Published online Jun 27, 2023. doi: 10.4240/wjgs.v15.i6.1256
Peer-review started: February 21, 2023
First decision: March 14, 2023
Revised: April 4, 2023
Accepted: April 20, 2023
Article in press: April 20, 2023
Published online: June 27, 2023
Processing time: 106 Days and 22.4 Hours
Small bowel diverticula are rare in clinics, and small intestinal obstruction caused by coprolites is rarer and difficult to diagnose early. The true incidence of these diverticula may be underestimated due to their clinical symptoms not differing from those of small bowel obstruction resulting from other causes. It is common in the elderly, although it can occur at any age.
This is a case report of a 78-year-old man with epigastric pain for 5 d. Conservative treatment does not effectively relieve pain, inflammatory indicators are elevated, and computed tomography suggests jejunal intussusception and mild ischemic changes in the intestinal wall. Laparoscopic exploration showed that the left upper abdominal loop was slightly edematous, the jejunum mass at the near Flex ligament was palpable, the size was about 7 cm × 8 cm, the local movement was slight, and the diverticulum was seen 10 cm downward, and the local small intestine was dilated and edema. Segmentectomy was performed. After the short parenteral nutrition after surgery, the fluid and enteral nutrition solution were pumped through the jejunostomy tube, and the patient was discharged after the treatment was stable, and the jejunostomy tube was removed in an outpatient clinic one month after the operation. Postoperative pathology: Jejunectomy specimen: (1) Small intestinal diverticulum with chronic inflammation, ulcer with full-thickness activity, and necrosis of the intestinal wall in some areas; (2) also see that the hard object is consistent with stone changes; and (3) the incision margin on both sides shows chronic inflammation of mucosal tissue.
Clinically, the diagnosis of small bowel diverticulum is difficult to distinguish from jejunal intussusception. Combined with the patient’s condition, rule out other possibilities after a timely disease diagnosis. According to the patient’s body tolerance adopt personalized surgical methods to achieve better recovery after surgery.
Core Tip: Small bowel diverticulum is clinically rare because it lacks specific clinical symptoms and has many complications. This case report presents a patient with a small bowel diverticulum with fecalith-causing intestinal obstruction diagnosed and treated by the Department of General Surgery of Jiangsu Provincial Hospital of Traditional Chinese Medicine.
- Citation: Wang LW, Chen P, Liu J, Jiang ZW, Liu XX. Small bowel diverticulum with enterolith causing intestinal obstruction: A case report. World J Gastrointest Surg 2023; 15(6): 1256-1261
- URL: https://www.wjgnet.com/1948-9366/full/v15/i6/1256.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v15.i6.1256
Small bowel diverticulum disease is a rare disease in clinical practice, with an incidence of approximately 5%. Clinically, small bowel diverticula can be divided into two subtypes depending on their pathogenesis: Congenital and acquired diverticula of the small intestine. These in turn include Meckel’s diverticulum (i.e., distal ileal diverticulum), duodenal diverticulum and jejunal diverticulum[1]. Patients with small bowel diverticulum disease are usually asymptomatic, and the lesions are mostly noticed during radiological examinations or laparotomy for other abdominal disorders. Laparotomy is usually the gold standard for confirming small bowel diverticulum[2]. Symptoms such as bloating, epigastric pain, and nausea are sometimes present but ignored because they are not specific. When complications occur, patients may also develop diverticulitis, bleeding, stone formation, and secondary ileus[3].
Epigastric pain intercropping for 5 d.
This was a 78-year-old male patient with no obvious cause of epigastric pain, accompanied by sweating, occasional pantothenic acid belching, no nausea and vomiting, stomachache, irregular stools, and no melena. He visited Jiangsu Provincial Hospital of Traditional Chinese Medicine on September 22, 2022, and did not have any weight loss, changes in bowel habits, fever, or other symptoms in the past six months.
The patient had a history of appendix surgery and type 2 diabetes, and he had no history of a colonic diverticulum.
The patient had no relevant personal or family history.
On September 23, 2022, the patient had left upper quadrant tenderness, no palpable mass, no rebound tenderness, or other signs of peritonitis. A digital rectal examination found no abnormal symptoms.
The patient’s hypersensitive C-reactive protein level was 2.87 mg/L, and the leukocyte count was 15.16 × 109/L.
On September 22, 2022, computed tomography (CT) of the whole abdomen showed that he possibly had a left upper quadrant jejunal intussusception (Figure 1A). On September 23, 2022, CT showed left upper quadrant jejunal intussusception and mild ischemic changes in the intestinal wall (Figure 1B).
Small bowel diverticulum with a fecalith causing intestinal obstruction.
On September 23, 2022, laparoscopic exploration revealed no obvious exudation in the abdominal cavity, slight edema of the left upper abdominal intestinal loop, a jejunal mass near Qu’s ligament, with a size of approximately 7 cm × 8 cm, local slight activity; the diverticulum was 10 cm distally; and there was obvious local small intestinal dilation edema. Jejunectomy anastomosis: A median incision was made into the upper abdomen, approximately 8 cm long, and the skin, white line, and peritoneum were separated to enter into the peritoneum layer by layer. The incision was placed into an incision protective sleeve. Breaking of the adhesions around the beginning of Qucker’s ligament, separation and severing of the mesenteric vessels around the mass, ligation, and disconnection of the mesangium were performed to cut the small intestine approximately 15 cm below the lesion. After the small intestine was severed at Treitz’s ligament, the stapler nail seat was placed, and jejunal side anastomosis was performed with a 25-tube stapler. The patency of the anastomosis was checked. A 4-0 Vijo line was used to strengthen the anastomosis and close the mesangium. Jejunocentesis catheterization was performed 30 cm below the anastomotic port; jejunostomy was performed, 3-0 sutures were used to suture the intestinal wall to form a 1 cm tunnel, and the sutures were suspended to the abdominal wall, allowing the jejunostomy tube to exit from the left upper quadrant.
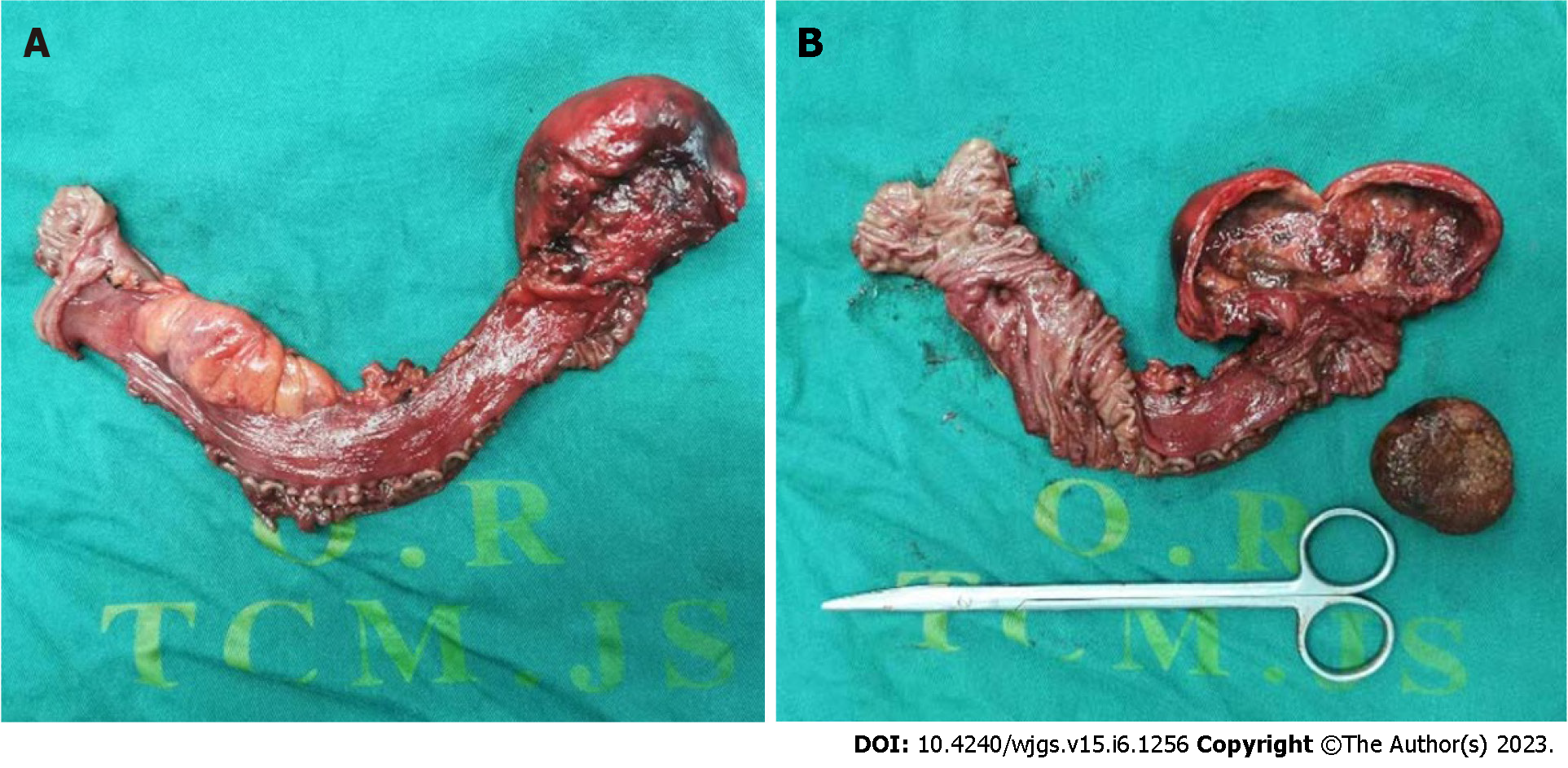
After parenteral nutrition support was given for a short amount of time after surgery, the fluid and enteral nutrition solution were pumped through the jejunostomy tube, and the patient was discharged after stable treatment. The jejunostomy tube was removed one month after surgery. The postoperative pathology results were as follows: Jejunectomy specimens: (1) There was a small intestinal diverticulum with chronic inflammation, full-thickness inflammatory ulcers, and intestinal wall necrosis in some areas; (2) the quality of hard objects is consistent with stone changes; and (3) the resection margin on both sides shows chronic inflammation of mucosal tissue (Figure 2).
Acquired jejunal diverticulum is a pseudodiverticulum that invades only the mucosal layer and the submucosal layer, and it was first reported by de Bree et al[4]. It is more common in people in their sixties and seventies, and is seen more in men than in women. As in this patient, small bowel diverticula are usually multiple, and these diverticula provide a pocket for the stagnation of intestinal contents, leading to the formation of intestinal stones. Intestinal stones are rare and can be divided into true and pseudo stones according to their quality. Pseudo stones are formed by the accumulation of feces, fruits, and other exotic substances, while true stones are deposited by substances that digest the chyle layer.
The causes of intestinal stones are more complex and closely related to the patient’s eating habits. Related studies have shown that the intake of persimmons, dates, hawthorn and other foods rich in tannic acid is an important cause of inducing fecalith intestinal obstruction; tannic acid and gastric acid form colloidal substances; and protein to form tannic acid protein can be mixed with food residues to form intestinal stones[5]. This patient had a history of diabetes, which can lead to autonomic lesions and reduce gastric emptying function, and it is also one of the important causes of intestinal fecalith formation[6]. In terms of diagnosis, patients with small bowel diverticular disease are usually asymptomatic. When complications occur, patients also show manifestations associated with complications. Diagnosis can be aided by ultrasound, CT, or small bowel enema[3]. Currently, contrast-enhanced CT remains the first choice for the diagnosis of small bowel diverticulum[7], but the diverticular presentation on CT is difficult to distinguish from the intestinal tube with fluid accumulation. Intestinal stones usually appear on CT as round or oval clumps at the site of obstruction and contain mottled gas that appears to be specific. However, small bowel stones can also present as gas-free soft tissue masses that are difficult to distinguish from intussusception[3]. In this patient, chronic fecalith formation was caused by small intestinal diverticula, and the internal fecalith shadow and local loop edema made the CT imaging findings similar to those of intussusception. During intraoperative laparotomy, we consider that small intestinal tumors such as stromal tumors are more likely to be observed during a comprehensive operation due to local chronic inflammatory adhesions, edema of local intestinal loops, and solid manifestations of internal fecal stone filling. It was not until the surgical specimen was dissected ex vivo that the patient’s mass was found to be a small intestinal diverticulum with local fecalith formation in the small intestinal lumen. The rarity and specificity of this case led to a misdiagnosis before surgery.
For treatment, patients with small bowel diverticular disease do not require any treatment in the absence of clinical symptoms, and conservative treatment should be considered when accompanied by diverticulitis. If conservative treatment is ineffective or accompanied by other complications, such as bleeding, obstruction, and perforation, surgery should be performed immediately. Small intestinal stones can be crushed and squeezed into areas of the intestine distal to the cecum so that they can pass naturally[8]. CT showed ischemic changes in the intestinal wall, and the patient required surgery to prevent bowel syndrome[9].
Due to the advanced age of the patient, long-term parenteral nutrition support is associated with complications such as catheter infection, liver damage, and metabolic disorders[10]. Moreover, advanced age is also a high-risk factor for anastomotic fistula, and the mortality rate of high anastomotic fistula is 21.4%[11]. Therefore, based on previous experience and Ojo et al[12] systematic reviews, enteral IVF is safe and effective in improving the quality of life of patients. We placed a trans jejunostomy tube during surgery to pump fluid and enteral nutrition solution after surgery. As a result, patients can discontinue parenteral nutrition support as soon as possible and obtain a better and faster recovery after surgery.
In summary, the small intestinal diverticulum of this patient was accompanied by fecalith intestinal obstruction due to the special quality and size of the fecaliths. CT imaging and physical examination could not fully determine the quality, resulting in a misdiagnosis, and the diagnosis was not confirmed until after the autopsy specimen examination. In addition, the patient discontinued enteral nutrition support as soon as possible after surgery, and the method of pumping the nutrient solution through the jejunostomy tube was safer than long-term enteral nutrition support. Such means could be used as a common surgical method for elderly patients.
Clinically, small bowel diverticulum is difficult to distinguish from jejunal intussusception, and early diagnosis and surgery are the main means of appropriate management.
Thanks to Professor Jiang Zhi-Wei for his perioperative guidance on the use of Enhanced Recovery After Surgery, and Professor Liu Xin-Xin for his precise surgery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Haddadi S, Algeria; Litvin A, Russia S-Editor: Chen YL L-Editor: A P-Editor: Guo X
| 1. | Zhao L, Lu W, Sun Y, Liang J, Feng S, Shi Y, Wu Q, Wang J, Wu K. Small intestinal diverticulum with bleeding: Case report and literature review. Medicine (Baltimore). 2018;97:e9871. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Makris K, Tsiotos GG, Stafyla V, Sakorafas GH. Small intestinal nonmeckelian diverticulosis. J Clin Gastroenterol. 2009;43:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Rangan V, Lamont JT. Small Bowel Diverticulosis: Pathogenesis, Clinical Management, and New Concepts. Curr Gastroenterol Rep. 2020;22:4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | de Bree E, Grammatikakis J, Christodoulakis M, Tsiftsis D. The clinical significance of acquired jejunoileal diverticula. Am J Gastroenterol. 1998;93:2523-2528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 56] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Kim JH, Ha HK, Sohn MJ, Kim AY, Kim TK, Kim PN, Lee MG, Myung SJ, Yang SK, Jung HY, Kim JH. CT findings of phytobezoar associated with small bowel obstruction. Eur Radiol. 2003;13:299-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Albert JG, Lübbert C, Surow A, Zeuzem S. [Small bowel diverticula - unknown disease]. Z Gastroenterol. 2009;47:674-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Lebert P, Ernst O, Zins M. Acquired diverticular disease of the jejunum and ileum: imaging features and pitfalls. Abdom Radiol (NY). 2019;44:1734-1743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Kornprat P, Langner C, Mischinger HJ. Enterolithiasis in jejunal diverticulosis, a rare cause of obstruction of the small intestine: a case report. Wien Klin Wochenschr. 2005;117:297-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Massironi S, Cavalcoli F, Rausa E, Invernizzi P, Braga M, Vecchi M. Understanding short bowel syndrome: Current status and future perspectives. Dig Liver Dis. 2020;52:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 10. | Abunnaja S, Cuviello A, Sanchez JA. Enteral and parenteral nutrition in the perioperative period: state of the art. Nutrients. 2013;5:608-623. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 11. | Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 662] [Cited by in RCA: 751] [Article Influence: 41.7] [Reference Citation Analysis (0)] |
| 12. | Ojo O, Keaveney E, Wang XH, Feng P. The Effect of Enteral Tube Feeding on Patients' Health-Related Quality of Life: A Systematic Review. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |