planning before surgery (n = 38). This study was approved by the Medical Ethics Committee of The First Affiliated Hospital of Hebei North University.
The inclusion criteria were as follows: (1) HCCA was diagnosed by preoperative imaging such as CT and MRI, and was diagnosed by postoperative pathology[8]; (2) clear indications for surgery, generally in good condition, with no major heart and lung diseases, and could tolerate anesthesia and surgery after adequate preoperative evaluation; (3) no history of major abdominal trauma or surgery; (4) preoperative liver function assessment was Child–Pugh grade A or B; and (5) pathological data were complete and the treatment compliance was good. The exclusion criteria were: (1) Imaging data showed that the patient had disease other than HCCA; (2) abnormal liver development; (3) extensive tumor metastasis or invasion of important blood vessels; (4) liver function was not significantly improved after the treatment of protecting liver and alleviating jaundice; (5) body mass index > 32 kg/m2; (6) switch to laparotomy; and (7) perioperative death or loss of follow-up. The clinicopathological characteristics of the two groups were similar (Table 1). The study protocol is shown in Figure 1.
| Group | Sex (male/female) | Age (yr, mean ± SD) | Child–Pugh grade A/ B | Preoperative biliary drainage (yes/no) | Bismuth classification | |||
| II | IIIa | IIIb | IV | |||||
| Traditional group (n = 35) | 15/20 | 58.55 ± 5.13 | 29/6 | 27/8 | 3 | 14 | 12 | 6 |
| eOrganmap group (n = 38) | 14/24 | 57.86 ± 5.67 | 34/4 | 30/8 | 1 | 16 | 13 | 8 |
| χ2/t | 0.275 | 0.544 | 0.675 | 0.035 | 1.338 | |||
| P value | 0.600 | 0.588 | 0.411 | 0.852 | 0.720 | |||
The eOrganmap group established preoperative eOrganmap 3D reconstruction and full quantification technology. In order to ensure the accuracy of the 3D reconstruction image, the procedure was carried out by experienced radiologists. The 320-slice spiral CT was used for scanning, the current and voltage were set to 110 mAs and 120kV, respectively, and the layer thickness was 5 mm. We input the original image data into the eOrganmap 3D reconstruction system. The system automatically sketched the contour of each layer of liver parenchyma according to its anatomical position and density, and it could be modified. 3D reconstruction of the tumor, blood vessels, bile ducts, and liver was conducted by a radiologist and a surgeon. Multislice spiral CT and 3D reconstruction image analysis were performed by a radiologist and a surgeon. The analysis included the tumor location and size, whether it invaded the bile duct at grade II or higher, whether it involved peripheral blood vessels, and whether it had lymph node or distant metastasis. The results were compared with the actual intraoperative situation and postoperative pathological results.
Surgical plan planning: Complete the surgical plan design on the computer. The surgical plan should meet the multi-dimensional R0 margin; the residual liver volume should be at least 30% greater than the standard. Ensure that the pre-reserved liver's blood flow and bile drainage are unobstructed. According to the preoperative evaluation, the surgical plan was formulated, and the patients were treated with hemihepatic resection, expanded hemicombined caudate lobectomy, extrahepatic bile duct resection, endoskeletonization of the hepatoduodenal ligament, and bile duct and jejunum Roux-en-Y anastomosis. A five-hole small incision was made to perform laparoscopic surgery, and abdominal exploration was performed for abdominal and distant lymph node metastasis. The hepatoduodenal ligament was dissected by skeletonization, and the liver on the side to be resected was fully dissociated. The pre-resection area was separated along the hepatic ischemia line and the whole specimen was resected after an appropriate blood flow blocking method was selected. Rapid cryoscopy was performed to determine whether the upper and lower resection margins reached the R0 resection level. After the trans-sectional bile duct was reconstructed, biliary anastomosis was performed with Roux-en-Y. All patients were followed up for 10 mo after surgery.
For preoperative evaluation, HCCA tumor progression[9] was evaluated in two aspects: Longitudinal progression (tumor invasion along the bile duct) and vertical progression (tumor invasion through the bile duct into the adjacent portal vein and hepatic artery in the vertical direction). Bismuth–Corlette classification was used for longitudinal progression. For patients in the eOrganmap group, only the tumor and biliary system were displayed after removing other tissues in the 3D model. Longitudinal invasion information was obtained by rotating the field of vision, and the tumor and portal vein or hepatic artery were separately displayed in the 3D model to observe the relationship between the tumor and vasculature from multiple angles. For patients in the traditional group, surgeons judged the degree of longitudinal progression from the CT images, such as middle bile duct stenosis and intraluminal space occupation. The Baek classification[10] was used as the standard to evaluate the degree of hepatic artery and portal vein invasion. Grade 0 tumor invasion indicated no vascular invasion; Grade I indicated that the blood vessels were stained or moved (the tumor was adjacent to the blood vessels); Grade Ⅱ indicated that the tumor had fused to the blood vessel and completely enclosed it[11]. The Couniaud method was used for bile duct anatomical classification[12], the Cheng method for portal vein classification[13], and the Michels method for hepatic artery variation classification[14].
Indicators associated with surgery: Surgical margin pathology, number of lymph nodes dissected, operating time, amount of intraoperative blood loss, postoperative intestinal ventilation time, and postoperative hospital stay. Postoperative complications included bile leakage, abdominal fluid accumulation, lung infection, postoperative liver insufficiency, and stress ulcers. Evaluation of postoperative bile leakage was based on the diagnostic criteria of the International Liver Surgery Research Group[15]. Total bilirubin (TBIL) level in the abdominal drainage tube was three times higher than in the serum on postoperative day 3. Liver function was detected preoperatively (T1), and on postoperative day 1 (T2), postoperative day 3 (T3), and postoperative day 7 (T4), and the indexes included TBIL, alanine transaminase (ALT), aspartate aminotransferase (AST), and albumin (ALB).
Stress response indexes were: Interleukin (IL)-6, cortisol (Cor), and norepinephrine (NE). For detection, 5 mL venous blood was collected, centrifuged for 10 min at 3000 rpm (Heidelge Medical Equipment, Building 3, 229 Amber Road, Shanghai International Medical Park, Pudong New Area, Shanghai), and the serum was separated and stored at -20°C for testing. ELISA was used to detect the above indicators.
For patients in the eOrganmap group, the software module was used to automatically calculate the volume of each segment of the liver, and the volume of the excised liver was measured by the drainage method after surgery, and the volume of the virtual excised liver measured by 3D reconstruction before surgery was compared with the actual volume of the excised liver specimen during surgery. For the drainage method[16], the excised liver and tumor specimens were wrapped in cling film and placed in a container filled with water. The overflow water was collected and the volume was measured in a measuring cup, which corresponded to the specimen volume.
SPSS 22.0 was used for statistical analysis. The measurement data in line with normal distribution were expressed as mean ± SD. The t test was used for comparison of measurement data in the two groups, and repeated-measurement analysis of variance was used for comparison of data at different time points between groups. Numerical data were represented by n (%) and χ2 test. The χ2 value was corrected when theoretical frequency was ≥ 1 and < 5, and calculated by exact probability method when theoretical frequency < 1. Pearson correlation test was used for correlation analysis. P < 0.05 was considered statistically significant.
The accuracy of longitudinal progression was 89.47% (34/38) in the eOrganmap group compared with 82.86% (29/35) in the conventional group (χ2 = 0.231, P = 0.631). The accuracy of vertical progression in the eOrganmap group was compared with that in the traditional group: Portal vein invasion: 94.74% (36/38) vs 91.43% (32/35) (χ2 = 0.009, P = 0.924); hepatic artery invasion: 89.47% (34/38) vs 85.71% (30/35) (χ2 = 0.017, P = 0.895).
In the eOrganmap group, seven cases of hepatic artery anatomical variation, three of portal vein variation, and four of bile duct anatomical variation were found preoperatively. All the results of preoperative evaluation were identical with the results of intraoperative exploration, and the classification accuracy was 100%. In the traditional group, four cases of hepatic artery anatomical variation, two of portal vein variation, and three of bile duct anatomical variation were found preoperatively. The typing accuracy was 64.29% in three cases of hepatic artery variation, one of portal vein variation and one of bile duct variation. Comparison of typing accuracy between the eOrganmap and traditional groups was χ2 = 8.027 and P = 0.005.
Compared with the traditional group, the amount of intraoperative blood loss in the eOrganmap group was lower, the operating time and postoperative intestinal ventilation time were shorter, and R0 resection rate and lymph node dissection number were higher (P < 0.05) (Table 2).
| Group | Traditional group (n = 35) | eOrganmap group (n = 38) | t/χ2 | P value |
| Surgical procedure, n (%) | 1.276 | 0.865 | ||
| Left/right half liver + caudate lobectomy | 23 (65.71) | 27 (71.05) | ||
| Extended hemihepatectomy + caudate lobectomy | 6 (17.14) | 7 (18.42) | ||
| Liver trilobites + caudate lobectomy | 2 (5.71) | 2 (5.26) | ||
| Mesohepatectomy + caudate lobectomy | 1 (2.86) | 1 (2.63) | ||
| Other | 3 (8.57) | 1 (2.63) | ||
| Amount of intraoperative blood loss (mean ± SD, mL) | 772.52 ± 112.13 | 553.62 ± 98.56 | 8.875 | < 0.001 |
| Operating time (mean ± SD, min) | 645.29 ± 121.14 | 523.19 ± 103.15 | 4.648 | < 0.001 |
| Surgical margin pathology, n (%) | 4.425 | 0.035 | ||
| R0 | 29 (82.86) | 37 (97.37) | ||
| R1 | 6 (17.14) | 1 (2.63) | ||
| No. of lymph nodes dissected (mean ± SD) | 9.12 ± 2.34 | 10.75 ± 2.58 | 2.819 | 0.006 |
| Postoperative intestinal ventilation time (mean ± SD, d) | 3.15 ± 1.02 | 2.65 ± 0.71 | 2.447 | 0.017 |
| Postoperative hospital stay (mean ± SD, d) | 22.64 ± 5.26 | 21.15 ± 4.87 | 1.257 | 0.213 |
The total complication rate in the eOrganmap group was 21.05%, compared with 25.71% in the traditional group (P > 0.05) (Table 3). All patients with postoperative complications were cured after conservative treatment.
| Complication | Traditional group (n = 35) | eOrganmap group (n = 38) | χ2/Z | P value |
| Bile leakage | 2 (5.71) | 2 (5.26) | 2.149 | 0.708 |
| Abdominal fluid accumulation | 3 (8.57) | 3 (7.89) | ||
| Lung infection | 3 (8.57) | 2 (5.26) | ||
| Postoperative liver insufficiency | 1 (2.86) | 0 (0.00) | ||
| Stress ulcers | 0 (0.00) | 1 (2.63) | ||
| Total complication rate | 9 (25.71) | 8 (21.05) | 0.222 | 0.638 |
The levels of TBIL, ALB, AST, and ALT in the eOrganmap group were significantly different from those in the traditional group (intergroup effect: F = 450.40, 79.120, 95.730, and 13.240, respectively; all P < 0.001). TBIL, AST, and ALT in both groups showed a decreasing trend with time (time effect: F = 30.270, 17.340, and 13.380, respectively; all P < 0.001), and there was an interaction effect between grouping and time (F = 3.072, 2.965, and 2.703, respectively; P = 0.0282, 0.032, and 0.046, respectively); ALB levels in both groups tended to increase with time (time effect: F = 22.490, P < 0.001), and there was an interaction effect between groups and time (interaction effect: F = 4.607, P = 0.004) (Table 4 and Table 5).
| Time | TBIL (μmol/L) | ALB (g/L) | ||||||
| Traditional group (n = 35) | eOrganmap group (n = 38) | t | P value | Traditional group (n = 35) | eOrganmap group (n = 38) | t | P value | |
| T1 | 211.26 ± 15.31 | 209.58 ± 16.75 | 0.446 | 0.657 | 27.69 ± 4.13 | 23.16 ± 3.83 | 4.863 | < 0.001 |
| T2 | 165.28 ± 14.37 | 151.22 ± 12.58 | 4.456 | < 0.001 | 29.39 ± 4.02 | 27.24 ± 4.12 | 2.253 | 0.027 |
| T3 | 148.56 ± 17.28 | 140.37 ± 15.47 | 2.137 | 0.036 | 32.25 ± 3.23 | 30.22 ± 3.54 | 2.552 | 0.013 |
| T4 | 128.62 ± 14.39 | 113.28 ± 15.27 | 4.408 | < 0.001 | 34.66 ± 3.15 | 34.85 ± 4.41 | 0.210 | 0.834 |
| Time | AST (U/L) | ALT (U/L) | ||||||
| Traditional group (n = 35) | eOrganmap group (n = 38) | t | P value | Traditional group (n = 35) | eOrganmap group (n = 38) | t | P value | |
| T1 | 112.17 ± 28.42 | 108.62 ± 30.23 | 0.516 | 0.608 | 122.15 ± 32.48 | 123.49 ± 31.58 | 0.179 | 0.859 |
| T2 | 81.82 ± 10.67 | 75.38 ± 15.43 | 2.057 | 0.043 | 112.41 ± 24.15 | 101.21 ± 23.24 | 2.019 | 0.047 |
| T3 | 75.25 ± 10.58 | 70.26 ± 6.38 | 2.462 | 0.016 | 108.36 ± 25.58 | 95.26 ± 26.31 | 2.154 | 0.035 |
| T4 | 74.85 ± 9.20 | 56.12 ± 8.39 | 9.098 | < 0.001 | 107.25 ± 28.56 | 82.28 ± 30.25 | 3.619 | < 0.001 |
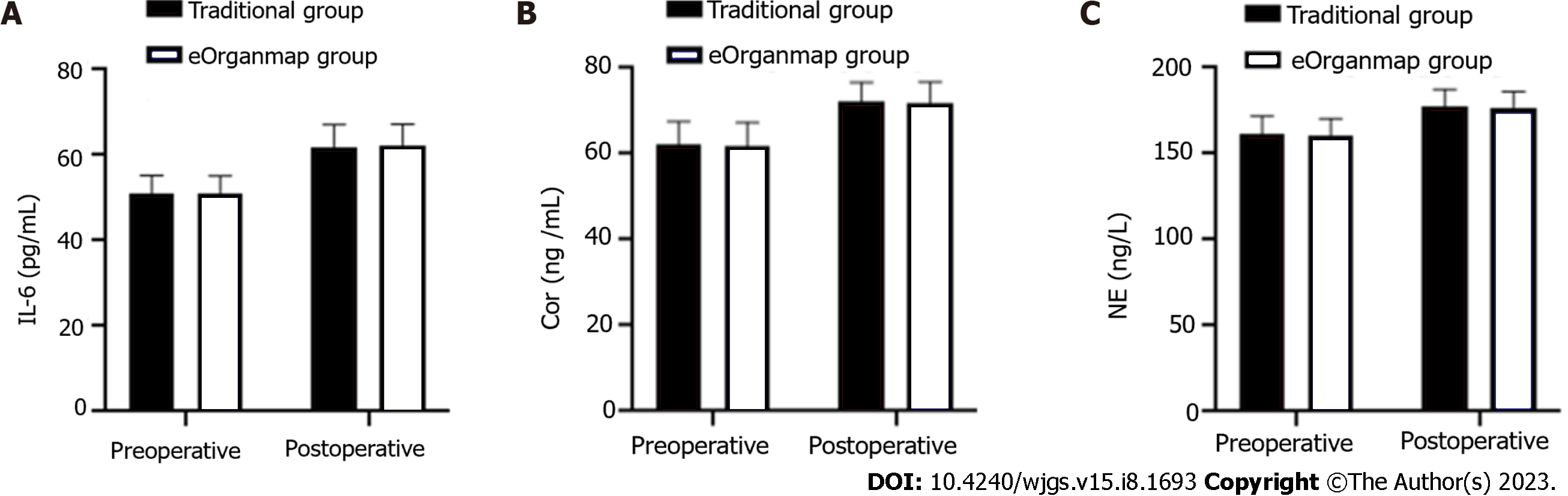
The levels of IL-6, Cor and NE in the eOrganmap group and traditional group were compared before and after surgery (P > 0.05) (Table 6 and Figure 2).
| Indicators | Traditional group (n = 35) | eOrganmap group (n = 38) | χ2/Z | P value |
| IL-6 (pg/mL) | ||||
| Pre-operation | 50.89 ± 4.42 | 51.02 ± 4.16 | 0.130 | 0.897 |
| Post-operation | 61.66 ± 5.48 | 62.07 ± 5.14 | 1.243 | 0.742 |
| Cor (ng/mL) | ||||
| Pre-operation | 62.35 ± 5.16 | 61.75 ± 5.58 | 0.476 | 0.636 |
| Post-operation | 72.22 ± 4.48 | 71.74 ± 5.03 | 0.429 | 0.669 |
| NE (ng/L) | ||||
| Pre-operation | 161.53 ± 10.38 | 160.85 ± 9.47 | 0.293 | 0.771 |
| Post-operation | 177.25 ± 10.12 | 176.95 ± 9.13 | 0.133 | 0.894 |
In the eOrganmap group, the preoperative virtual resection volume was 523.45 ± 112.03 mL, and the actual intraoperative resection volume was 558.43 ± 125.41 mL. There was a high correlation between the actual intraoperative resection volume and the preoperative virtual resection volume (t = 0.916, P < 0.001).
The prevalence of HCCA is increasing annually, and surgical resection is the main treatment. Accurate preoperative evaluation of HCCA and optimal surgical planning are important for good prognosis. In recent years, digital medical technology and the concept of 3D visualization precision diagnosis and treatment have been widely promoted and practiced. The 3D visualization and 3D printed models are more intuitive and accurate than traditional 2D CT and MRI images, making it possible to achieve accurate diagnosis, preoperative evaluation, and accurate surgery.
In this study, laparoscopic precise resection of HCCA was established based on preoperative eOrganmap 3D reconstruction and full quantification technology, which achieved good results. In the evaluation of degree of tumor invasion, we found that there was no difference in the accuracy of preoperative evaluation results and postoperative actual results between the two groups. Bismuth–Corlette classification is the most commonly used clinical classification method, which divides HCCA into types I–IV according to the extent of bile duct invasion by tumor. At present, the formulation of HCCA surgical plan is mainly based on this classification. However, there is no unified standard for surgical procedures established according to this classification method, and Bismuth–Corlette classification does not take into account tumor invasion of the portal vein and hepatic artery, which also affects the choice of surgical procedure. The eOrganmap 3D reconstruction and full quantification can make up for the deficiency of traditional preoperative evaluation methods.
Our results showed that the classification accuracy of patients based on preoperative eOrganmap 3D reconstruction and full quantification technology was significantly increased. The images based on eOrganmap 3D reconstruction and full quantification technology clearly showed the anatomical variation of the hilar liver. As a 3D visualization technology, eOrganmap 3D reconstruction and full quantification technology uses high-quality 2D-enhanced CT images or MR images to carry out 3D reconstruction, so as to display the lesions’ location, size, scope, and their anatomical relationship with the hepatic artery and portal vein in a 3D, comprehensive, and multiangular manner. According to this information, the tumor can be judged whether it has vascular invasion[17]. At the same time, it can evaluate the anatomical variation and spatial conformation of the hepatic artery, portal vein and bile duct, accurately measure the volume of each hepatic segment, and calculate the residual liver volume[18]. Accurate assessment of variation of the hepatic artery, portal vein and hepatic vein is important to surgical planning and avoidance of accidental injury during surgery[19]. In terms of vascular reconstruction, as long as CT image layer is thin enough, 3D software can automatically generate a vascular boundary without manual drawing, which reduces the secondary error caused by manual drawing. The 3D vascular images can intuitively discover the variation in blood vessels and the relationship between tumors and blood vessels, which could improve the accuracy of resectable evaluation[20]. eOrganmap 3D reconstruction and full quantification technology is a new development of CT reconstruction. This technique can register and fuse images of different scanning periods, displaying liver, hepatic artery, portal vein, hepatic vein, and bile duct singly or in combination in the same 3D model, which can be observed by several physicians simultaneously[21,22]. Through the adjustment of transparency, the internal structure can be displayed, so that the spatial deformation of the important tubular structure in the liver can be observed, and an individualized surgical plan formulated. Couinaud’s anatomical segmentation can be carried out to achieve virtual surgery. Surgical information can be quantified through the built-in measurement tools of the software. The eOrganmap 3D reconstruction and full quantification technology has transformed the previous qualitative evaluation into quantitative evaluation, so as to accurately carry out individualized preoperative evaluation and surgical planning, which is consistent with the development of precision surgery.
Preoperative reasonable planning of surgery, prior understanding of the anatomical variation of the perihilar bile duct and blood vessels, and possible intraoperative conditions could reduce the possibility of accidental intraoperative injury of the bile duct and blood vessels, thus avoiding the blindness of intraoperative exploration, and improving the safety of surgery and reducing liver dysfunction[23]. eOrganmap 3D reconstruction and full quantification technology can accurately measure liver volume, which prevents postoperative liver failure and ensures the safety of HCCA surgery. The results of this study showed that laparoscopic HCCA resection based on preoperative eOrganmap 3D reconstruction and full quantification technology reduced intraoperative blood loss, shortened operating time, and promoted postoperative intestinal ventilation, without increasing the incidence of complications and alleviating liver function damage. The results of this study also showed that the R0 resection rate and lymph node dissection number in the eOrganmap group were higher, indicating that 3D reconstruction and full quantification had some advantages in surgical margin treatment and lymph node dissection. Surgical margin and lymph node metastasis are both important factors affecting the prognosis of patients with hilar tumor[24]. Improving R0 resection rate and lymph node dissection are important measures to improve therapeutic efficacy and prognosis. Therefore, we hypothesized that laparoscopic HCCA resection based on preoperative eOrganmap 3D reconstruction and full quantification would promote efficacy and improve prognosis. There was a high correlation between the actual volume of intraoperative liver resection and the volume of preoperative virtual liver resection in the eOrganmap group. Accurate calculation of residual liver volume was important to ensure the safety of hepatectomy. Conventional CT or MRI integral measurement method was difficult to complete the measurement of segmental liver volume; however, preoperative eOrganmap 3D reconstruction and full quantification technology could accurately measure the volume of each segment of liver through a portal vein drainage algorithm, and it was consistent with the actual postoperative situation. In conclusion, accurate measurement of liver volume provides a reliable guarantee for the realization of accurate liver resection.
This study was the first to systematically carry out a new liver segmentation method based on three-dimensional reconstruction visualization and comprehensive quantification technology and the establishment of new indicators for liver reserve function evaluation and used a variety of mathematical models to analyze its feasibility and accuracy, providing a potential evaluation method for preoperative planning and postoperative risk prediction of hilar cholangiocarcinoma. On this basis, laparoscopic precise resection of HCCA was convenient for the application and promotion of this technology. However, this study also had some shortcomings. This study was retrospective and lacked prospective randomized controlled trials, so the reliability of the results could not be guaranteed. In addition, the number of cases included in this study was small, and the results may be biased, which needs to be confirmed by studies with a larger sample size.
Laparoscopic precise resection of HCCA based on preoperative eOrganmap 3D reconstruction and full quantification technology made preoperative assessment, hilar vasculature anatomical classification, and resected liver volume assessment more accurate. It improved the rate of R0 resection and the number of lymph nodes dissected. It also had a low impact on liver function and stress response. Therefore, the method is safe and worthy of wider application.
The incidence of hilar cholangiocarcinoma (HCCA) has shown a significant upward trend, and radical surgery is an effective treatment. However, the complexity of the anatomical structure of the hilar bile duct and blood vessels, the invasion of the adjacent blood vessels of the tumor, jaundice, and the scope of hepatectomy have resulted in a low resection rate for HCCA and poor prognosis.
The preoperative evaluation of HCCA mainly relies on traditional computed tomography and magnetic resonance imaging. Surgeons need to construct 2D images into 3D models in their minds based on clinical experience and anatomical knowledge. Such a method is subjective and will affect the formulation of surgical plans.
This study aimed to establish a laparoscopic precise resection of HCCA based on preoperative eOrganmap 3D reconstruction and full quantification technology, to provide a new method for precise treatment of HCCA.
We retrospectively analyzed the clinical data of 73 patients with HCCA who underwent surgery. Patients were divided into the traditional group (2D imaging planning before surgery) and eOrganmap group (3D reconstruction and full quantification technology planning before surgery). To compare the relevant indicators of the two groups of patients and to further explore the difference between eOrganmap 3D reconstruction and full quantification technology and traditional 2D image planning treatment.
eOrganmap 3D reconstruction and full quantification technology planning have obvious advantages in classification accuracy, blood loss, operating time, postoperative intestinal ventilation time, R0 resection rate, number of lymph nodes dissected, total complication rate, and liver function. In the eOrganmap group, there was a high correlation between the volume of the actual resected liver specimen and the volume of the virtual resected liver specimen before the operation.
Establishing laparoscopic precise resection of hilar cholangiocarcinoma based on preoperative eOrganmap 3D reconstruction and full quantification technology can make laparoscopic HCCA resection more accurate and safe.
The results of this study were verified by a retrospective study with a large sample size, which enhanced the reliability of the results and contributed to the clinical promotion of eOrganmap 3D reconstruction and full quantification technology.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhangu A, United Kingdom; Garcia K, Spain S-Editor: Wang JL L-Editor: A P-Editor: Ji MX
| 1. | Abou-Alfa GK, Macarulla T, Javle MM, Kelley RK, Lubner SJ, Adeva J, Cleary JM, Catenacci DV, Borad MJ, Bridgewater J, Harris WP, Murphy AG, Oh DY, Whisenant J, Lowery MA, Goyal L, Shroff RT, El-Khoueiry AB, Fan B, Wu B, Chamberlain CX, Jiang L, Gliser C, Pandya SS, Valle JW, Zhu AX. Ivosidenib in IDH1-mutant, chemotherapy-refractory cholangiocarcinoma (ClarIDHy): a multicentre, randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2020;21:796-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 557] [Cited by in RCA: 715] [Article Influence: 143.0] [Reference Citation Analysis (0)] |
| 2. | Li H, Zhang ZY, Zhou ZQ, Guan J, Tong DN, Zhou GW. Combined gemcitabine and S-1 chemotherapy for treating unresectable hilar cholangiocarcinoma: a randomized open-label clinical trial. Oncotarget. 2016;7:26888-26897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Ma D, Wang W, Wang J, Zhang T, Jiang Z, Du G, Yang J, Zhang X, Qin G, Jin B. Laparoscopic versus open surgery for hilar cholangiocarcinoma: a retrospective cohort study on short-term and long-term outcomes. Surg Endosc. 2022;36:3721-3731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Matsuo K, Rocha FG, Ito K, D'Angelica MI, Allen PJ, Fong Y, Dematteo RP, Gonen M, Endo I, Jarnagin WR. The Blumgart preoperative staging system for hilar cholangiocarcinoma: analysis of resectability and outcomes in 380 patients. J Am Coll Surg. 2012;215:343-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 157] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 5. | Peng Y, Zhao Z, Zhao Y, Wang Z, Li J, Zhang H, Liu X, Zhou X. Three-dimensional reconstruction of magnetic resonance images of carp brain for brain control technology. J Neurosci Methods. 2022;366:109428. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Pang L, Bo X, Wang J, Wang C, Wang Y, Liu G, Yu H, Chen L, Shi H, Liu H. Role of dual-time point (18)F-FDG PET/CT imaging in the primary diagnosis and staging of hilar cholangiocarcinoma. Abdom Radiol (NY). 2021;46:4138-4147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Kelkar A, Kelkar J, Chougule Y, Bolisetty M, Singhvi P. Cognitive workload, complications and visual outcomes of phacoemulsification cataract surgery: Three-dimensional versus conventional microscope. Eur J Ophthalmol. 2022;32:2935-2941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | You Y, Heo JS, Shin SH, Shin SW, Park HS, Park KB, Cho SK, Hyun D, Han IW. Optimal timing of portal vein embolization (PVE) after preoperative biliary drainage for hilar cholangiocarcinoma. HPB (Oxford). 2022;24:635-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Gomez DR, Blumenschein GR Jr, Lee JJ, Hernandez M, Ye R, Camidge DR, Doebele RC, Skoulidis F, Gaspar LE, Gibbons DL, Karam JA, Kavanagh BD, Tang C, Komaki R, Louie AV, Palma DA, Tsao AS, Sepesi B, William WN, Zhang J, Shi Q, Wang XS, Swisher SG, Heymach JV. Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: a multicentre, randomised, controlled, phase 2 study. Lancet Oncol. 2016;17:1672-1682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 747] [Cited by in RCA: 840] [Article Influence: 93.3] [Reference Citation Analysis (0)] |
| 10. | Baek SY, Sheafor DH, Keogan MT, DeLong DM, Nelson RC. Two-dimensional multiplanar and three-dimensional volume-rendered vascular CT in pancreatic carcinoma: interobserver agreement and comparison with standard helical techniques. AJR Am J Roentgenol. 2001;176:1467-1473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | He M, Li Q, Zou R, Shen J, Fang W, Tan G, Zhou Y, Wu X, Xu L, Wei W, Le Y, Zhou Z, Zhao M, Guo Y, Guo R, Chen M, Shi M. Sorafenib Plus Hepatic Arterial Infusion of Oxaliplatin, Fluorouracil, and Leucovorin vs Sorafenib Alone for Hepatocellular Carcinoma With Portal Vein Invasion: A Randomized Clinical Trial. JAMA Oncol. 2019;5:953-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 381] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 12. | Ludwig K, Santoro L, Ingravallo G, Cazzato G, Giacometti C, Dall'Igna P. Congenital anomalies of the gastrointestinal tract: the liver, extrahepatic biliary tree and pancreas. Pathologica. 2022;114:55-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Cheng YF, Huang TL, Lee TY, Chen TY, Chen CL. Variation of the intrahepatic portal vein; angiographic demonstration and application in living-related hepatic transplantation. Transplant Proc. 1996;28:1667-1668. [PubMed] |
| 14. | Fang CH, Huang YP, Chen ML, Lu CM, Li XF, Qiu WF. Digital medical technology based on 64-slice computed tomography in hepatic surgery. Chin Med J (Engl). 2010;123:1149-1153. [PubMed] |
| 15. | Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 948] [Cited by in RCA: 1413] [Article Influence: 100.9] [Reference Citation Analysis (0)] |
| 16. | Hogan MC, Chamberlin JA, Vaughan LE, Waits AL, Banks C, Leistikow K, Oftsie T, Madsen C, Edwards M, Glockner J, Kremers WK, Harris PC, LaRusso NF, Torres VE, Masyuk TV. Pansomatostatin Agonist Pasireotide Long-Acting Release for Patients with Autosomal Dominant Polycystic Kidney or Liver Disease with Severe Liver Involvement: A Randomized Clinical Trial. Clin J Am Soc Nephrol. 2020;15:1267-1278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Yamada K, Endo H, Tetsunaga T, Miyake T, Sanki T, Ozaki T. Accuracy of Cup Positioning With the Computed Tomography-Based Two-dimensional to Three-Dimensional Matched Navigation System: A Prospective, Randomized Controlled Study. J Arthroplasty. 2018;33:136-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Yang SF, Powell A, Srinivasan S, Kim JC, Baker SR, Green GE, Zopf DA. Addressing the Pandemic Training Deficiency: Filling the Void with Simulation in Facial Reconstruction. Laryngoscope. 2021;131:E2444-E2448. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Dala Riva DF, Nacif LS, Fernandes MR, Silva NA, Pinheiro RS, Rocha-Santos V, De Martino RB, Waisberg DR, Macedo RA, Ducatti L, De Paiva Haddad LB, Galvão FHF, Andraus W, Carneiro-D'Albuquerque L. Relationship of Anatomic Variations and Arterial Reconstruction of the Hepatic Artery: Prevalence and Effect on Orthotopic Liver Transplantation. Transplant Proc. 2022;54:1313-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 20. | Acar G, Cicekcibasi AE, Koplay M, Seher N. Anatomical Variations of the Celiac Trunk and Hepatic Arteries with a New Classification, Based on CT Angiography. J Coll Physicians Surg Pak. 2022;32:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Smillie RW, Williams MA, Richard M, Cosker T. Producing three-dimensional printed models of the hepatobiliary system from computed tomography imaging data. Ann R Coll Surg Engl. 2021;103:41-46. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Cannella R, Sartoris R, Grégory J, Garzelli L, Vilgrain V, Ronot M, Dioguardi Burgio M. Quantitative magnetic resonance imaging for focal liver lesions: bridging the gap between research and clinical practice. Br J Radiol. 2021;94:20210220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Damle-Vartak A. 3D visualization of the biliary tree by X-ray phase-contrast computed tomography. Arch Toxicol. 2018;92:3601-3602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Buettner S, Margonis GA, Kim Y, Gani F, Ethun CG, Poultsides G, Tran T, Idrees K, Isom CA, Fields RC, Krasnick B, Weber SM, Salem A, Martin RC, Scoggins CR, Shen P, Mogal HD, Schmidt C, Beal E, Hatzaras I, Shenoy R, Maithel SK, Pawlik TM. Conditional probability of long-term survival after resection of hilar cholangiocarcinoma. HPB (Oxford). 2016;18:510-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |